Types of Non-Small Cell Lung Cancer Explained
A comprehensive guide to NSCLC types, risk factors, symptoms, diagnosis, treatment, and prognosis for patients and caregivers.
Types of Non-Small Cell Lung Cancer
Non-small cell lung cancer (NSCLC) is the most common type of lung cancer, representing about 80%–85% of all lung cancer diagnoses. Understanding the subtypes, risk factors, symptoms, and available treatments is essential for patients, caregivers, and healthcare providers seeking effective management strategies for this complex disease.
What is Non-Small Cell Lung Cancer?
Non-small cell lung cancer is a broad category composed of several distinct cancer types that arise from the epithelial cells lining the lungs, excluding small cell lung cancer (SCLC). Unlike SCLC, NSCLC generally grows and spreads more slowly, but outcomes and treatment options still vary by subtype and stage.
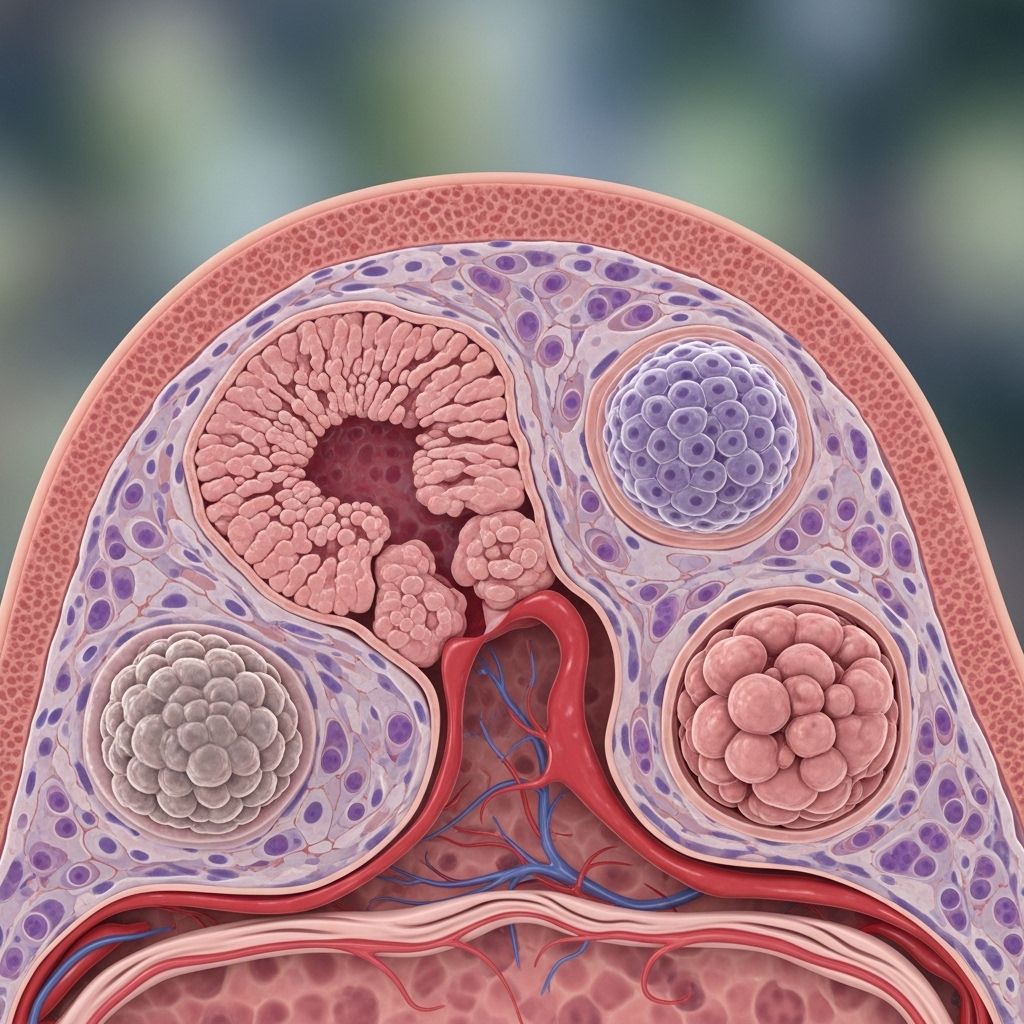
Main Subtypes of NSCLC
There are three primary subtypes of non-small cell lung cancer, each with distinct characteristics and clinical implications:
- Adenocarcinoma: The most common subtype of NSCLC (comprising about 40% of cases). It typically arises in the outer areas of the lungs and develops from cells that produce mucus. This type can occur in both smokers and non-smokers, and it is the predominant lung cancer in people who have never smoked.
