Types of Heart Attacks: Names, Symptoms, and Treatment
Learn about STEMI, NSTEMI, and coronary artery spasm heart attacks, their symptoms, treatments, risks, and prevention.
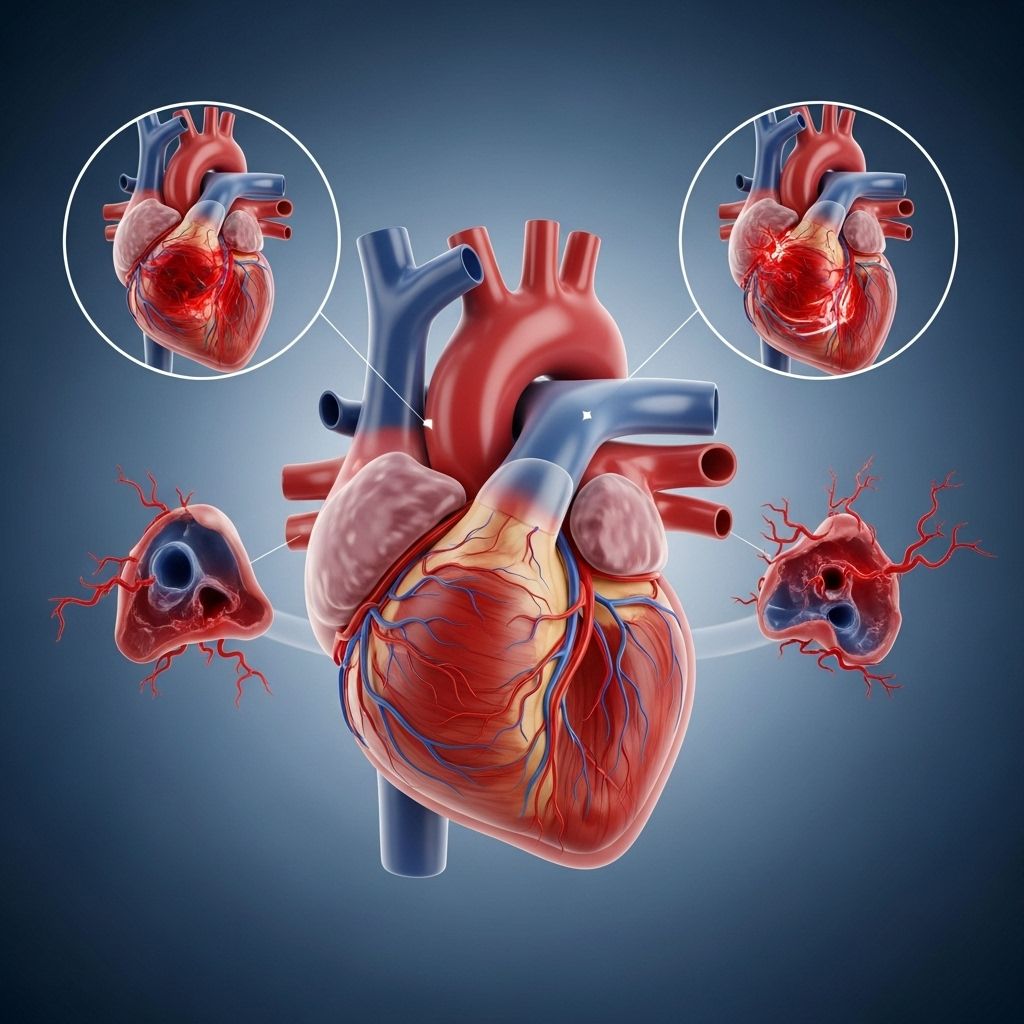
Heart attacks, medically called myocardial infarctions, are serious medical emergencies that require prompt attention. They occur when the arteries supplying blood to the heart muscle (coronary arteries) become blocked or suddenly constrict, impairing adequate blood flow and leading to damage of heart tissue. Understanding the types, symptoms, treatment, and recovery process is crucial for anyone at risk or interested in cardiovascular health.
What Is Acute Coronary Syndrome and a Heart Attack?
Acute coronary syndrome (ACS) refers to a range of conditions, including heart attacks, that result from blocked blood flow to the heart muscle. Heart attacks happen when one or more coronary arteries are obstructed and the heart doesn’t receive enough oxygenated blood. The most critical form of ACS is the myocardial infarction, typically caused by a buildup of fatty deposits and cholesterol (called plaques), which can rupture or become unstable and trigger blood clots, blocking blood flow.
Key Facts About Heart Attacks
- Heart attacks are also known as myocardial infarctions (MI).
