Understanding Acute Myeloid Leukemia (AML) Subtypes
Explore the evolving classification, genetic basis, and prognosis of acute myeloid leukemia (AML) subtypes for improved diagnosis and treatment.
Acute Myeloid Leukemia (AML) Subtypes: A Comprehensive Guide
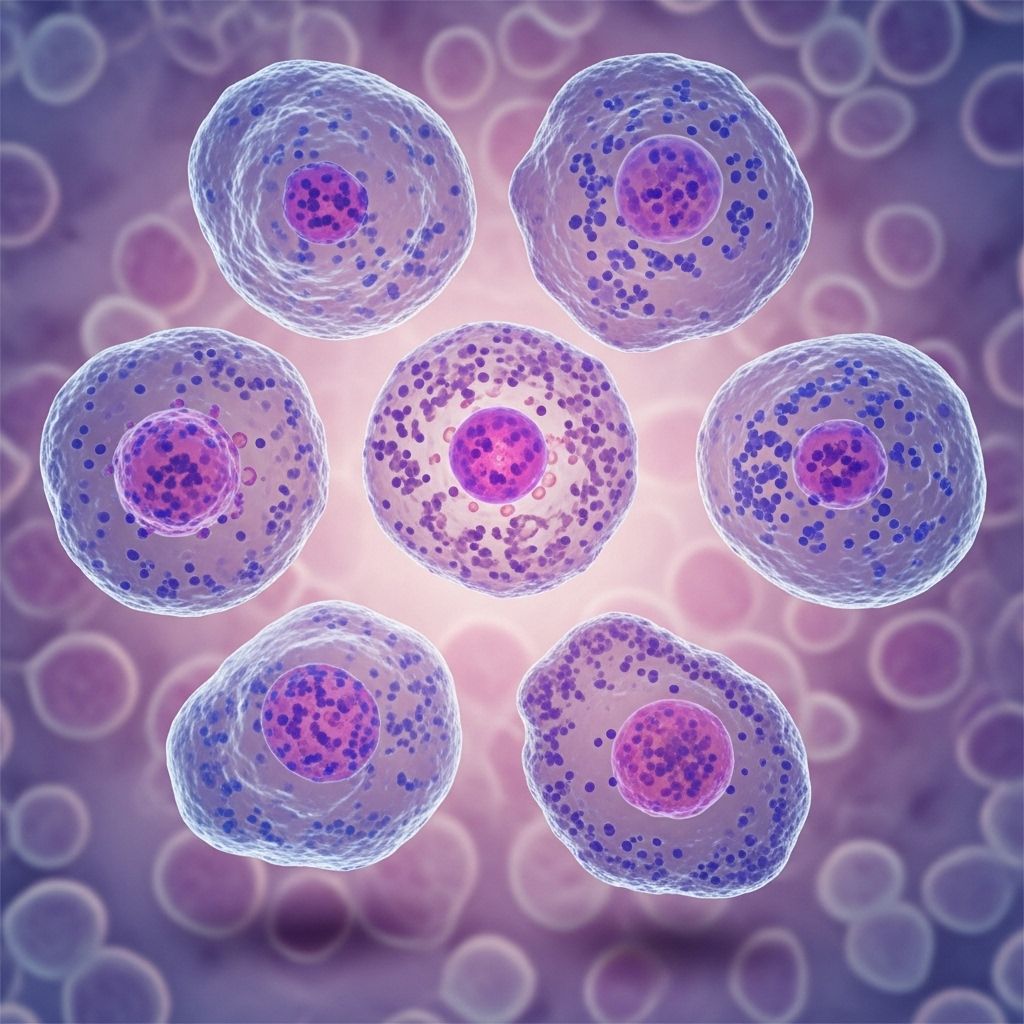
Acute myeloid leukemia (AML) is a complex and aggressive form of blood cancer, characterized by the rapid growth of abnormal white blood cells in the bone marrow and blood. Understanding the different AML subtypes is crucial because each carries unique genetic and clinical features that directly impact prognosis, treatment strategies, and patient outcomes.
Why Are AML Subtypes Important?
The classification of AML into subtypes helps healthcare professionals:
- Determine the most effective treatment plan.
- Estimate prognosis and survival rates for each patient.
- Monitor and understand the disease progression.
- Facilitate communication among specialists and research groups.