Key Features:
- Often found in the periphery (outer regions) of the lung
- More common in women and younger patients
- Associated with smoking but also found in non-smokers
- Can produce substances such as mucus
Understanding the symptoms of non-small cell lung cancer is crucial for early detection and effective management. For an in-depth look at what to look for, check out our detailed overview of NSCLC symptoms and diagnosis. Identifying these symptoms could be pivotal in seeking timely medical advice. - Squamous Cell Carcinoma: Making up about 25%–30% of NSCLC cases, squamous cell carcinoma develops in the central parts of the lungs, near the main airways (bronchi), usually in areas previously affected by smoking-related damage.
Key Features:
- Originates in the central part of the lungs
- Frequently linked to a history of tobacco smoking
- Tends to form cavities within the tumor mass
- Large Cell Carcinoma: Representing about 10% of NSCLC, large cell carcinoma can occur anywhere in the lung and tends to grow and spread rapidly. Some subtypes, such as large cell neuroendocrine carcinoma, are particularly aggressive.
Key Features:
- Can arise in any lung region
- Often grows quickly with a tendency for early metastasis
- Includes uncommon variants: neuroendocrine carcinoma, clear cell carcinoma, lymphoepithelioma-like carcinoma
Other Less Common NSCLC Variants
- Adenosquamous carcinoma: Tumors showing both glandular (adenocarcinoma) and squamous features.
- Sarcomatoid carcinoma: Rare tumors with spindle-shaped or giant cells, representing a morphological overlap between carcinomas and sarcomas.
- Salivary gland type tumors: Extremely rare and behave similarly to salivary gland cancers elsewhere in the body.
- Carcinoid tumors: Atypical carcinoids have an intermediate prognosis, falling between the less aggressive typical carcinoids and high-grade carcinomas.
Incidence and Mortality
Lung cancer remains the leading cause of cancer-related deaths worldwide. In the United States alone, it is estimated that 226,650 new cases and 124,730 deaths from lung cancer (NSCLC and SCLC combined) will occur in 2025.*
- The overall 5-year relative survival rate for lung cancer is 27%.
- Survival rates are stage-dependent:
- Local Stage: 64% 5-year survival
- Regional Stage: 36% 5-year survival
- Distant Stage: 9% 5-year survival
Risk Factors for NSCLC
Several factors increase the risk of developing non-small cell lung cancer. The strongest association is with exposure to tobacco smoke, but other environmental, occupational, and genetic factors contribute.
- Tobacco smoking: Responsible for about 80% of cases. Both active and secondhand smoke elevate risk.
The risk depends on the amount and duration of smoking. Stopping smoking reduces risk over time. - Exposure to environmental carcinogens:
- Air pollution (particularly PM2.5 and nitrogen dioxide)
- Arsenic (found in contaminated water)
- Radon
- Workplace exposure: Mining, manufacturing, and chemical work may expose individuals to carcinogens such as asbestos, uranium, beryllium, vinyl chloride, nickel chromates, coal products, and diesel exhaust.
- Radiation exposure: Previous radiotherapy to the chest increases risk.
- Genetic predisposition: Family history of lung cancer and certain inherited mutations.
- Other risk factors: Age (rare in people under 45), chronic lung disease, smoking marijuana (some studies suggest possible risk but no direct link established).
Symptoms and Warning Signs
NSCLC symptoms are often subtle in early stages, contributing to late diagnoses. Symptoms vary by tumor type, size, location, and spread.
- Persistent cough
- Coughing up blood (hemoptysis)
- Chest pain
- Shortness of breath
- Hoarseness
- Recurrent respiratory infections (pneumonia, bronchitis)
- Unexplained weight loss
- Fatigue
- Loss of appetite
- Wheezing
Advanced cancer can produce bone pain, neurological symptoms (if metastatic to the brain), and lymph node enlargement.
Diagnostic Methods
Diagnosis of NSCLC involves a combination of imaging studies, laboratory tests, histological analysis, and molecular profiling:
- Imaging: Chest X-ray, computed tomography (CT), positron emission tomography (PET), and magnetic resonance imaging (MRI).
- Tissue biopsy: Samples obtained by bronchoscopy, needle aspiration, or surgical techniques.
- Histopathological examination: Determines cancer subtype (adenocarcinoma, squamous cell, large cell, variants).
- Molecular testing: Assesses genetic mutations such as EGFR, ALK, KRAS, and ROS1 to guide targeted therapies.
- Laboratory studies: Sputum cytology, blood tests, and tumor marker detection.
