Types and Stages of Heart Failure: Comprehensive Guide
Explore the many forms and progression stages of heart failure, their key characteristics, and recommended treatment strategies.
Types and Stages of Heart Failure: A Comprehensive Guide
Heart failure is a chronic condition affecting millions worldwide, marked by the heart’s inability to pump blood effectively to meet the body’s needs. Understanding the different types and stages of heart failure is essential for effective diagnosis, management, and lifestyle adjustment. This guide delves into the major forms of heart failure, their classification by function and progression, symptoms, diagnosis strategies, and common treatments.
What Is Heart Failure?
Heart failure occurs when the heart’s muscle cannot pump blood as well as it should. It does not mean the heart has stopped working; rather, it means its efficiency is impaired, resulting in symptoms like fatigue, swelling, and shortness of breath. Heart failure may affect one or both sides of the heart and varies in severity, type, and progression.
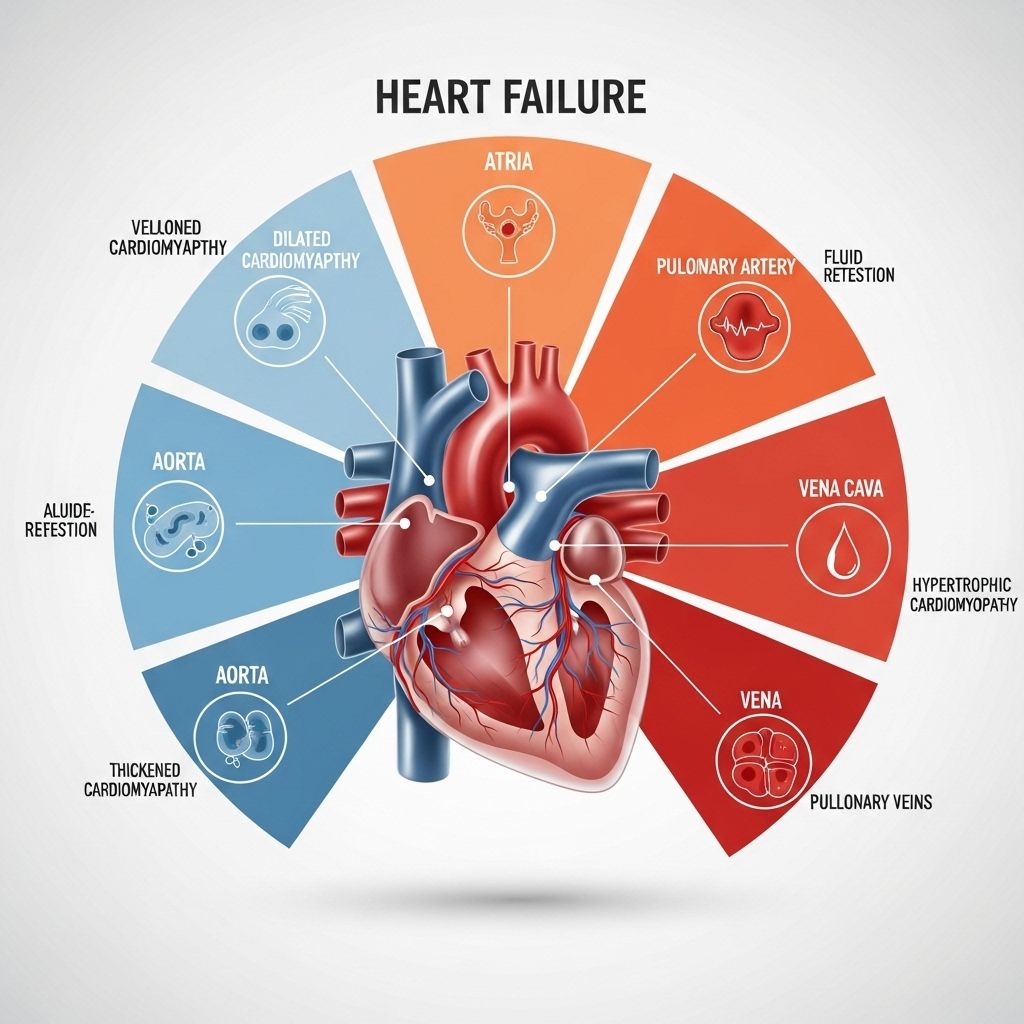
Types of Heart Failure
Heart failure is broadly categorized by the affected area of the heart and by how well the heart ejects blood. The major clinical types include:
- Left-sided heart failure
- Right-sided heart failure
- Systolic heart failure (HFrEF – reduced ejection fraction)
- Diastolic heart failure (HFpEF – preserved ejection fraction)
- Heart failure with mildly reduced ejection fraction (HFmrEF)
- Heart failure with improved ejection fraction
Left-Sided Heart Failure
Left-sided heart failure is the most common type, in which the left ventricle loses its power to pump blood efficiently. The left ventricle is crucial for distributing oxygen-rich blood to the body. Weakness here can cause a backup of blood into the lungs, resulting in characteristic symptoms:
- Shortness of breath (dyspnea)
- Fatigue
- Fluid retention in the lungs (pulmonary congestion)
- Persistent cough or wheezing, often with pink-tinged phlegm
Systolic vs. Diastolic Left-Sided Heart Failure
| Type | Description |
|---|---|
| Systolic (HFrEF) | The left ventricle muscle cannot contract vigorously, leading to a reduced ejection of blood (LVEF ≤40%). |
| Diastolic (HFpEF) | The ventricle contracts normally, but its ability to relax is impaired, preventing sufficient filling (LVEF ≥50%). |
| Mildly Reduced (HFmrEF) | Left ventricular ejection fraction is mildly reduced (LVEF 41–49%) with evidence of heart failure. |
LVEF (Left Ventricular Ejection Fraction) is used to measure the efficiency of the heart’s pumping; it’s a key diagnostic parameter for distinguishing between these types.
