Types of Stroke: Understanding Ischemic, Hemorrhagic, and More
Explore the causes, symptoms, and differences between the main types of stroke—including ischemic, hemorrhagic, TIA, and more.
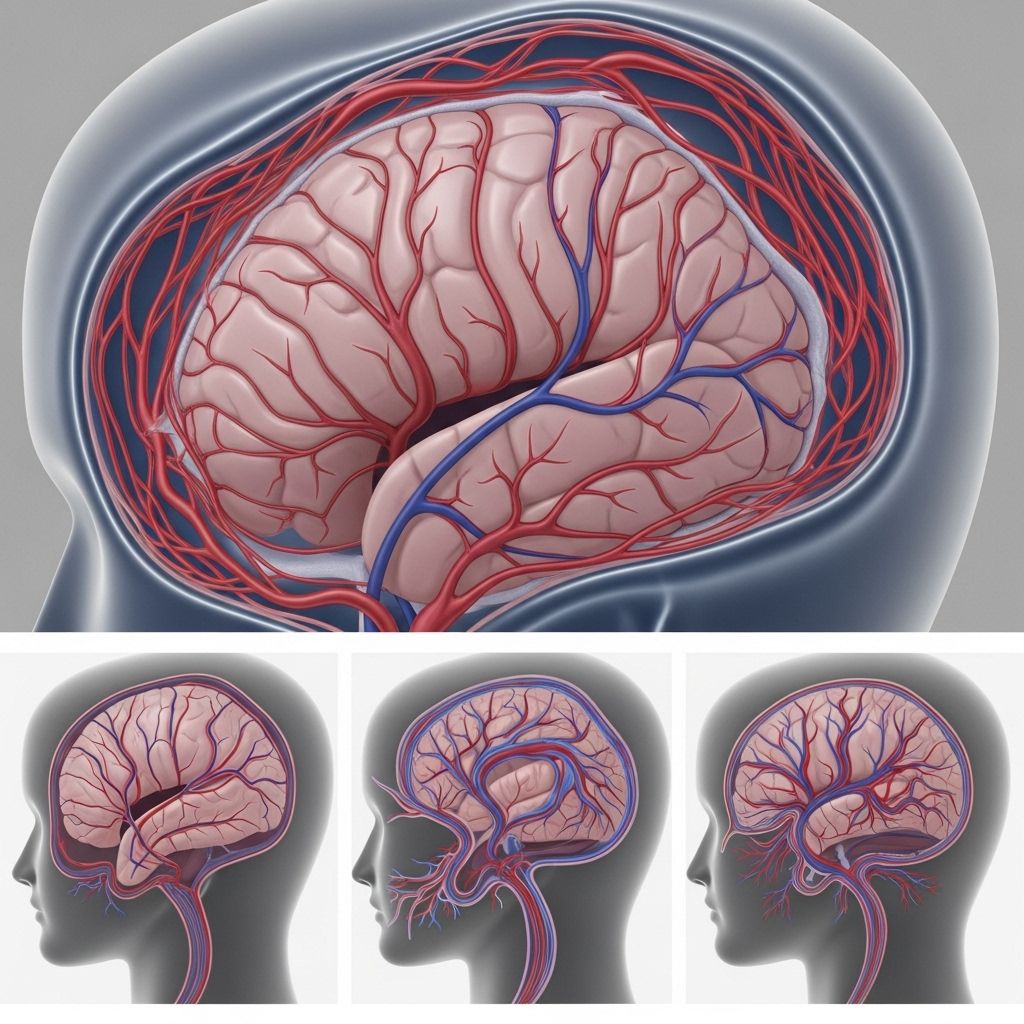
Strokes are sudden, life-threatening events that disrupt blood flow to the brain, resulting in damaged brain cells and varying degrees of neurological impairment. Understanding the types of stroke, their causes, and symptoms is critical for prompt diagnosis, effective treatment, and the best possible recovery. This comprehensive guide explores the main types of stroke, their distinctive features, underlying causes, and associated conditions.
What Is a Stroke?
A stroke, often termed a “brain attack,” occurs when the blood supply to a part of the brain is interrupted or significantly reduced. Without oxygen and nutrients, brain tissue begins to die within minutes. Strokes are medical emergencies and require immediate attention to minimize brain damage and complications.
- A stroke can cause emotional, physical, and cognitive difficulties, the severity of which depends on the type, location, and duration of the interruption to blood flow.
- The two primary mechanisms leading to stroke are either a blockage (ischemia) or bleeding (hemorrhage) within the brain.
