Stomach Pain and Type 1 Diabetes: Causes, Symptoms, and Treatment
Understanding the link between stomach pain and type 1 diabetes can help prevent severe complications and improve quality of life.
Stomach Pain and Type 1 Diabetes: What You Need to Know
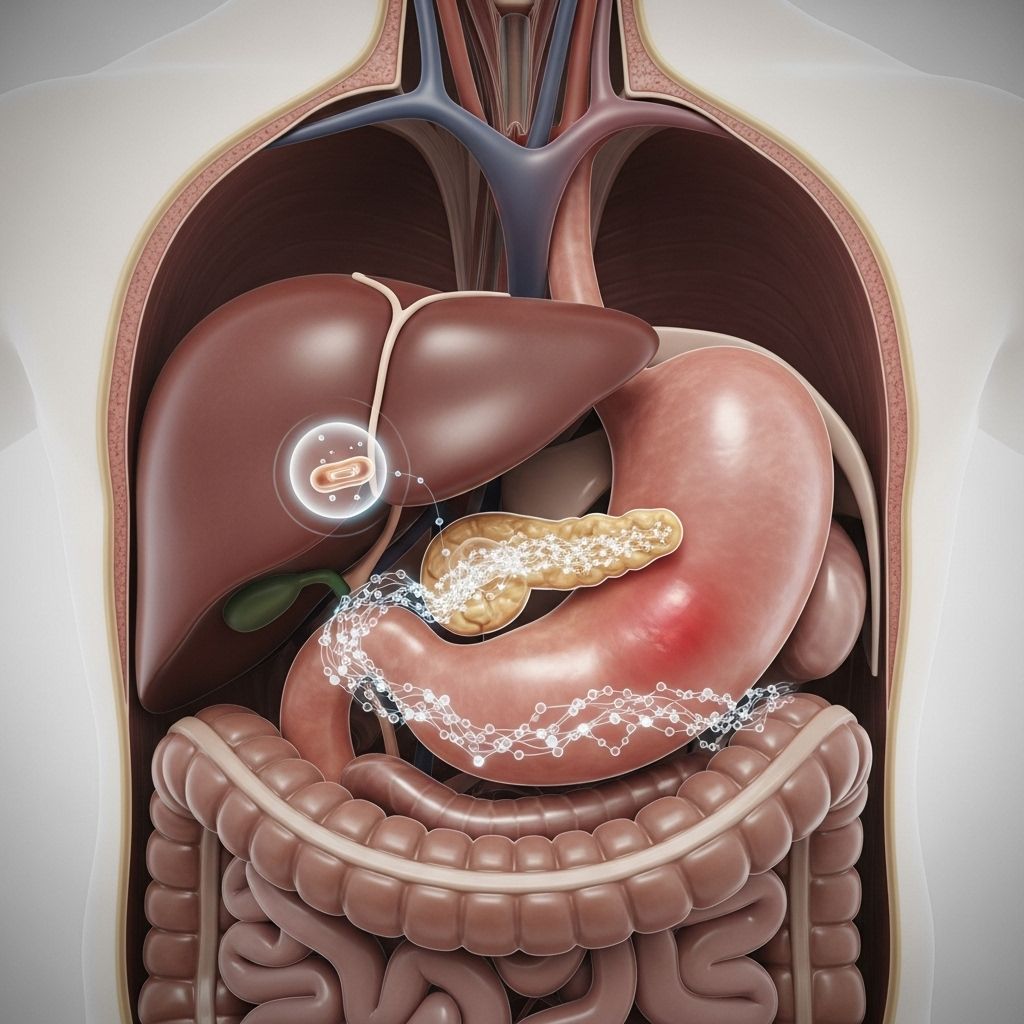
Stomach pain is generally not the first symptom people associate with type 1 diabetes (T1D), but it can be a significant sign of underlying issues. For many, this pain points to more serious diabetes-related complications such as diabetic ketoacidosis (DKA) or gastroparesis. Understanding the connection between type 1 diabetes and stomach pain can help individuals seek timely care, manage their condition, and prevent emergencies.
Can Stomach Pain Signal Type 1 Diabetes?
