Ulnar Nerve Entrapment: Causes, Symptoms, Diagnosis, and Treatment
Explore the essential facts, key signs, and modern treatment options for ulnar nerve entrapment, a common condition affecting the arm and hand.
Ulnar Nerve Entrapment: An In-Depth Overview
Ulnar nerve entrapment, commonly known as “cubital tunnel syndrome” when occurring at the elbow, is a prevalent neurological condition characterized by compression or irritation of the ulnar nerve as it travels from the neck down to the hand. The ulnar nerve helps control movement and sensation in the forearm, hand, and fingers, particularly the ring finger and pinky. This article provides a thorough exploration of the causes, risk factors, symptoms, diagnostic strategies, treatment options, prognosis, and prevention related to ulnar nerve entrapment.
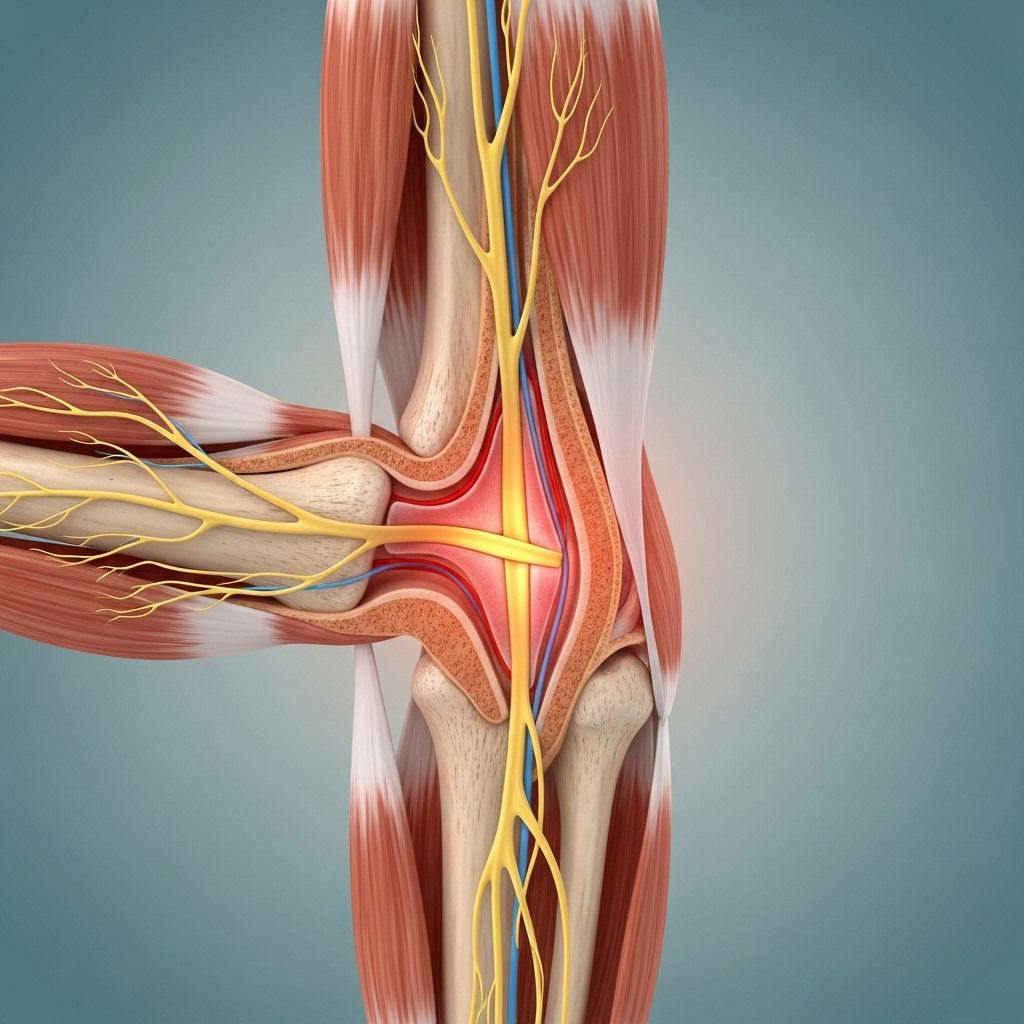
What Is the Ulnar Nerve?
The ulnar nerve is one of the three major nerves in the arm, originating from the brachial plexus in the neck and running down to the hand. It controls sensation in the pinky and part of the ring finger and powers numerous small muscles in the hand responsible for grip and fine motor control.
Commonly referred to as the “funny bone,” the ulnar nerve is especially vulnerable where it passes around the elbow and wrist, two areas prone to compression due to anatomical constraints and frequent movement.