Early Classification: The FAB System
The French-American-British (FAB) system, introduced in the 1970s, was the first attempt to systematically classify AML. FAB classified AML into eight subtypes, M0 through M7, based mainly on the appearance (morphology) of leukemia cells and their level of maturation under a microscope:
- M0: Undifferentiated AML
- M1: AML with minimal maturation
- M2: AML with maturation
- M3: Acute promyelocytic leukemia (APL)
- M4: Acute myelomonocytic leukemia
- M5: Acute monocytic leukemia
- M6: Acute erythroid leukemia
- M7: Acute megakaryoblastic leukemia
While the FAB system was groundbreaking, it did not account for many increasingly important genetic and molecular factors. Over time, a more nuanced classification system was needed.
The Modern Standard: WHO Classification of AML
The World Health Organization (WHO) classification, last substantially updated in 2016 and further refined in 2022, organizes AML subtypes using not only cell morphology but also genetic, molecular, and clinical information. According to the most recent WHO standards, AML is divided into major groups:
- AML with recurrent genetic abnormalities
- AML with myelodysplasia-related changes
- Therapy-related myeloid neoplasms
- AML, not otherwise specified (NOS)
- Myeloid sarcoma
- Myeloid proliferations related to Down syndrome
The shift toward genetic and cytogenetic criteria allows for more precise categorization and enables clinicians to personalize care.
AML with Recurrent Genetic Abnormalities
Some of the most clinically relevant AML subtypes are defined by recurrent genetic changes. These gene mutations and chromosomal rearrangements strongly influence disease behavior and treatment responses. Key subtypes include:
- AML with t(8;21)(q22;q22.1)/RUNX1-RUNX1T1
- AML with inv(16)(p13.1q22) or t(16;16)(p13.1;q22)/CBFB-MYH11
- Acute promyelocytic leukemia (APL) with t(15;17)(q22;q12)/PML-RARA
- AML with t(9;11)(p21.3;q23.3)/MLLT3-KMT2A
- AML with t(6;9)(p23;q24)/DEK-NUP214
- AML with inv(3)(q21.3q26.2) or t(3;3)(q21.3;q26.2)/GATA2, MECOM
- AML (megakaryoblastic) with t(1;22)(p13.3;q13.3)/RBM15-MKL1
- AML with mutated NPM1
- AML with mutated CEBPA
- AML with t(9;22)(q34.1;q11.2)/BCR::ABL1
These genetic alterations are found through specialized tests and can dictate specific targeted therapies.
AML with Myelodysplasia-Related Changes
This AML subtype occurs in patients with a history of myelodysplastic syndromes (MDS) or who have certain chromosomal abnormalities previously linked to MDS. These cases generally have a poorer prognosis and may require different therapeutic approaches.
Therapy-Related Myeloid Neoplasms
Also known as therapy-related AML (t-AML), this form arises after prior chemotherapy, radiation, or toxin exposure (such as benzene). Therapy-related AML often shows complex genetic changes, making it especially challenging to treat.
AML Not Otherwise Specified (NOS)
When an AML case does not fit into any of the categories above, it is classified as “not otherwise specified.” This group mirrors the older morphologic FAB subtypes, such as:
- AML with minimal differentiation
- AML without maturation
- AML with maturation
- Acute myelomonocytic leukemia
- Acute monoblastic/monocytic leukemia
- Pure erythroid leukemia
- Acute megakaryoblastic leukemia
- Acute basophilic leukemia
- Acute panmyelosis with myelofibrosis
How Are AML Subtypes Determined?
The classification of AML subtypes uses a combination of methods, including:
- Microscopy: Assessing the appearance and maturation of abnormal cells.
- Immunophenotyping: Detecting specific proteins on the cell surface.
- Cytogenetic testing: Identifying chromosomal abnormalities.
- Molecular genetic testing: Analyzing DNA for mutations such as NPM1, CEBPA, or FLT3.
Factors That Influence Subtype Classification
- Developmental stage of the leukemia cells at diagnosis
- Proteins expressed on the cell surface
- Degree of difference between leukemia cells and normal cells (dysplasia)
- Underlying genetic abnormalities
AML Origins: De Novo, Secondary, and Therapy-Related
Besides genetic and morphologic features, AML can be categorized by origin:
- De novo AML: Arises spontaneously, with no prior history of blood or bone marrow disorders or known risk factors.
- Secondary AML (s-AML): Evolves from pre-existing bone marrow diseases such as MDS, myeloproliferative neoplasms (MPNs), or other blood cancers.
- Therapy-related AML (t-AML): Develops as a result of previous exposure to chemotherapy, radiation, or toxic substances.