Though uncommon as an early indicator, stomach or abdominal pain can appear alongside other classic symptoms during the onset of type 1 diabetes. While more often a complication after diagnosis, for some, it may be the initial reason someone seeks medical attention, particularly if associated with high blood sugar or DKA episodes.
Key points about stomach pain in T1D:
- As many as 75% of people with diabetes (type 1 or type 2) experience some form of gastrointestinal (GI) symptoms such as pain, nausea, vomiting, or bloating.
- These symptoms can occur at the time of diagnosis, especially if blood sugar is high, and often result from either DKA or chronic complications like gastroparesis.
- Stomach pain can also be a clue in people without a previous diagnosis who are newly developing diabetes.
Diabetic Ketoacidosis (DKA): A Medical Emergency
Diabetic ketoacidosis (DKA) occurs when a lack of insulin causes the body to break down fat for energy instead of glucose. This process produces ketones—acids that build up in the blood and make it more acidic, which is dangerous and potentially fatal if untreated.
Symptoms of DKA
- Stomach or abdominal pain (may be severe)
- Nausea and vomiting
- Fruity-smelling breath
- Sleepiness or drowsiness
- Rapid, deep breathing
- Confusion or disorientation
- Loss of consciousness (in severe cases)
DKA is a life-threatening complication that can develop swiftly, especially in people who are undiagnosed, have illness or infection, miss insulin doses, or experience insulin delivery failures (such as a malfunctioning insulin pump).
| DKA Symptom | Common T1D Symptom |
|---|---|
| Severe stomach pain | Increased thirst |
| Nausea, vomiting | Frequent urination |
| Rapid breathing | Unintentional weight loss |
| Confusion | Fatigue |
| Fruity breath | Blurred vision |
Immediate medical attention is necessary if DKA symptoms are present, as untreated DKA can result in coma or death.
Gastroparesis: A Diabetic Digestive Complication
Gastroparesis is a digestive disorder characterized by delayed stomach emptying due to nerve and muscle dysfunction, commonly seen in diabetes. Research suggests up to 40-50% of people with T1D can experience some form of this condition.
What Causes Gastroparesis?
The primary cause is damage to the vagus nerve, which controls how the stomach muscles contract. High blood sugar over time can impact this nerve and stomach muscles, leading to slowed or erratic emptying of food from the stomach to the small intestine.
Symptoms of Gastroparesis
- Nausea after eating
- Bloating
- Vomiting undigested food (sometimes hours after a meal)
- Early satiety (feeling full too soon)
- Abdominal discomfort or pain
- Poor appetite
- Unintentional weight loss (sometimes weight gain)
- Unstable or unpredictable blood sugar levels
Gastroparesis can range from mild—causing moderate inconvenience—to severe, impairing nutrition and significantly impacting daily life.
Diagnosing Gastroparesis
- Gastric emptying scan: Involves eating a small radioactive meal and using scans to track how quickly it leaves the stomach (typically up to 4 hours).
- Breath testing: Measures breakdown of a radiolabeled compound in the breath to assess stomach emptying.
- Wireless motility capsule: A swallowed device collects and sends movement and pH data as it passes through the GI tract.
How Gastroparesis Affects Diabetes Management
- Erratic stomach emptying can make timing and effectiveness of insulin doses unpredictable.
- Higher risk of both hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar) due to mismatched food absorption and insulin action.
- Discomfort can lead to poor appetite, malnutrition, and unintentional weight changes.
Other Causes of Stomach Pain in Type 1 Diabetes
Stomach pain in people with T1D is not always due to DKA or gastroparesis. Other possible causes include:
- Infections: Gastrointestinal infections can occur independently of diabetes.
- Celiac disease: People with T1D are at increased risk and may have abdominal pain, bloating, or chronic diarrhea.
- Side effects of medication: Certain diabetes medications or antibiotics may cause GI upset.
- Neuropathic pain: Some may experience nerve-related abdominal pain, particularly with rapid changes in blood glucose.
When stomach pain is persistent or severe, it is critical to work with healthcare providers to find the underlying cause.