Main Types of Stroke
Strokes are primarily classified based on what disrupts the blood flow—either a blockage (ischemic stroke) or a rupture in the blood vessel (hemorrhagic stroke). Each type has its own subtypes and unique features.
| Type of Stroke | Cause | Prevalence |
|---|---|---|
| Ischemic Stroke | Blockage of an artery supplying the brain | About 87% |
| Hemorrhagic Stroke | Rupture of a blood vessel in the brain | About 13% |
| Transient Ischemic Attack (TIA) | Temporary blockage, “mini-stroke” | Variable |
| Other Specialized Types* | Location-based or unexplained (e.g., cryptogenic) | Varies |
*Specialized types include cryptogenic and brainstem strokes, discussed in later sections.
Ischemic Stroke
Ischemic strokes are the most common, accounting for nearly 9 out of 10 cases.
- They occur when a blood clot blocks or narrows an artery leading to the brain, resulting in a significant reduction or cessation of blood flow that deprives brain cells of oxygen.
Causes of Ischemic Stroke
- Embolism: A clot forms elsewhere in the body (commonly in the heart) and travels to the brain, causing an embolic stroke.
- Thrombosis: A clot forms within a blood vessel in the brain, often due to the buildup of plaque (atherosclerosis), called a thrombotic stroke.
- Systemic Hypoperfusion: Severe drop in blood pressure resulting in decreased overall blood flow to the brain.
- Cerebral Venous Sinus Thrombosis: Rare clots form in the veins that drain the brain, causing venous congestion and tissue damage.
Symptoms: Sudden numbness or weakness (especially on one side of the body), confusion, trouble speaking, vision problems, difficulty walking, dizziness, or loss of balance.
Bamford (Oxford) Classification of Ischemic Stroke
The Bamford or Oxfordshire Community Stroke Project (OCSP) classification divides ischemic strokes by clinical symptoms and the area of the brain affected, without relying on imaging results.
- Total Anterior Circulation Stroke (TACS)
- Involves all three: unilateral weakness or sensory deficit of face, arm, and leg; homonymous hemianopia (visual field loss); and higher cerebral dysfunction (such as speech or cognitive problems).
- Typically associated with the most severe symptoms and highest early mortality rate.
- Partial Anterior Circulation Stroke (PACS)
- Any two of the TACS features or isolated higher cortical dysfunction.
- Less extensive and typically lower mortality than TACS.
- Lacunar Stroke (LACS)
- Small, deep infarcts affecting subcortical structures (e.g., basal ganglia, internal capsule).
- Key signs: pure motor or sensory deficit, sensorimotor deficit, ataxic hemiparesis, or dysarthria-clumsy hand syndrome.
- Usually does not affect higher cerebral function or cause visual field loss.
- Best prognosis among ischemic types.
- Posterior Circulation Stroke (POCS)
- Involves the brainstem, cerebellum, or occipital lobes.
- Symptoms: isolated visual field defect, brainstem signs (double vision, swallowing problems), or cerebellar ataxia (impaired coordination).
Hemorrhagic Stroke
Hemorrhagic strokes result from the rupture and subsequent bleeding of a blood vessel in the brain, quickly increasing pressure within the skull and leading to brain tissue injury.
- Less common than ischemic strokes, but generally more severe in outcomes and recovery prospects.
There are two major subtypes of hemorrhagic stroke:
- Intracerebral Hemorrhage (ICH): Bleeding occurs directly into brain tissue when a small artery within the brain bursts.
- Subarachnoid Hemorrhage (SAH): Bleeding occurs in the area between the brain and the surrounding thin tissues (subarachnoid space).
Causes of Hemorrhagic Stroke
- Uncontrolled high blood pressure (hypertension), the leading cause of both ICH and SAH.
- Brain aneurysms (weakened blood vessels that bulge and can rupture).
- Arteriovenous malformations (AVMs), congenital blood vessel abnormalities.
- Trauma, bleeding disorders, or use of blood-thinning medications.
Symptoms: Sudden, severe headache; weakness or numbness; difficulty speaking; vision changes; confusion; loss of coordination; nausea or vomiting; loss of consciousness.
Transient Ischemic Attack (TIA, or “Mini-Stroke”)
A transient ischemic attack (TIA) is a temporary episode of neurological symptoms caused by a brief lack of blood flow to the brain. Often called a “mini-stroke,” a TIA does not cause permanent damage but is a serious warning sign of significant stroke risk.
- Symptoms are similar to a stroke but typically resolve within minutes to a few hours—and always within 24 hours.
- Although the blockage and symptoms are temporary, TIAs indicate an underlying issue and require prompt evaluation.
- About one in three people who experience a TIA will later have a full-blown stroke, sometimes within days or weeks.
Other Types of Stroke
- Cryptogenic Stroke: A stroke for which no definite cause can be determined, despite an extensive medical evaluation. This accounts for up to one-third of ischemic strokes.