What Is Ulnar Nerve Entrapment?
Ulnar nerve entrapment refers to the pinching or compression of the ulnar nerve, typically at the elbow (cubital tunnel syndrome) and less frequently at the wrist (Guyon canal syndrome). This condition can lead to sensory changes, motor deficits, and potentially permanent nerve damage if left untreated.
It is the second most common nerve entrapment in the upper extremity, after carpal tunnel syndrome.
Entrapment can also occur anywhere along the nerve’s course—shoulder, upper arm, forearm, and wrist.
Common Causes of Ulnar Nerve Entrapment
- Prolonged elbow bending: Frequently resting or leaning on an elbow, or sleeping with the arm bent
- Repetitive movement: Activities that require repeated bending or straightening of the elbow, such as sports or occupations involving manual labor
- Nerve instability: The ulnar nerve may slip in and out of its groove as the elbow flexes
- Fluid buildup or swelling: Can result from injury, inflammation, or systemic conditions like arthritis
- Direct trauma: A blow to the inner aspect of the elbow or wrist
- Bony abnormalities: Bone spurs, cysts, or post-fracture changes that contribute to compression
- Arthritis: Particularly rheumatoid arthritis in the elbow or wrist
- Pregnancy, diabetes, and other medical conditions: These can increase risk due to altered tissue swelling or nerve vulnerability
Main Sites of Entrapment
| Location | Name | Common Features |
|---|---|---|
| Elbow | Cubital Tunnel Syndrome | Numbness/tingling worse with elbow flexion |
| Wrist | Guyon Canal Syndrome | Numbness/weakness of ring/pinky fingers |
| Forearm | Between Wrist and Elbow | Rare, can occur due to trauma or anatomical variants |
| Upper Arm | Between Shoulder and Elbow | Least common, may result from compression or inflammation |
Common Symptoms of Ulnar Nerve Entrapment
- Numbness and tingling: Typically in the ring finger and pinky; symptoms tend to be intermittent, often worse at night or after elbow bending
- Pain or tenderness: Along the inner side of the elbow or wrist, sometimes radiating up and down the arm
- Weak grip strength: Difficulty gripping objects firmly
- Muscle weakness: In advanced cases, wasted hand muscles especially those between the thumb and forefinger (the intrinsic hand muscles)
- Clumsiness: Problems manipulating small objects, buttoning shirts, or performing fine motor activities
- Difficulty controlling movement: Loss of hand coordination and dexterity
If left untreated, symptoms can progress from intermittent numbness to persistent weakness and, eventually, to permanent nerve injury and muscle atrophy.
Risk Factors
- Occupations or activities requiring repetitive elbow bending or pressure
- Sports with frequent arm flexion (e.g., baseball, tennis)
- History of elbow or wrist injury
- Systemic conditions (diabetes, rheumatoid arthritis, pregnancy)
- Genetic predisposition to connective tissue disorders
When to See a Doctor
Consult a healthcare professional if you experience:
- Persistent numbness or tingling in your fingers
- Decreasing grip strength or hand coordination
- Pain interfering with work or daily routine
- Muscle wasting or visible hand deformities
Diagnosis of Ulnar Nerve Entrapment
Diagnosis typically involves:
- Detailed medical history and physical examination: Assessing symptom patterns, hand muscle strength, and elbow/wrist movement
- Provocative tests: Tapping over the nerve (Tinel’s sign) or sustained elbow flexion to reproduce symptoms
- Imaging studies:
- X-rays – Rule out bone spurs, fractures, or arthritis
- MRI/Ultrasound – Evaluate soft tissue, cysts, or swelling
- Electrodiagnostic testing: Nerve conduction studies and electromyography (EMG) measure nerve function, localize the site of compression, and evaluate severity
Prompt diagnosis is crucial; delayed recognition increases the risk for permanent nerve damage and may reduce chances of full recovery.
Treatment Options for Ulnar Nerve Entrapment
Treatment strategies depend on the severity and duration of symptoms and whether there is nerve injury or muscle wasting.
Conservative (Non-surgical) Treatments
- Activity modification: Avoiding prolonged elbow flexion, reducing repetitive movements, and adjusting work ergonomics
- Anti-inflammatory medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen help reduce swelling and discomfort
- Splints or braces: Worn at night to hold the elbow straight, prevent excessive bending, and reduce nerve irritation
- Physical therapy: Includes nerve gliding exercises to help the nerve move smoothly through its anatomical pathway, promote healing, and improve function
- Pain management: Sometimes tricyclic antidepressants or other medications for nerve pain
Typically, mild symptoms improve with these measures over a period of several weeks to months. If there is no improvement after three months or symptoms worsen, more advanced interventions may be considered.