Right-Sided Heart Failure
Right-sided heart failure involves the right ventricle, responsible for pumping blood to the lungs. If the right ventricle is weakened, blood backs up into the body’s veins. Common causes include left-sided heart failure, pulmonary hypertension, and certain lung diseases.
- Swelling in the legs, ankles, and feet (peripheral edema)
- Abdominal swelling (ascites)
- Rapid weight gain due to fluid retention
- Distended neck veins (jugular venous distension)
Right-sided heart failure rarely occurs in isolation—it’s usually a consequence of advanced left-sided failure or pulmonary disorders.
Congestive Heart Failure (CHF)
The term ‘congestive heart failure’ is often used to describe both right- and left-sided failure. It emphasizes fluid buildup (congestion) in tissues, particularly the lungs, abdomen, or extremities, causing swelling and discomfort. CHF is the classic presentation for many patients, with symptoms that may fluctuate in severity.
Other Functional Classifications of Heart Failure
- Acute vs. Chronic Heart Failure
- Acute heart failure arises suddenly, often requiring emergency intervention.
- Chronic heart failure develops gradually and may be managed over the long term.
- Compensated vs. Decompensated Heart Failure
- Compensated: Heart failure is present but the body adapts, minimising symptoms.
- Decompensated: Adaptive mechanisms fail, symptoms worsen, and hospitalization may be necessary.
Recognizing the symptoms of congestive heart failure can lead to timely and effective interventions. For a comprehensive look at early signs, diagnosis, and treatment options, be sure to read our thorough guide on congestive heart failure symptoms. This resource can help you navigate your path to better heart health.
Stages of Heart Failure (ACC/AHA Classification)
The progressive nature of heart failure is classified by the American College of Cardiology/American Heart Association (ACC/AHA) into four main stages, denoted A to D:
- Stage A: At Risk
- No symptoms or structural cardiovascular changes, but the presence of risk factors.
- Common risk factors: hypertension, diabetes, coronary artery disease, obesity, metabolic syndrome, family history, genetic variants, or exposure to cardiotoxic medications.
- Stage B: Pre-Heart Failure
- No symptoms, but there are subtle changes in heart structure or function.
- May have abnormal echocardiograms or persistent elevation of biomarkers.
- Stage C: Symptomatic Heart Failure
- Patient has current or past symptoms of heart failure (such as fatigue, dyspnea, edema).
- Structural heart disease is present (e.g., reduced ejection fraction, faulty valves).
- Stage D: Advanced Heart Failure
- Marked symptoms at rest or with minimal activity.
- Frequent hospitalizations and poor response to standard therapies.
| Stage | Description | Example Patient Profile |
|---|---|---|
| A | At risk, no symptoms or structural changes | Person with hypertension and diabetes |
| B | Pre-heart failure (structural changes, no symptoms) | Person with abnormal echocardiogram but no symptoms |
| C | Symptomatic heart failure | Individual with heart failure symptoms and reduced ejection fraction |
| D | Advanced heart failure (severe symptoms, repeated hospitalizations) | Person experiencing breathlessness even at rest despite treatment |
Heart Failure Symptom Classes (NYHA Functional Classification)
For patients with symptomatic heart failure (mostly stage C and D), severity is further measured by the New York Heart Association (NYHA) functional classes, which relate to physical activity limitations:
| NYHA Class | Symptom Profile |
|---|---|
| I | No symptoms with ordinary activity; no limitation. |
| II | Slight limitation; comfortable at rest, but usual activity causes symptoms (fatigue, dyspnea, palpitations). |
| III | Marked limitation; comfortable at rest, minimal activity causes symptoms. |
| IV | Symptoms occur even at rest; any activity increases discomfort. |
- NYHA class is dynamic and may change with treatment.
- Helps guide treatment approaches and prognosis discussions.