Knowing the AML’s origin provides key information about its possible behavior and helps guide prognosis and treatment.
The 2022 ELN Guidelines: The Latest in AML Classification
The European LeukemiaNet (ELN) 2022 guidelines are now the benchmark for AML classification. Notable updates include:
- A lower blast threshold (now 10% for some genetic subtypes) to define AML presence in the blood or bone marrow.
- Newly defined AML types with specific genetic mutations, including in-frame bZIP-mutated CEBPA and t(9;22)/BCR::ABL1.
- Expansion of the category of AML with recurrent genetic abnormalities.
These advancements reflect a trend toward precision medicine, using highly specific genetic data to identify optimal treatments for individual patients.
Comparison Table: FAB vs. WHO AML Classification
| FAB Subtype | Cellular Feature | WHO Category |
|---|---|---|
| M0 | Undifferentiated | AML NOS (minimal differentiation) |
| M1 | Minimal maturation | AML NOS (without maturation) |
| M2 | With maturation | AML NOS (with maturation) |
| M3 | Acute promyelocytic (APL) | AML with PML-RARA |
| M4 | Myelomonocytic | Myelomonocytic leukemia |
| M5 | Monocytic | Monoblastic/monocytic leukemia |
| M6 | Erythroid | Pure erythroid leukemia |
| M7 | Megakaryocytic | Acute megakaryoblastic leukemia |
Prognosis and Personalized Treatment
Understanding AML subtypes is critical for predicting disease behavior and identifying optimal treatment strategies. Factors that influence prognosis include:
- The specific genetic mutations (some, like NPM1, are associated with better outcomes; others, like FLT3-ITD, with poorer).
- Patient age and overall health.
- Response to initial therapy.
- History of prior blood disorders or treatments.
New targeted drugs are being developed for particular mutations, increasing effectiveness while reducing side effects for some patients.
Frequently Asked Questions (FAQs) About AML Subtypes
Q: Why do AML subtypes matter for treatment and prognosis?
A: Different subtypes can respond very differently to therapies. Knowing a patient’s AML subtype allows doctors to select treatments that are most likely to be effective and anticipate potential complications.
Q: How are AML subtypes diagnosed?
A: Determining a subtype usually involves blood and bone marrow tests, microscopy, cytogenetics, and advanced molecular genetic sequencing to find chromosome and gene mutations.
Q: Are genetic abnormalities always present in AML?
A: Not every AML case has a known genetic abnormality, but most do. The discovery of new mutations is expanding the number of recognized subtypes and improving treatment personalization.
Q: What is the difference between de novo, secondary, and therapy-related AML?
A: De novo AML arises spontaneously, secondary AML develops from previous blood disorders, and therapy-related AML results from past chemotherapy, radiation, or toxin exposure.
Q: Where can patients find updated information about their AML subtype?
A: Patients can learn more by discussing directly with their hematologist or accessing credible resources such as the American Cancer Society, National Institutes of Health, and dedicated leukemia foundations.
Advances, Research, and Future Directions
Research on AML is rapidly advancing. Key trends include:
- Increasing use of genetic and molecular profiling for every AML diagnosis.
- Development of targeted therapies for specific mutations (e.g., FLT3, IDH1/2 inhibitors).
- Integration of new classification systems in international guidelines for customized patient care.
- Ongoing clinical trials exploring combinations of chemotherapy, immune therapies, and experimental agents for various subtypes.
Understanding your AML subtype is the first step in navigating the complexities of modern leukemia care. Patients are encouraged to work closely with their healthcare team and seek out reputable sources for the latest research and treatment updates.
Summary
The landscape of AML subtypes and classification has evolved from simple cell morphology to highly sophisticated genetic and molecular analysis. Better understanding of these subtypes means improved diagnosis, individualized treatment, and growing hope for those affected by acute myeloid leukemia.
References
- https://www.ncbi.nlm.nih.gov/books/NBK507875/
- https://healthtree.org/aml/community/articles/aml-types-and-classification
- https://www.cancer.org/cancer/types/acute-myeloid-leukemia/detection-diagnosis-staging/how-classified.html
- https://www.cancerresearchuk.org/about-cancer/acute-myeloid-leukaemia-aml/types-aml
- https://www.news-medical.net/health/Acute-Myeloid-Leukemia-Classification.aspx
- https://my.clevelandclinic.org/health/diseases/6212-acute-myeloid-leukemia-aml
Read full bio of Sneha Tete