Advanced and Surgical Treatments
- Peripheral percutaneous electrode placement: Minimally invasive technique to stimulate the nerve and relieve pain
- Ultrasound-guided injection or electrode placement: For more targeted therapy
- Surgical decompression:
- Cubital tunnel release: Releases compressed structures around the elbow
- Anterior transposition of the nerve: Moves the ulnar nerve to a less compressive position in the elbow
- Endoscopic or small-incision surgery: Modern techniques offer effective results with smaller scars and faster recovery
The goal of surgery is to relieve pressure, restore normal nerve function, and prevent further muscle loss. Most patients recover well, though the degree of improvement depends on the damage to the nerve prior to treatment.
Recovery and Prognosis
- Mild cases often resolve with conservative management in four weeks to three months
- Most surgical patients regain substantial function, but severe/prolonged entrapment may leave some residual weakness or numbness
- Physical therapy and nerve gliding exercises may be recommended after surgery for restoration of strength and range of motion
- Prognosis is best if the condition is recognized and treated early, before permanent muscle wasting or nerve injury occurs
Prevention Strategies
- Avoid prolonged elbow flexion; use armrests and pillows for support
- Take breaks from repetitive activities requiring elbow movement
- Use proper ergonomic positioning at work and during exercise
- Monitor and treat underlying medical conditions, such as diabetes or arthritis
Frequently Asked Questions (FAQs)
Q: What activities are most likely to lead to ulnar nerve entrapment?
A: Activities involving frequent elbow bending, prolonged pressure on the elbow (using computer desks, leaning on armrests), repetitive manual tasks, or sports with frequent arm flexion (tennis, baseball, cycling) are common contributors.
Q: How do I know if I need surgery?
A: Surgery is considered if symptoms persist for three months or more despite conservative measures, worsen noticeably, or there is evidence of muscle wasting and significant nerve dysfunction.
Q: Can ulnar nerve entrapment heal on its own?
A: Mild cases sometimes resolve spontaneously with avoidance of aggravating activities and modest lifestyle changes. However, ongoing symptoms require medical evaluation to prevent permanent damage.
Q: What exercises are helpful during recovery?
- Nerve gliding exercises: Guided movements that promote smooth nerve motion
- Range-of-motion exercises: To maintain flexibility in the arm and wrist
- Strengthening exercises: Focused on hand and forearm muscles, under guidance of a therapist
Q: Which doctor should I see for ulnar nerve entrapment?
A: Start with a primary care physician or orthopedic specialist. Neurologists, hand surgeons, or physical medicine doctors may be involved in diagnosis and treatment, especially for advanced cases.
Key Takeaways
- Ulnar nerve entrapment is a common cause of hand and arm neuropathy, typically occurring at the elbow or wrist
- Symptoms include numbness, tingling, and weakness in the ring and pinky fingers, often exacerbated by elbow bending
- Early diagnosis and treatment are crucial for best recovery outcomes
- Conservative management includes activity modification, medications, splints, and physical therapy
- Surgical options are effective for severe or persistent cases
- Preventive strategies focus on minimizing repetitive elbow stress and managing underlying conditions
FAQs About Ulnar Nerve Entrapment
Q: Is ulnar nerve entrapment permanent?
Early cases are rarely permanent, but if untreated and severe, muscle wasting and nerve damage may become irreversible. Timely medical attention can prevent long-term disability.
Q: Can I prevent ulnar nerve entrapment if I’ve had it before?
Yes. Use proper ergonomic support and avoid pressure on elbows. Regular stretching and strengthening may help, and preventive use of braces or splints during high-risk activities can reduce recurrence risk.
Q: How long does recovery take after surgery?
Recovery depends on the procedure and severity; most people recover within a few weeks to a few months. Your doctor will instruct you on gradual return to activity and exercises.
Further Resources
- American Academy of Orthopaedic Surgeons
- Hand Surgeons’ Society guidelines
- Physical therapy handouts for nerve glide exercises
- Patient support groups for neuropathy and musculoskeletal health
References
- https://www.hss.edu/health-library/conditions-and-treatments/list/ulnar-nerve-entrapment
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8207847/
- https://www.osmosis.org/answers/ulnar-nerve-entrapment
- https://www.medicalnewstoday.com/articles/318043
- https://my.clevelandclinic.org/health/diseases/22272-ulnar-nerve-entrapment
- https://www.healthline.com/health/lunar-nerve-entrapment
- https://www.uclahealth.org/medical-services/neurosurgery/conditions-treated/ulnar-nerve-entrapment
- https://www.youtube.com/watch?v=beKmfvOYtz4
Read full bio of medha deb