Managing Stomach Pain in Type 1 Diabetes
Appropriate treatment depends on the underlying cause. Management strategies typically involve:
For Diabetic Ketoacidosis (DKA)
- Emergency insulin therapy: Restores proper glucose use and halts ketone production.
- Rehydration: IV fluids address dehydration and correct electrolyte imbalances.
- Identification of triggers: Treating infections or other contributing factors is critical.
For Gastroparesis
- Dietary changes:
- Eat smaller, more frequent meals.
- Favor soft, liquid, or blended foods that are easier to digest.
- Avoid high-fat and high-fiber foods, which slow digestion further.
- Careful blood sugar monitoring: Adjust insulin dosing and timing as stomach emptying may be unpredictable.
- Medications: Metoclopramide (may increase stomach contractions, but carries risks), erythromycin, and other options can be prescribed for nausea and motility.
- Severe cases: Rarely, feeding tubes or more invasive interventions may be needed for persistent, treatment-resistant gastroparesis.
For Other Causes
- Treat infections with appropriate medications.
- Address celiac disease with a gluten-free diet if diagnosed.
- Review all current medications with your healthcare team for GI side effects.
When to Seek Medical Attention
Stomach pain in T1D should never be ignored, especially if accompanied by any of the following:
- Persistent vomiting (over several hours)
- Severe pain or bloating
- Rapid breathing, drowsiness, or confusion
- Sugar and ketone levels outside your normal range
- Signs of dehydration (dry mouth, dark urine, dizziness)
- Unexplained weight loss or appetite changes
Prompt evaluation can prevent serious complications and help identify the right treatment strategy.
Tips for Preventing Stomach Pain in T1D
- Keep blood sugar levels within your target range whenever possible.
- Recognize early signs of hyperglycemia and DKA.
- Take insulin doses on time and check for device malfunctions if on a pump.
- Maintain regular follow-ups with your diabetes care team to monitor for complications.
- If you develop chronic digestive symptoms, discuss the possibility of gastroparesis with your doctor.
Frequently Asked Questions (FAQs) About Type 1 Diabetes and Stomach Pain
Q: Is stomach pain a common first symptom of type 1 diabetes?
A: No, stomach pain is not typically among the earliest symptoms, but it can develop during severe hyperglycemia or ketoacidosis and later as a complication.
Q: What should I do if I have stomach pain and diabetes?
A: Monitor your blood sugar and ketone levels immediately, and seek medical attention if you have severe symptoms, vomiting, or any signs of DKA.
Q: Can all people with T1D develop gastroparesis?
A: Not everyone, but up to 40-50% of people with long-term T1D may develop some form of delayed gastric emptying or gastroparesis.
Q: Can gastroparesis be cured?
A: Gastroparesis can be managed with dietary changes, medication, and careful blood sugar control, but it is not considered curable. Most people experience symptom relief with treatment.
Q: Does controlling my blood sugar help prevent stomach problems?
A: Yes, maintaining blood sugar within the recommended range can help prevent or minimize complications such as gastroparesis and DKA that lead to stomach pain.
Key Takeaways
- Stomach pain in type 1 diabetes may signal high blood sugar, DKA (a medical emergency), or chronic conditions like gastroparesis.
- DKA requires emergency treatment, while gastroparesis and other causes need careful long-term management with medication, diet, and blood sugar monitoring.
- Consult your healthcare provider for a personalized plan if you experience persistent or severe gastrointestinal symptoms.
References
- https://www.healthline.com/health/diabetes/type-1-diabetes-stomach-pain
- https://www.webmd.com/diabetes/diabetes-and-gastroparesis
- https://www.breakthrought1d.org/news-and-updates/complication-type-1-gastroparesis/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4521428/
- https://my.clevelandclinic.org/health/diseases/21500-type-1-diabetes
- https://www.cdc.gov/diabetes/signs-symptoms/index.html
- https://www.mayoclinic.org/diseases-conditions/type-1-diabetes/symptoms-causes/syc-20353011
- https://www.youtube.com/watch?v=gW07lSaNPdw
Read full bio of medha deb