- Brainstem Stroke: Strokes occurring in the brainstem can affect basic bodily functions (breathing, heartbeat, swallowing) and may cause complex symptoms such as double vision, loss of coordination, locked-in syndrome, or coma.
- Silent Stroke: Strokes that do not cause noticeable symptoms but result in brain tissue damage detected on imaging or later in the presence of cognitive decline.
Comparing Stroke Types
| Stroke Type | Cause | Common Symptoms | Outcomes |
|---|---|---|---|
| Ischemic | Clot/blockage | Sudden weakness/numbness, speech/vision issues | Varies by location/severity; better if treated rapidly |
| Hemorrhagic | Blood vessel rupture/bleed | Severe headache, sudden neurological deficit, nausea/vomiting | Often more severe, higher risk of early mortality |
| TIA | Temporary blockage | Same symptoms as ischemic, but transient | No permanent deficit, but high risk for future stroke |
Recognizing Stroke Symptoms: Act F.A.S.T.
Every stroke requires rapid recognition and treatment. The sooner a stroke is identified, the greater the chances of recovering lost brain function. Use the F.A.S.T. acronym to recognize warning signs:
- Face Drooping: Sudden droop or asymmetry on one side of the face.
- Arm Weakness: Inability to lift or maintain arm strength on one side.
- Speech Difficulty: Slurred speech, confusion, or inability to speak clearly.
- Time to Call Emergency Services: If any of these symptoms appear, seek immediate medical attention.
Treatment Options by Stroke Type
Ischemic Stroke
- The main goal is restoring blood flow as quickly as possible.
- Medications such as tissue plasminogen activator (tPA) can dissolve clots if given within a specific time window.
- Endovascular procedures may involve mechanical removal of a clot using specialized devices.
Hemorrhagic Stroke
- The focus is controlling bleeding and reducing intracranial pressure.
- Treatment may include surgery to repair or remove abnormal blood vessels (like aneurysms or AVMs), or to drain collected blood.
- Medications may be used to manage blood pressure or reverse anticoagulant effects.
Transient Ischemic Attack (TIA)
- Management focuses on preventing a future, potentially larger, stroke.
- Lifestyle modifications, blood-thinning medications, and management of risk factors (such as atrial fibrillation, hypertension, diabetes, or high cholesterol) are key.
Stroke Risk Factors & Prevention
- High blood pressure (hypertension)
- Heart disease (especially atrial fibrillation)
- Diabetes mellitus
- High cholesterol (hyperlipidemia)
- Smoking and substance abuse
- Obesity, physical inactivity
- Family history or genetic predisposition
- Unhealthy diet and excessive alcohol intake
Prevention strategies such as maintaining a balanced diet, regular exercise, not smoking, and controlling blood pressure and other chronic conditions are essential in reducing stroke risk.
Frequently Asked Questions (FAQs)
Q: What is the difference between ischemic and hemorrhagic stroke?
A: Ischemic strokes are caused by a blockage (clot) in an artery supplying blood to the brain, while hemorrhagic strokes result from a ruptured blood vessel leading to bleeding within or around the brain.
Q: What is a TIA, and how serious is it?
A: A transient ischemic attack (TIA) is a “mini-stroke” where symptoms are temporary and resolve within 24 hours. It is a serious warning that a major stroke could occur soon and requires urgent medical assessment.
Q: Who is at the highest risk for stroke?
A: Anyone can have a stroke, but risk increases with age, high blood pressure, atrial fibrillation, diabetes, high cholesterol, smoking, and a family history of stroke.
Q: Can strokes be prevented?
A: Many strokes are preventable. Managing blood pressure, avoiding tobacco, staying physically active, eating a healthy diet, and controlling underlying medical conditions can significantly lower risk.
Q: What are the most important steps to take if stroke symptoms appear?
A: Call emergency services immediately. Time is critical—do not wait to see if symptoms resolve, as rapid treatment can reduce brain damage and improve outcomes.
Key Takeaways
- Strokes are mainly classified as ischemic (blockage) or hemorrhagic (bleeding), with ischemic being far more common.
- TIAs are “mini-strokes” offering a crucial opportunity to prevent a major stroke.
- Stroke symptoms often begin suddenly; immediate medical evaluation is vital.
- Many risk factors are modifiable—prevention and prompt care can save lives and brains.
References
- https://geekymedics.com/stroke-classification/
- https://www.brighamandwomens.org/neurosurgery/cerebrovascular/stroke/types
- https://pharmaceutical-journal.com/article/ld/stroke-classification-and-diagnosis
- https://www.stroke.org/en/about-stroke/types-of-stroke
- https://www.cdc.gov/stroke/about/index.html
- https://www.stroke.org.uk/stroke/types
- https://www.upstate.edu/stroke/about_stroke/types-of-stroke/index.php
Read full bio of medha deb












