Types of Valvular Heart Disease: Understanding Causes, Symptoms, and Treatments
Comprehensive guide to valvular heart disease: covering causes, types, symptoms, treatment, and prevention.
Types of Valvular Heart Disease: Causes, Symptoms, Diagnosis, and Treatment
Valvular heart disease affects the valves of the heart, impacting the organ’s ability to circulate blood efficiently. These conditions can develop suddenly or progress slowly over time, and they encompass a range of disorders with varying seriousness. Understanding the types, underlying causes, warning signs, and treatment options is key to ensuring early detection and effective management.
What Is Valvular Heart Disease?
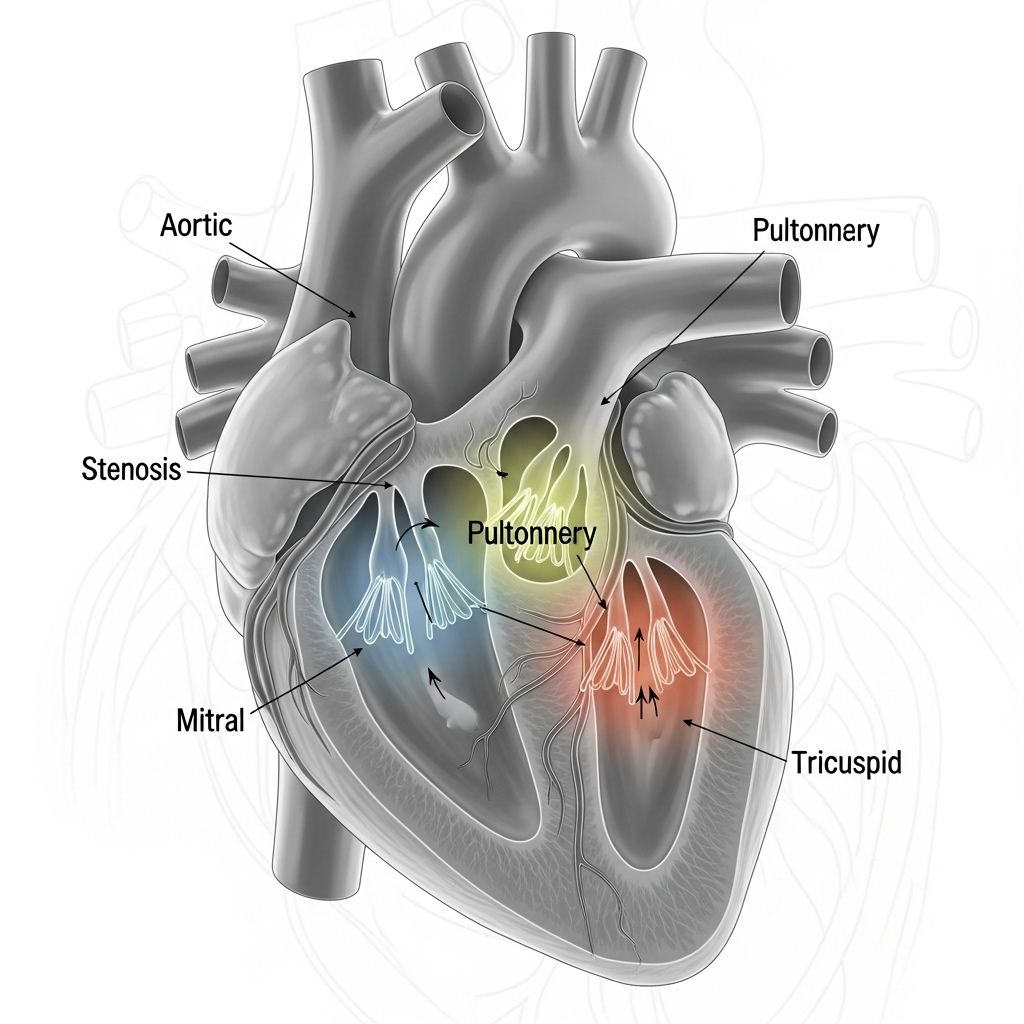
The heart contains four main valves—the aortic, mitral, tricuspid, and pulmonary valves—that are responsible for ensuring blood flows in the correct direction through the heart’s chambers. Valvular heart disease occurs when one or more of these valves malfunctions. Such malfunctions can lead to problems like leakage (regurgitation), narrowing (stenosis), or complete closure (atresia).
- Regurgitation: The valve does not close completely, resulting in blood leaking backward.
- Stenosis: The valve becomes narrowed or stiff, causing restricted blood flow.
- Atresia: The valve is missing or fails to form, blocking blood flow entirely.
Main Types of Valvular Heart Disease
Valvular heart disease generally falls into the following main types, classified according to the affected valve and the nature of the dysfunction:
- Aortic Valve Disease
- Aortic Stenosis: The aortic valve opening is narrowed, impeding blood flow from the left ventricle to the aorta.