- The main symptom is chest pain or discomfort, but other symptoms may occur, especially in women.
- There are several types of heart attacks, each requiring a tailored approach to management and treatment.
Types of Heart Attacks
There are three primary types of heart attacks, distinguished by the nature and severity of artery blockage and how they present on an electrocardiogram (ECG).
- ST segment elevation myocardial infarction (STEMI)
- Non-ST segment elevation myocardial infarction (NSTEMI)
- Coronary artery spasm (also known as unstable angina)
1. ST Segment Elevation Myocardial Infarction (STEMI)
STEMI heart attacks are considered the most severe and dangerous type. They occur when a major coronary artery is completely blocked, preventing blood from reaching a significant area of the heart muscle. The name arises from the pattern of “ST elevation” seen on an ECG, which signals extensive damage.
- Symptoms:
- Intense or crushing chest pain
- Pain may radiate to the left arm, shoulder, neck, or jaw
- Shortness of breath
- Nausea and vomiting
- Cold sweat and lightheadedness
The symptoms of NSTEMI heart attacks can often be subtle, making them easy to overlook. However, understanding these differences is vital for seeking the right care in a timely manner. If you’re wondering how to differentiate between various heart attack symptoms, read our in-depth guide to recognizing NSTEMI signs and what you should do. - Causes: Complete blockage of a coronary artery due to rupture of an atherosclerotic plaque and subsequent clotting.
- Diagnosis: ECG showing ST-segment elevation; elevated cardiac biomarkers (troponin).
- Urgency: Requires immediate emergency care to restore blood flow and save heart tissue.
2. Non-ST Segment Elevation Myocardial Infarction (NSTEMI)
NSTEMI heart attacks occur when a coronary artery is partially blocked, leading to reduced blood flow and damage to the heart muscle. The ST segment does not show elevation on an ECG, which distinguishes this type.
- Symptoms:
- Chest pain or discomfort (often milder than STEMI)
- Shortness of breath
- Fatigue, nausea
Confusing angina with a heart attack can be risky. Angina often manifests as temporary chest discomfort, but knowing the differences can help you respond effectively to serious issues. Understanding these distinctions can guide you in seeking immediate medical assistance when needed. Find out how to tell the difference and when to take action to safeguard your heart health. - Causes: Partial blockage due to plaque, clot, or other substances narrowing the coronary arteries.
- Diagnosis: ECG without ST elevation; increased cardiac biomarkers (troponin).
- Risks: Can still cause significant damage and requires prompt medical management.
3. Coronary Artery Spasm (Unstable Angina)
A coronary spasm occurs when the coronary artery suddenly contracts (spasms), temporarily decreasing or stopping blood flow to part of the heart muscle. If prolonged or severe enough, it can trigger a heart attack. If not severe, symptoms are called “unstable angina.”
- Symptoms:
- Chest pain or tightness (often occurring at rest)
- Shortness of breath
- Dizziness
- Causes: Spasm can be triggered by stress, certain drugs (e.g., cocaine), cold exposure, or other conditions.
- Diagnosis: May not show blockage on angiogram, but symptoms and ECG can suggest spasm.
- Prognosis: Can lead to heart attack or be a warning sign of severe underlying disease.
Table 1: Comparison of Heart Attack Types
| Type | Blockage in Artery | ECG Findings | Urgency | Common Symptoms |
|---|---|---|---|---|
| STEMI | Complete | ST elevation | Critical / Emergency | Severe chest pain, breathlessness |
| NSTEMI | Partial | No ST elevation | Serious / Urgent | Chest pain, mild symptoms |
| Coronary Spasm | Temporary / None | Variable, may show changes | Urgent if prolonged | Chest pain (often at rest) |
Symptoms of Heart Attacks
While chest pain is the hallmark symptom, heart attacks may present with a variety of warning signs. Recognizing these, particularly early, can save lives.
- Crushing, squeezing, or burning chest pain or pressure
- Pain radiating to the arms (often left side), neck, jaw, back, or stomach
- Shortness of breath
- Nausea, vomiting, or indigestion-like discomfort
- Cold sweat, dizziness, or lightheadedness
- Unusual fatigue (especially in women and elderly)
Not everyone experiences classic chest pain. Women, older adults, and people with diabetes may have subtler symptoms such as unexplained tiredness, indigestion, or neck pain.
