Understanding Types of Macular Degeneration: Dry, Wet, and Beyond
Explore the different types of macular degeneration, their progression, treatment options, and impacts on vision for better eye health awareness.
What to Know About Different Types of Macular Degeneration
Macular degeneration is a progressive eye disorder that impairs the macula, a crucial part of the retina responsible for central vision. Over time, this condition can lead to significant vision issues and even blindness. Understanding the types of macular degeneration is essential for effective diagnosis, management, and treatment options. This guide examines the core differences between the types, their progression, and clinical impact.
Key Points Covered in This Article
- Definitions and classifications of macular degeneration
- Characteristics of dry (atrophic) and wet (neovascular) age-related macular degeneration
- Prevalence and epidemiology
- Rare genetic forms of macular degeneration
- Symptoms, risk factors, and progression
- Why distinguishing between types matters for treatment
What Types of Macular Degeneration Are There?
Macular degeneration isn’t limited to a single disease. Several types exist, each impacting vision differently:
- Age-related Macular Degeneration (AMD) – Most common and subdivided into dry and wet forms.
- Juvenile Macular Degeneration or Dystrophies – Includes diseases like Stargardt and Best disease, typically presenting earlier in life.
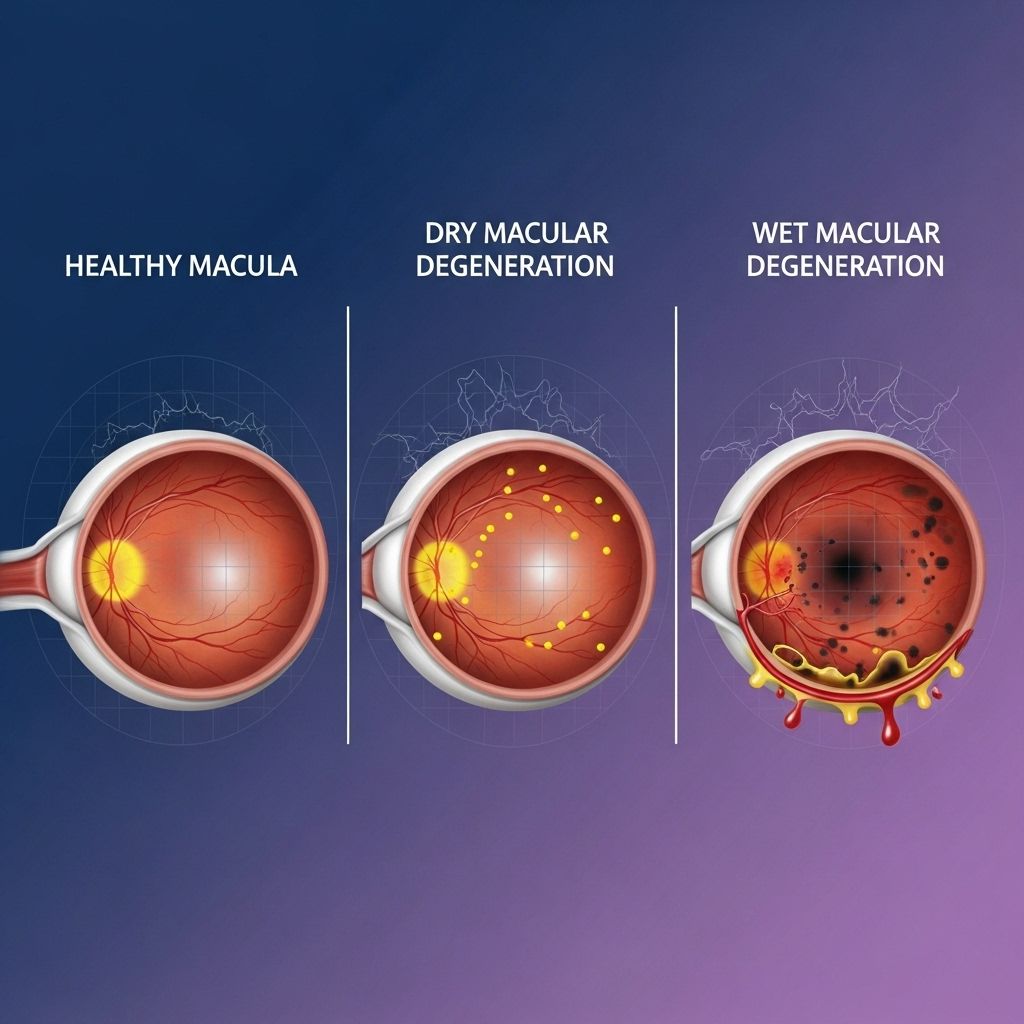
The well-known forms are dry and wet AMD:
- Dry (Atrophic) AMD: The macula thins gradually as you age, often starting in your 50s. The progression is slow, and symptoms can be subtle or absent in early stages.