- Aortic Regurgitation (Insufficiency): The valve does not close tightly, causing blood to flow backward into the left ventricle.
- Mitral Valve Disease
- Mitral Stenosis: The mitral valve narrows, limiting blood flow from the left atrium to the left ventricle.
- Mitral Regurgitation: Ineffective closure of the valve leads to backward flow of blood into the left atrium.
- Mitral Valve Prolapse: The valve’s flaps bulge back (prolapse) into the left atrium when the heart contracts, which can result in leaking.
Leaky heart valves, particularly the mitral valve, can lead to significant health risks. If you're experiencing symptoms or suspect you might be affected, discover essential information in our detailed article on Leaky Heart Valve Symptoms, Causes, and Treatment options that can help you take control of your health. - Tricuspid Valve Disease
- Tricuspid Stenosis: Narrowing between the right atrium and right ventricle, restricting blood flow.
- Tricuspid Regurgitation: Blood leaks backward into the right atrium due to an incompetent valve.
- Pulmonary Valve Disease
- Pulmonary Stenosis: Narrowing of the pulmonary valve restricts blood flow from the right ventricle to the lungs.
- Pulmonary Regurgitation: Backward flow of blood into the right ventricle during diastole.
- Congenital Valve Disease
- Present from birth, these defects include misshapen or fused valve leaflets, missing valves (atresia), and abnormal valve connections.
- Acquired Valve Disease
- Conditions that develop over time, often due to infections, rheumatic fever, or age-related changes.
Causes and Risk Factors
Valvular heart diseases result from a variety of causes, including structural abnormalities, infections, and lifestyle-related factors. Understanding these causes and associated risk factors can help guide prevention and early intervention.
- Congenital Defects: Some people are born with malformed valves, often detected during childhood or adolescence.
- Age-Related Degeneration: With aging, calcium buildup and tissue wear can stiffen or thicken valve leaflets.
- Rheumatic Fever: A complication of untreated strep throat can cause lasting valve damage, especially in developing countries.
- Endocarditis: Bacterial infections can damage heart valves, leading to regurgitation or stenosis.
- Calcium Deposits: Mineral deposits accumulate on the valve leaflets, particularly in the aortic valve, making them less flexible.
- Other Heart Diseases: Cardiomyopathy and hypertension may indirectly harm valves.
- Radiation Therapy: Previous chest radiation increases risk for valve problems.
- Autoimmune Disorders: Conditions like lupus can affect the heart valves.
Key risk factors include advanced age, history of rheumatic disease, high blood pressure, previous infections, certain genetic conditions, and a family history of heart disease.
Common Signs and Symptoms
Valvular heart disease may remain silent for years. Early symptoms are often subtle or mistaken for other conditions. As the condition progresses, warning signs become more noticeable:
- Shortness of breath, especially during exertion or when lying down
- Fatigue or weakness
- Swelling in the ankles, feet, or abdomen
- Irregular, rapid, or skipped heartbeats (arrhythmia)
- Chest pain or pressure
- Dizziness or fainting spells
- Heart murmur (distinctive sound heard via stethoscope during heartbeat)
Some symptoms develop quickly if valve problems arise suddenly, such as with endocarditis or valve rupture. Many signs and symptoms overlap with other types of heart disease, making professional evaluation essential.
How Is Valvular Heart Disease Diagnosed?
Early detection is crucial for effective treatment. Diagnosis usually involves a combination of the following:
- Physical Exam: A doctor listens for murmurs, clicks, or other abnormal heart sounds.
- Electrocardiogram (ECG): Records the heart’s electrical activity and rhythm.
- Echocardiogram: Uses ultrasound waves to create images of heart valves, chambers, and blood flow dynamics.
- Chest X-ray: Reveals heart enlargement or fluid in the lungs.
- Cardiac MRI or CT Scan: Provides detailed images for complex cases or pre-surgical planning.
- Cardiac Catheterization: A thin tube inserted into a blood vessel offers detailed pressure and chamber measurements and allows dye-assisted imaging.
Treatment Options for Valvular Heart Disease
Treatment depends on the type, severity, and progression of valve disease, and whether symptoms are present. The main approaches include:
- Medications
- Help control symptoms by reducing fluid buildup, lowering blood pressure, or slowing heart rate.
- May include diuretics, beta-blockers, ACE inhibitors, or anticoagulants to prevent clots.
- Lifestyle Modifications
- Adopting a heart-healthy diet rich in fruits, vegetables, and whole grains.
- Regular physical activity per medical clearance.
- Maintaining a healthy weight.
- Quitting smoking and limiting alcohol intake.
- Managing stress and attending follow-ups with healthcare providers.
- Procedures and Surgery
- Balloon Valvuloplasty: Inflation of a balloon within the valve to widen a narrowed opening, often for stenosis in children and some adults.
- Valve Repair: Surgery to restore proper valve functioning without replacement, often preferred in children and young adults.
