Types of Retinal Detachment: Symptoms, Causes, and Treatment
Explore the main types of retinal detachment, their symptoms, causes, risk factors, diagnosis, and essential treatment options for preserving vision.
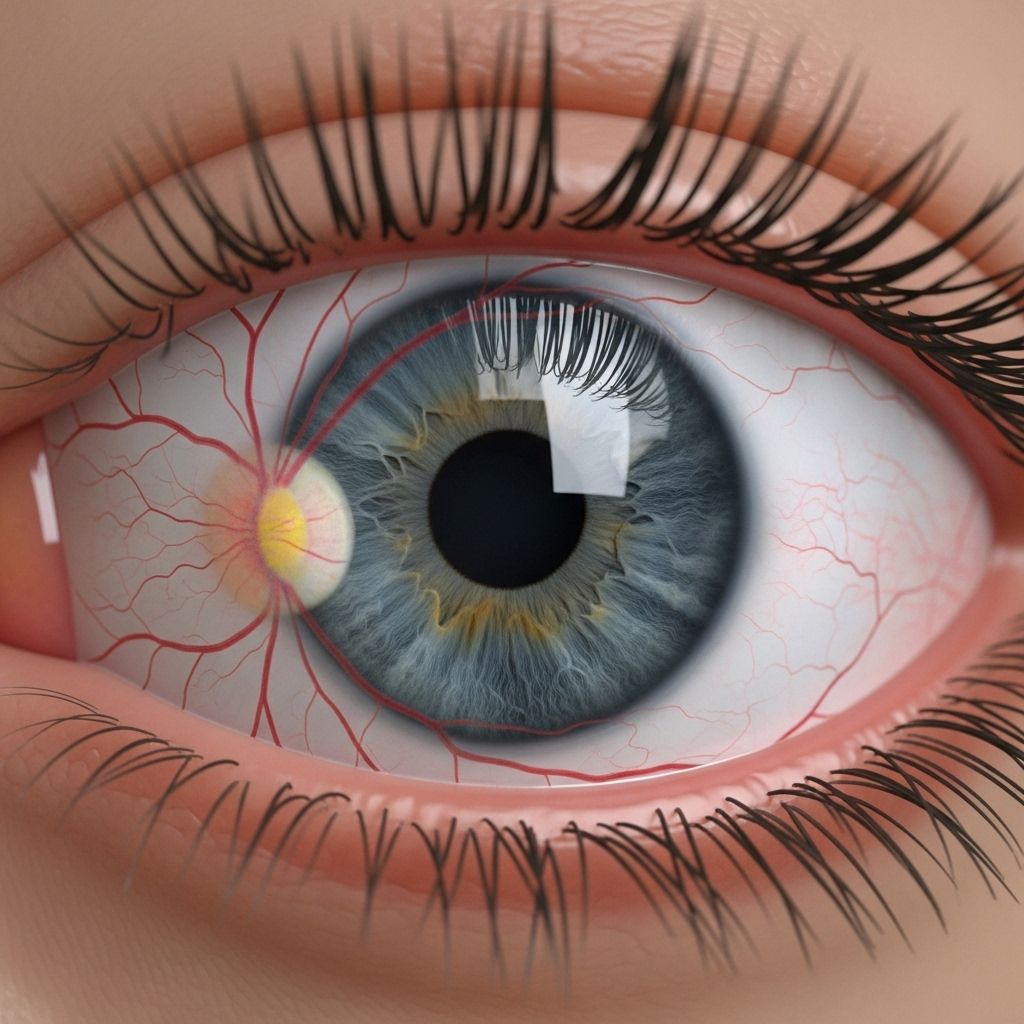
Retinal detachment is a serious eye condition that occurs when the retina—a thin, light-sensitive layer at the back of the eye—separates from its normal position and underlying blood supply. This separation disrupts the retina’s ability to function properly and can lead to permanent vision loss if not treated quickly. Understanding the types, symptoms, causes, and available treatments for retinal detachment can help individuals recognize the urgency of this condition and seek timely intervention.
What Is Retinal Detachment?