Staging and Classification
Staging of non-small cell lung cancer is critical for guiding treatment decisions and determining prognosis.
| Stage | Description | 5-Year Survival Rate |
|---|---|---|
| Stage I | Cancer confined to one lung (no lymph node spread) | 60–80% |
| Stage II | Cancer spread to nearby lymph nodes | 35–50% |
| Stage III | Cancer spread to lymph nodes near the center of the chest | 7–25% |
| Stage IV | Cancer metastasized to distant organs | Less than 5% |
Staging uses the TNM (Tumor, Node, Metastasis) system based on tumor size, lymph node involvement, and distant metastasis.
Treatment Options for NSCLC
Treatment strategies depend on cancer stage, subtype, molecular profile, and overall health of the patient. Approaches include:
- Surgery: Preferred for early-stage cancers (stages I and II) where complete tumor removal is possible.
- Radiation therapy: Used to control local tumor growth, especially in patients who cannot undergo surgery.
- Chemotherapy: Systemic drugs (platinum compounds, taxanes, pemetrexed) to kill cancer cells, often combined with surgery or radiation for higher stages.
- Targeted therapies: Agents designed to block specific genetic alterations (e.g., EGFR inhibitors, ALK inhibitors, ROS1 inhibitors).
- Immunotherapy: Drugs such as checkpoint inhibitors (pembrolizumab, nivolumab) that enhance the immune response against cancer cells.
- Palliative care: Symptom management and supportive care for advanced cancers to improve quality of life.
Patients with resectable disease have the best chance of cure. Those with unresectable or metastatic disease may benefit from combined approaches, including new targeted and immunotherapeutic agents.
Prognosis and Outlook
The prognosis for NSCLC varies based on the cancer subtype, stage at diagnosis, and the patient’s overall health and molecular tumor characteristics. Early detection is associated with improved survival rates, but the majority of cases are diagnosed at advanced stages.
- Localized tumors (detected and treated early) have a relatively favorable prognosis.
- Regional or distant metastasis is associated with reduced survival and increased treatment complexity.
- Molecular markers and genetic profiles increasingly inform targeted therapies, offering improved outcomes for select patients.
Long-term survival is possible for some patients with advanced NSCLC through new therapies and clinical trials.
FAQs About NSCLC
Q: What is the difference between NSCLC and SCLC?
A: NSCLC (non-small cell lung cancer) comprises about 80–85% of lung cancers, grows more slowly, and is less sensitive to chemotherapy than SCLC (small cell lung cancer), which is faster growing and more likely to respond to chemotherapy and radiation.
Q: Can non-smokers develop NSCLC?
A: Yes, adenocarcinoma—a subtype of NSCLC—is common among non-smokers, especially women and younger people. Environmental factors, genetics, and occupational exposures can also play a role.
Q: What are the main treatment options for NSCLC?
A: Treatments include surgery, radiation therapy, chemotherapy, targeted therapies (e.g. EGFR, ALK inhibitors), and immunotherapy, depending on cancer stage and genetic profile.
Q: Is lung cancer always diagnosed at a late stage?
A: The majority of lung cancers are diagnosed at later stages due to subtle symptoms, but screening with low-dose CT in high-risk individuals can help detect cancer at earlier, more treatable stages.
Q: How can I lower my risk of developing NSCLC?
A: Avoid tobacco smoke, reduce exposure to carcinogens (both environmental and occupational), maintain healthy air quality, and seek regular medical care if at high risk.
Key Takeaways
- NSCLC is the most prevalent form of lung cancer, comprising three main subtypes: adenocarcinoma, squamous cell carcinoma, and large cell carcinoma.
- Symptoms are often vague and may include cough, chest pain, and unexplained weight loss.
- Risk is highest with tobacco exposure, but non-smokers are also vulnerable.
- Early diagnosis and molecular testing are crucial for selecting an effective treatment approach and improving survival rates.
- Emerging therapies—immunotherapy and targeted drugs—offer hope for advanced cases.
* Incidence and mortality figures are based on current estimates. Please consult your doctor or cancer specialist for personalized advice and updated data.
References
- https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/basics/lung-cancer-types
- https://www.cancer.gov/types/lung/hp/non-small-cell-lung-treatment-pdq
- https://medlineplus.gov/ency/article/007194.htm
- https://my.clevelandclinic.org/health/diseases/6203-non-small-cell-lung-cancer
- https://www.healthline.com/health/lung-cancer-non-small-cell
- https://www.healthline.com/health/video/5-things-pnsclc
- https://pmc.ncbi.nlm.nih.gov/articles/PMC2718421/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4931124/
- https://www.medicalnewstoday.com/articles/323701
Read full bio of medha deb