- Wet (Neovascular) AMD: The condition develops quickly, with abnormal blood vessel growth under the retina leading to bleeding, fluid leakage, and swift vision decline.
Rare Genetic Forms of Macular Degeneration
Though age-related types predominate, rare forms associated with genetic mutations exist. These tend to affect children or younger adults, and include:
- Best Disease – Linked to mutations in the BEST1 gene.
- Stargardt Disease (macular dystrophy) – Caused by the ABCA4 gene; inherited recessively.
- Stargardt-like Macular Dystrophy – Related to ELOVL4 gene mutations.
- Malattia Leventinese (Doyne honeycomb) retinal dystrophy – Involves EFEMP1 gene.
- Sorsby Fundus Dystrophy – Driven by TIMP3 gene mutations; presents similarly to wet AMD.
These rare forms are inherited either dominantly or recessively and are quite uncommon, affecting fewer than 1 in 2,000 people.
Dry Age-Related Macular Degeneration: The Most Common Type
Dry AMD is responsible for about 85-90% of all cases, making it by far the most prevalent macular degeneration subtype.
- Typically affects people over 50 years old, with risk increasing dramatically by age 85 and above.
- Estimated 20 million Americans lived with some form of macular degeneration as of 2019. Around 1.49 million, aged 40 and up, were in the late stages.
- Prevalence increases with age; about 2% in people aged 40 to 44, surging to nearly 46.6% among those over 85.
How Does Dry AMD Develop?
Dry AMD develops in three broad stages:
- Early Stage: Often no symptoms; small drusen (protein deposits) form under the retina.
- Intermediate Stage: Larger drusen, possible mild vision changes.
- Late Stage (Geographic Atrophy): Cell death in the retina; pronounced vision changes including blurred or dark central areas.
Symptoms of Dry AMD
- Blurry central vision
- Difficulty seeing and reading in low light
- Faded or dull colors
- Blind spots in the central vision
What Is Geographic Atrophy?
Geographic atrophy defines the advanced stage of dry AMD. It affects about 1 million people in the United States and is characterized by:
- Dark spots in the center of vision
- Numbers or letters disappearing during reading
- Difficulty distinguishing colors
- Problems seeing in dimly lit environments
Not all cases of dry AMD progress to geographic atrophy, but certain risk factors make this outcome more likely.
Risk Factors Associated With Dry AMD
- Older age (particularly over 60)
- Family history of the condition
- Poor diet and nutrition
- High blood pressure or high cholesterol
- Obesity
- Extended sun exposure
- Smoking
- Diabetes or heart disease
Management and Treatment of Dry AMD
- Regular eye exams for monitoring progression
- Adopting healthy lifestyle changes, such as quitting smoking and increasing exercise
- No treatment currently available for early stages, but preventive strategies are recommended
- Advanced geographic atrophy may require vision aids and rehabilitation
Wet Age-Related Macular Degeneration: Advanced and Rapid
While dry AMD develops slowly, wet AMD (also called neovascular or exudative AMD) is less common, accounting for about 10-20% of AMD cases, but progresses much more rapidly.
- Characterized by abnormal growth of blood vessels beneath the retina, which leads to leakage or bleeding.
- Causes sudden and severe central vision loss.
- Often considered an advanced stage of AMD.