Causes of Heart Failure
Many conditions can weaken or damage the heart, leading to heart failure. Common causes include:
- Coronary artery disease (blockages in heart arteries)
- High blood pressure (hypertension)
- Heart valve diseases (e.g., mitral or aortic valve insufficiency)
- Cardiomyopathy (diseases affecting heart muscle)
- Arrhythmias (irregular heart rhythms)
- Congenital heart defects
- Other chronic conditions (diabetes, obesity, renal failure)
- Certain medications or toxins
Symptoms of Heart Failure
Symptoms can develop rapidly (acute heart failure) or over time (chronic heart failure). They may differ depending on the underlying type. Key symptoms include:
- Shortness of breath (especially on exertion or lying flat)
- Swelling (edema) in the legs, ankles, and abdomen
- Unexplained fatigue or weakness
- Rapid or irregular heartbeat
- Persistent cough or wheezing
- Weight gain from fluid retention
- Difficulty exercising or reduced exercise tolerance
Diagnosis of Heart Failure
Diagnosing heart failure involves assessing symptoms, medical history, a physical exam, and a range of tests:
- Echocardiogram: Measures ejection fraction, structure, and function.
- Electrocardiogram (ECG): Detects abnormal rhythms or heart attack aftermath.
- Blood tests: Assess kidney/liver function and cardiac biomarkers (BNP, NT-proBNP).
- Chest X-ray: Identifies heart enlargement or fluid in lungs.
- Stress tests and cardiac MRI: Evaluate heart performance under exertion and detailed structure.
Additional diagnostic procedures may be necessary to distinguish heart failure from other similar conditions (valvular heart disease, pulmonary embolism, chronic kidney disease).
Treatment and Management
Heart failure treatment depends on type, stage, and severity, aiming to relieve symptoms, improve quality of life, and slow disease progression. Common strategies include:
- Lifestyle modifications:
- Low-sodium diet
- Fluid management
- Regular physical activity (as tolerated)
- Weight management and smoking cessation
- Medications:
- ACE inhibitors, ARBs, beta-blockers
- Diuretics (manage swelling and fluid)
- Aldosterone antagonists
- Heart-specific medications (e.g., sacubitril/valsartan)
- Devices and Surgery:
- Implantable cardioverter-defibrillator (ICD)
- Cardiac resynchronization therapy (CRT)
- Heart valve repair/replacement
- Left ventricular assist device (LVAD)
- Heart transplant (in advanced cases)
Treatment guidelines are tailored to the stage and type of heart failure, with a multidisciplinary approach often required for advanced cases (stage D).
Living with Heart Failure
With appropriate medical and lifestyle interventions, many individuals can manage heart failure successfully. Support systems, cardiac rehabilitation, and regular monitoring are fundamental components of long-term care. Regular follow-up ensures adjustments to therapy as disease status changes.
Frequently Asked Questions (FAQs)
What is the difference between systolic and diastolic heart failure?
Systolic heart failure (HFrEF) means the heart muscle can’t contract effectively, leading to less blood pumped out. Diastolic heart failure (HFpEF) means the heart contracts normally but doesn’t fill adequately due to stiffness.
How are heart failure stages determined?
Stages (A-D) are based on risk factors, heart structure and function, symptom presence, and disease progression. Early stages have no symptoms, while advanced stages involve marked symptoms and impaired quality of life.
Can heart failure be cured?
Heart failure is usually a chronic, lifelong condition. However, with early intervention and proper management, symptoms can be controlled, and progression slowed. Cure is rare except for cases amenable to surgery or transplantation.
How is ejection fraction measured and why is it important?
Ejection fraction is measured by echocardiogram and reflects the percentage of blood the left ventricle pumps out with each beat. It helps categorize heart failure and guide treatment.
Can people with heart failure live normal lives?
Yes. Many people with heart failure, especially in early stages, remain active and lead fulfilling lives with the right medical support and lifestyle changes.
References
- American Heart Association: Classes & Stages of Heart Failure
- NCBI StatPearls: Heart Failure (Congestive Heart Failure)
- The Cardiology Advisor: Congestive Heart Failure Classification
- Mayo Clinic: Heart failure – Diagnosis and Treatment
References
- https://www.thecardiologyadvisor.com/features/congestive-heart-failure-symptoms-stages-classification/
- https://www.heart.org/en/health-topics/heart-failure/what-is-heart-failure/classes-of-heart-failure
- https://www.ncbi.nlm.nih.gov/books/NBK430873/
- https://www.mayoclinic.org/diseases-conditions/heart-failure/diagnosis-treatment/drc-20373148
- https://www.heart.org/en/health-topics/heart-failure/what-is-heart-failure/types-of-heart-failure
- https://www.acc.org/Latest-in-Cardiology/Articles/2021/07/12/12/31/Universal-Definition-and-Classification-of-Heart-Failure
- https://hfsa.org/types-heart-failure-and-diagnosis
Read full bio of medha deb