- Valve Replacement: Severely damaged valves may be replaced with mechanical or biological (from animal or donated human tissue) prostheses. Mechanical valves require lifelong blood thinners.
- The choice between repair and replacement depends on the patient’s age, valve affected, degree of damage, and comorbidities.
Potential Complications
If left untreated or poorly managed, valvular heart disease can lead to serious, sometimes life-threatening, complications:
- Heart Failure: Inefficient pumping causes blood and fluid to back up in the lungs or other tissues.
- Arrhythmias: Irregular heartbeats, which can increase the risk of stroke.
- Stroke: Blood clots originating in malfunctioning heart chambers can travel to the brain.
- Blood Clots: May lead to pulmonary embolism or other organ damage.
- Sudden Cardiac Arrest or Death: Rare, but possible in severe, untreated cases.
- Infective Endocarditis: Damaged valves are more susceptible to infection.
Living With Valvular Heart Disease
Most people with valvular heart disease can lead active, fulfilling lives with proper treatment and regular medical care. Management strategies include:
- Regular medical checkups and heart imaging.
- Medications taken as prescribed.
- Monitoring for new or worsening symptoms.
- Prompt medical attention for infection or dental procedures (antibiotic prophylaxis may be recommended for some).
- Following heart-healthy lifestyle recommendations.
Prevention and Outlook
While not all forms are preventable (especially congenital valve abnormalities), steps below can lower risk for acquired valvular heart disease or help slow progression:
- Prompt treatment of strep throat to avoid rheumatic fever.
- Good dental hygiene to lower risk of bacterial endocarditis.
- Managing risk factors such as high blood pressure, obesity, and high cholesterol.
- Regular exercise and healthy eating.
- Regular heart screenings for those with family history or risk factors.
Outlook varies according to the severity of damage, affected valves, and response to treatment. Advances in diagnosis and therapy mean many people live symptom-free or experience a dramatic improvement in quality of life following intervention.
Comparison Table: Common Valve Disorders
| Valve Disorder | Location | Nature of Dysfunction | Common Symptoms |
|---|---|---|---|
| Aortic Stenosis | Aortic valve | Narrowing | Chest pain, fainting, heart murmur, shortness of breath |
| Mitral Regurgitation | Mitral valve | Leaking (backflow) | Fatigue, palpitations, shortness of breath |
| Tricuspid Stenosis | Tricuspid valve | Narrowing | Swelling, fatigue, abdominal discomfort |
| Pulmonary Regurgitation | Pulmonary valve | Leaking | Shortness of breath, fatigue, cyanosis (in severe cases) |
Frequently Asked Questions (FAQs)
What is the difference between valvular and non-valvular heart disease?
Valvular heart disease specifically affects the heart valves, leading to problems with blood flow through the heart. Non-valvular heart diseases involve other structures, such as blood vessels (coronary artery disease), heart muscle (cardiomyopathy), or rhythm disturbances (arrhythmias).
Can valve disease be reversed?
Structural damage to heart valves cannot usually be reversed, but treatments such as medications or surgery can alleviate symptoms and improve heart function. Early-stage problems, like mild regurgitation or stenosis, may stabilize with careful management.
How often should someone with valve disease see a doctor?
Follow-up frequency depends on the type and severity of the valve problem but usually involves annual or semiannual visits with periodic heart imaging to monitor changes.
Is surgery always necessary for valvular disease?
Many cases of mild or moderate disease are managed with medication and observation. Surgery or intervention is recommended for severe symptoms, worsening valve function, or the development of heart failure or other complications.
Are children affected by valvular heart disease?
Yes. Children can be born with congenital valve defects or acquire valve disease due to infections. Early diagnosis and appropriate management are important for best outcomes.
When to See a Doctor
Anyone experiencing symptoms like unexplained fatigue, chest pain, palpitations, or swelling should consult a healthcare professional. Timely diagnosis and treatment of valvular heart disease dramatically improves prognosis and quality of life.
If you have a known risk factor or family history of valve disease, regular screening and prompt treatment of infections (particularly strep throat or dental infections) are recommended.
References
- https://www.healthline.com/health/heart-disease
- https://www.medicalnewstoday.com/articles/237191
- https://www.chp.gov.hk/en/static/80035.html
- https://www.medicalnewstoday.com/articles/257484
- https://lifeprogram.org.au/health-hub/earlysignsofheartdiseaseinmen/
- https://www.healthline.com/health/heart-disease/how-heart-works
- https://www.healthline.com/health/video/how-to-prevent-heart-disease-according-to-a-cardiologist
- https://www.heart.org/en/health-topics/heart-attack/life-after-a-heart-attack/lifestyle-changes-for-heart-attack-prevention
- https://www.mayoclinic.org/diseases-conditions/heart-disease/in-depth/heart-healthy-diet/art-20047702
Read full bio of Sneha Tete