Symptoms of Wet AMD
- Blurry or distorted vision
- Wavy lines or shapes, especially in central vision
- Rapid onset of blank spots or dark areas
- Difficulty recognizing faces, reading, or driving
Treatment Options for Wet AMD
Treatments for wet AMD focus on slowing or halting blood vessel growth:
- Anti-VEGF injections: These medications inhibit vascular endothelial growth factor, reducing vessel growth and leakage.
- Laser photocoagulation therapy: Selectively treats leaking blood vessels in rare cases.
- Photodynamic therapy: Combines injectable drugs with laser light to target abnormal vessel growth.
Prompt intervention is critical; untreated wet AMD can lead to permanent, severe vision loss within weeks or months.
Why Does It Matter What Type of Macular Degeneration You Have?
Knowing your type of macular degeneration is critical for several reasons:
- Treatment Choices: Available therapies differ between dry and wet AMD.
- Prognosis: Dry AMD progresses slowly, while wet AMD advances quickly with severe impact on vision.
- Risk Assessment: Symptom monitoring and preventive strategies vary based on type.
Vision Effects in Both Types
While both types often cause central vision problems, their presentations differ:
- Dry AMD: Gradual, subtle changes; may include trouble with night vision and faded colors.
- Wet AMD: Sudden vision distortion and rapid progression to blank spots.
| Feature | Dry AMD | Wet AMD |
|---|---|---|
| Prevalence | About 85-90% of cases | About 10-20% of cases |
| Onset & Progression | Develops slowly over years | Develops rapidly over weeks or months |
| Vision Loss | Gradual central vision loss | Sudden severe central vision loss |
| Treatment | Lifestyle & monitoring; no cure | Anti-VEGF injections, laser, other therapies |
| Symptoms | Blurry/dull vision, blind spots | Distorted vision, dark spots, wavy appearance |
Other Forms: Genetic Macular Degeneration
Though most cases are age-related, some forms of macular degeneration stem from rare genetic mutations. These forms can present in childhood or early adulthood and may include:
- Stargardt disease – Causes progressive vision loss and color changes, inherited from both parents.
- Best disease – Follows autosomal dominant inheritance; patients only need one mutated gene from a parent.
- Malattia Leventinese – Marked by characteristic “honeycomb” patterns of deposits under the retina.
- Sorsby fundus dystrophy – Clinically similar to wet AMD.
These conditions are rare (less than 1 in 2,000 people) and require genetic counseling for families affected.
Frequently Asked Questions (FAQs)
Q: What is the difference between dry and wet macular degeneration?
Dry AMD develops slowly as the retina thins and is more common. Wet AMD is caused by abnormal blood vessel growth under the retina and is less common but far more serious due to its rapid progression.
Q: Can macular degeneration lead to complete blindness?
No. Macular degeneration affects central vision but usually does not cause complete blindness. Peripheral vision is usually retained, although central vision loss can significantly impact daily activities.
Q: Are lifestyle changes useful for managing macular degeneration?
Yes. Maintaining a healthy diet, quitting smoking, controlling blood pressure and cholesterol, and regular exercise can help slow the progression and reduce risk factors.
Q: How is macular degeneration diagnosed?
Diagnosis requires a comprehensive eye exam, including retinal imaging and evaluation of visual acuity. Staging helps determine seriousness and treatment options.
Q: Are there treatments available for early stages of macular degeneration?
Currently, there are no cures for early dry AMD, but wet AMD can often be treated effectively if caught early. Regular monitoring is essential for early intervention.
Key Takeaways
- Macular degeneration includes dry, wet, and rare genetic forms—each with unique vision risks and treatment considerations.
- Dry AMD is the most common, typically progressing slowly; wet AMD is much less common but more aggressive.
- Early diagnosis and identifying the type are crucial for preserving sight and choosing the best therapies.
- Lifestyle modifications and prompt medical interventions help manage progression and outcomes.
References
- https://www.healthline.com/health/eye-health/macular-degeneration-types
- https://www.britannica.com/science/macular-degeneration
- https://www.medicalnewstoday.com/articles/macular-degeneration-types
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/age-related-macular-degeneration
- https://www.medicalnewstoday.com/articles/can-macular-degeneration-be-reversed
- https://www.webmd.com/eye-health/macular-degeneration/default.htm
Read full bio of Sneha Tete