The retina’s crucial role in converting light into electrical signals means that its detachment can have catastrophic consequences for vision. Retinal detachment is considered a medical emergency. Without prompt treatment, the separated retina cannot access vital nutrients and oxygen, which may lead to irreversible sight loss.
Main Types of Retinal Detachment
Retinal detachments are classified into three distinct types, each with unique causes and clinical features:
- Rhegmatogenous retinal detachment
- Tractional retinal detachment
- Exudative retinal detachment
Comparison Table: Types of Retinal Detachment
| Type | Main Cause | Key Feature | Common Risks |
|---|---|---|---|
| Rhegmatogenous | Retinal tear or hole | Gel-like vitreous fluid leaks under the retina | Aging, trauma, nearsightedness |
| Tractional | Scar tissue formation on retina | Retina is pulled away by fibrous tissue | Diabetes, inflammatory diseases |
| Exudative | Fluid accumulation without tears | Abnormal fluid leaks beneath retina | Eye injury, tumors, inflammation, AMD |
Rhegmatogenous Retinal Detachment
Rhegmatogenous detachment is the most common form of retinal detachment. It occurs when a tear or hole forms in the retina, allowing the gel-like vitreous fluid inside the eye to seep behind the retina. This fluid buildup pushes the retina away from the back wall of the eye, causing a detachment.
The main risk factor is aging. As we get older, the vitreous gel tends to shrink and change in texture, which can lead to a tear or separation from the retina. Nearsighted individuals are also at increased risk due to their eye structure, and trauma or previous eye surgery can further elevate this risk.
Sometimes, areas of the retina thin abnormally (such as in lattice degeneration), leading to susceptibility for tears.
- Aging: Most common cause due to changes in the vitreous.
- Eye injury: Trauma can induce tears.
- Nearsightedness (myopia): Structural changes increase risk.
- Previous eye surgery: Especially cataract procedures.
- Lattice degeneration: Peripheral thinning can predispose to tears.
Tractional Retinal Detachment
Tractional retinal detachment arises when scar tissue (fibrous or fibrovascular tissue) grows on the surface of the retina and pulls it away from the back of the eye. This type is most often associated with chronic medical conditions, particularly poorly controlled diabetes that leads to diabetic retinopathy.
Scar tissue either results from blood vessel growth or previous injury/inflammation. The pulling force by this tissue separates the retina from its normal position.
- Diabetes (diabetic retinopathy): Leading cause of tractional detachment due to abnormal blood vessel growth.
- Eye injury: Can induce scar formation.
- Inflammatory diseases: May cause cellular changes resulting in fibrosis.
Exudative Retinal Detachment
Exudative retinal detachment occurs when fluid builds up beneath the retina but does not result from a tear or hole. Instead, the fluid accumulates due to abnormal leakage from blood vessels or inflammation within the eye. This type is less common but remains sight-threatening.
- Inflammatory disorders: Uveitis, scleritis, and other conditions can increase vascular leakage.
- Eye injury: Trauma can trigger abnormal fluid accumulation.
- Eye tumors: Can disrupt vascular integrity.
- Age-related macular degeneration (AMD): Damaged blood vessels leak fluid.
Symptoms of Retinal Detachment
Recognizing symptoms early is crucial. Retinal detachment is typically painless, but vision changes may develop suddenly or progress gradually.
- Floaters: Small, dark or transparent moving spots in the field of vision.
- Flashes of light: Brief flashes, especially in peripheral vision.
- Shadow or curtain effect: A dark area spreading across the visual field, sometimes described as a curtain being drawn.
- Blurred vision: Progressive or sudden blurring.
- Loss of peripheral vision: Peripheral shadows may encroach on central sight.
Some cases may present with minimal or no symptoms until the detachment expands and affects the central retina.
Causes and Risk Factors
- Aging and vitreous changes (most common for rhegmatogenous type)
- Eye trauma or injury
- Previous eye surgeries
- High degree of myopia
- Lattice degeneration
- Diabetes mellitus (tractional type)
- Inflammation and certain eye conditions (exudative type)
- Tumors and AMD
Diagnosis
Prompt and thorough diagnosis is critical due to the potential for rapid sight loss. Eye specialists use several methods to assess retinal detachment:
- Comprehensive dilated eye exam: Detects tears, holes, or areas of detachment.