Causes and Risk Factors
Heart attacks typically result from cardiovascular disease, especially the buildup of plaques in coronary arteries. Several lifestyle and genetic factors increase risk:
- High blood pressure
- Smoking
- High cholesterol
- Diabetes
- Obesity
- Poor diet (high in saturated fats, cholesterol)
- Physical inactivity
- Family history of heart disease
- Excessive alcohol intake
- Stress, illicit drug use (especially cocaine)
Diagnosis of Heart Attacks
- Electrocardiogram (ECG): Measures electrical activity of the heart to diagnose STEMI/NSTEMI.
- Blood tests: Primarily troponin, rise when heart muscle is damaged.
- Imaging: Echocardiogram or coronary angiography to check for blockage and heart function.
Treatment Options
Treatment differs depending on the type and severity of heart attack, but prompt intervention is essential in every case.
Immediate Treatments
- STEMI: Urgent percutaneous coronary intervention (PCI) such as angioplasty and stenting, or clot-busting medications (thrombolytics) to restore blood flow.
- NSTEMI: Timely PCI for some, medications to reduce heart strain, blood thinners (antiplatelets, anticoagulants), management of contributing factors.
- Coronary Spasm: Medications to relieve spasm (nitroglycerin, calcium channel blockers), and treat underlying risk factors.
Long-term Management
- Lifestyle modifications: Diet, regular physical activity, smoking cessation, weight management
- Medications: Statins (to lower cholesterol), beta-blockers, ACE inhibitors, antiplatelet drugs
- Cardiac rehabilitation: Supervised exercise, nutrition counseling, stress management
Recovery After a Heart Attack
Recovery focuses on restoring heart health, preventing further attacks, and regaining quality of life.
- Hospital care: Continuous monitoring, initial treatment, assessment of heart damage
- Cardiac rehab: Structured programs to recover physical and emotional strength
- Follow-up: Regular visits for medication management and monitoring heart health
- Support: Emotional, psychological, and social support for survivors and families
Risk Factors for Heart Attacks
Major risk factors include high blood pressure, high cholesterol, diabetes, sedentary lifestyle, poor nutrition, family history, smoking, and stress. Some are modifiable, making prevention possible by addressing these risks.
Preventing Heart Attacks
- Eat a heart-healthy diet rich in fruits, vegetables, whole grains, and healthy fats
- Exercise regularly (at least 150 minutes per week of moderate activity)
- Maintain a healthy weight and keep blood pressure, cholesterol, and diabetes controlled
- Quit smoking and avoid excessive alcohol use
- Manage chronic stress and get regular medical checkups
Frequently Asked Questions (FAQs)
Q: How do STEMI and NSTEMI heart attacks differ?
A: STEMI is a complete blockage with visible ST elevation on ECG and needs emergency intervention; NSTEMI is a partial blockage, without ST elevation but is still serious and may need urgent care.
Q: What should I do if I think I’m having a heart attack?
A: Seek emergency help immediately by calling your local emergency number. Do not drive yourself. Prompt treatment is vital to reduce heart damage.
Q: Can heart attacks be prevented?
A: Yes, many heart attacks are preventable through lifestyle changes, regular screenings, and managing risk factors like high blood pressure, cholesterol, and diabetes.
Q: Are symptoms different in women?
A: Yes, women are more likely to have less typical symptoms, including fatigue, nausea, or neck/jaw pain instead of severe chest pain.
Q: What is cardiac arrest, and how does it differ from a heart attack?
A: Cardiac arrest is when the heart suddenly stops beating, often due to an electrical malfunction. Heart attack (myocardial infarction) occurs due to blocked blood supply to the heart muscle. Cardiac arrest can result from a heart attack, but they are not the same.
Takeaway
- Heart attacks are serious, life-threatening events requiring rapid response.
- Three main types exist—STEMI, NSTEMI, and Coronary Spasm/Unstable Angina—each with unique implications for treatment and recovery.
- Understanding symptoms, risks, and prevention strategies is crucial for minimizing your risk and protecting heart health.
References
- https://www.healthline.com/health/heart-disease/types-of-heart-attacks
- https://en.wikipedia.org/wiki/Myocardial_infarction
- https://www.medicalnewstoday.com/articles/321699
- https://www.bhf.org.uk/informationsupport/heart-matters-magazine/medical/ask-the-experts/what-are-the-different-types-of-heart-attacks
- https://www.mayoclinic.org/diseases-conditions/heart-attack/symptoms-causes/syc-20373106
- https://www.massgeneralbrigham.org/en/patient-care/services-and-specialties/heart/conditions/heart-attack
- https://www.ncbi.nlm.nih.gov/books/NBK537076/
Read full bio of Sneha Tete