- Ophthalmoscopy: Evaluates the retina through the pupil.
- Optical coherence tomography (OCT): High-resolution imaging to visualize retinal layers.
- Ultrasound imaging: Used when media opacities (like cataracts or blood) block direct view.
Treatment Options
Retinal detachment must be treated quickly to restore or preserve vision. The best treatment depends on the type and severity of detachment, as well as the patient’s overall health. Interventions generally aim to repair tears, reattach the retina, and prevent further detachment.
Surgical Treatments for Retinal Detachment
- Laser photocoagulation: Seals retinal tears using laser energy.
- Cryopexy: Freezes around the tear to promote scarring and sealing.
- Scleral buckle surgery: Silicone band is placed around the eyeball to press the wall against the retina.
- Pneumatic retinopexy: A gas bubble is injected into the eye to press the retina against its wall and close the tear. This is often combined with laser or cryotherapy.
- Vitrectomy: Removal of the vitreous gel, especially for complex cases and tractional detachments.
Treatment Considerations by Detachment Type
- Rhegmatogenous: Most often treated with laser, cryotherapy, scleral buckle, pneumatic retinopexy, or vitrectomy, depending on tear complexity.
- Tractional: Vitrectomy is usually required to remove scar tissue and relieve traction.
- Exudative: Medical treatment to reduce inflammation, address underlying tumors, or treat vascular disease. Surgery is less common unless there is significant fluid accumulation.
Prevention and Eye Health
Although some risk factors like aging are unavoidable, the following steps can reduce your risk of retinal detachment:
- Schedule regular comprehensive eye exams, especially if you are nearsighted or have diabetes.
- Protect eyes from trauma by using safety gear during sports, home improvement, or hazardous work.
- Control chronic conditions, particularly diabetes, to limit retinal damage.
- Seek prompt medical attention for any sudden changes in vision, such as the sudden appearance of floaters, flashes, or loss of peripheral sight.
Frequently Asked Questions (FAQs)
Q: How quickly should I seek help for symptoms of retinal detachment?
A: Retinal detachment is a medical emergency. Immediate evaluation by an eye care professional is essential to prevent permanent vision loss.
Q: Can retinal detachment be prevented?
A: Not all cases are preventable. However, regular eye exams, diabetes management, eye protection, and prompt attention for vision changes can lower the risk.
Q: Are all types of retinal detachment treated with surgery?
A: Rhegmatogenous and tractional detachments usually require surgery, while exudative types may respond to medications or treatments targeting the underlying condition.
Q: How successful is surgery for retinal detachment?
A: Rapid intervention can often preserve or restore vision, but outcomes depend on the detachment’s severity, location, and duration before treatment.
Q: What role does diabetes play in retinal detachment?
A: Diabetes increases risk of tractional retinal detachment due to abnormal blood vessel growth and scar tissue formation in the retina.
Key Takeaways
- Retinal detachment is a medical emergency where the retina separates from the back of the eye, threatening vision.
- Three main types: rhegmatogenous (most common; due to tear), tractional (scar tissue pull), and exudative (fluid accumulation without tear).
- Symptoms include floaters, flashes, peripheral shadows, and vision loss.
- Risk factors include age, injury, diabetes, high myopia, and inflammation.
- Treatment options range from surgery to medication, depending on detachment type.
- Early diagnosis and intervention are vital for saving sight.
References
- https://www.retinagroupflorida.com/blog/understanding-retinal-detachment-causes-symptoms-and-treatment-options
- https://hackensackeye.com/retinal-detachment/
- https://www.asrs.org/retinaldetachment
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/retinal-detachment/types-and-causes-retinal-detachment
- https://www.medparkhospital.com/en-US/disease-and-treatment/retinal-detachment
- https://my.clevelandclinic.org/health/diseases/10705-retinal-detachment
- https://eyewiki.org/Retinal_Detachment
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/retinal-detachment
Read full bio of medha deb












