The Connection Between Type 1 Diabetes and Kidney Disease
Uncover how type 1 diabetes affects the kidneys, early signs, management, and prevention of diabetic kidney disease.
Type 1 diabetes is a complex autoimmune disease that frequently leads to other serious health complications, one of the most significant being chronic kidney disease. Understanding the link between type 1 diabetes and kidney disease is vital for early intervention, effective management, and prevention. This article provides a comprehensive overview of how type 1 diabetes can lead to kidney disease, symptoms to watch for, diagnostic approaches, available treatments, effects on life expectancy, and practical strategies to prevent progression.
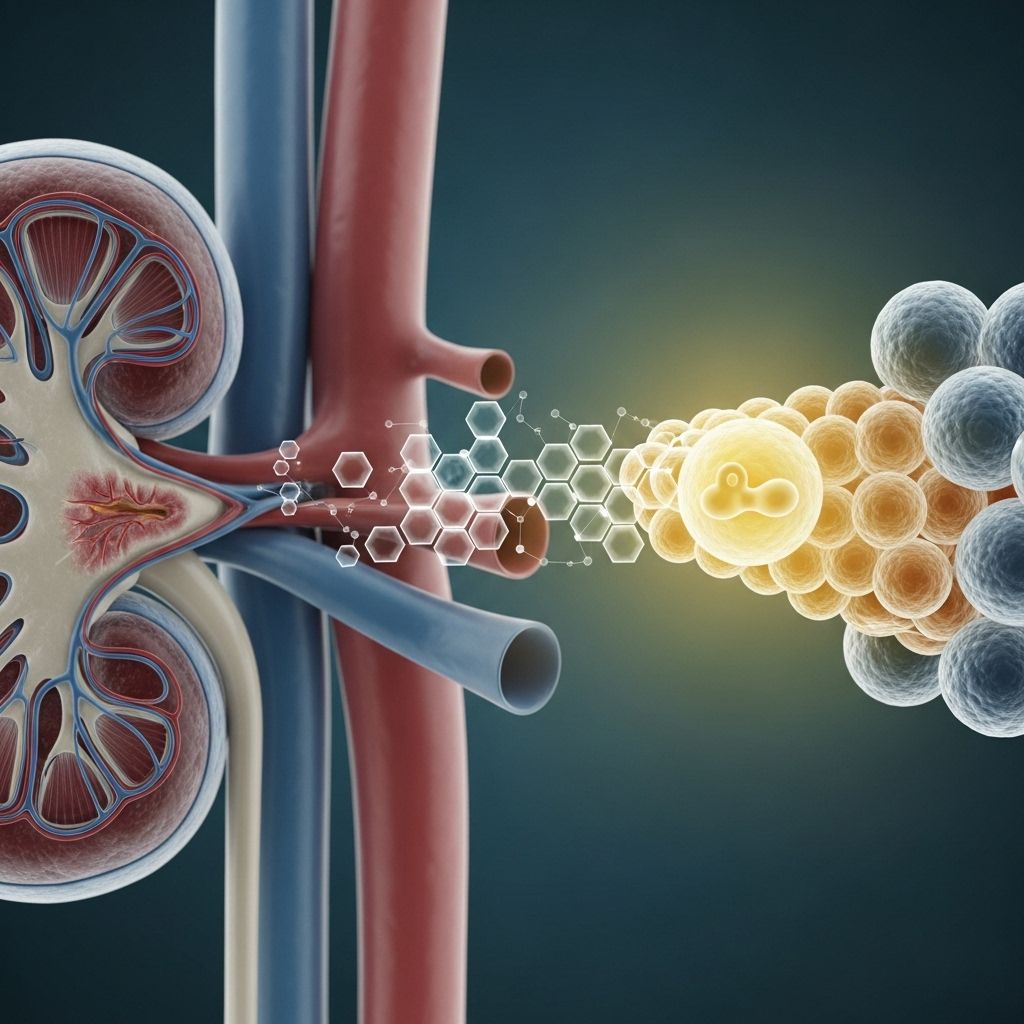
How Type 1 Diabetes Impacts the Kidneys
Kidneys play a crucial role in filtering waste products from the blood and maintaining the right balance of fluids and electrolytes. In type 1 diabetes, a lack of insulin disrupts blood sugar regulation, causing elevated glucose levels. Persistently high blood sugar can gradually damage the small blood vessels (nephrons) and other cells within the kidneys, impairing their ability to function properly.
- Microvascular Damage: High glucose levels damage small blood vessels in the kidneys, leading to a leakage of protein into urine—a condition called microalbuminuria.
- Loss of Filtering Ability: As more nephrons are damaged over time, the kidneys become less effective at filtering out waste, resulting in the buildup of toxins in the body.
- Progression to Chronic Kidney Disease (CKD): CKD develops gradually. In advanced stages, kidney function can become critically impaired, eventually leading to end-stage renal disease (ESRD), which may require dialysis or transplantation.
Studies report that 1 in 3 adults with diabetes develop some degree of CKD, making diabetes the leading cause of kidney disease in many countries.
Major Causes and Risk Factors
Not everyone with type 1 diabetes will develop kidney disease. Several factors increase the risk of developing diabetic kidney disease:
- Poor Blood Sugar Control: Chronic hyperglycemia accelerates kidney damage.
- High Blood Pressure: Hypertension adds further strain to kidney vessels, increasing damage risk.
- Genetics: A family history of kidney disease increases your susceptibility.
- Duration of Diabetes: The longer you have diabetes, the greater your risk of CKD.
- Other Factors: Smoking, obesity, and high cholesterol can also contribute to faster kidney decline.
| Risk Factor | Impact on Kidney Disease |
|---|---|
| Poor glycemic control | Increases risk of microvascular damage in kidneys |
| Hypertension | Strains kidney blood vessels, accelerating damage |
| Long duration of diabetes | More years of hyperglycemia raises risk |
| Family history | Genetic predisposition increases likelihood |
| Smoking | Reduces blood flow, accelerates nephron damage |
Symptoms of Diabetic Kidney Disease
Diabetic kidney disease can develop slowly and often shows no symptoms in the early stages. As the disease progresses, symptoms become more apparent, usually only after significant kidney damage has occurred.
- Swelling in the hands, ankles, feet, and around the eyes (fluid retention)
- Foamy or bubbly urine (proteinuria)
- Fatigue and weakness
- Nausea and loss of appetite
- Difficulty concentrating
- Changes in urination frequency or color
- Shortness of breath (as fluid builds up)
- High blood pressure (may worsen)
Because early-stage kidney disease is often silent, regular screening is essential for anyone living with type 1 diabetes.
When to Seek Medical Help
If you have type 1 diabetes, you should have an open dialogue with your healthcare provider regarding kidney health. Seek immediate medical attention if you notice:
- Swelling in your legs, ankles, or around your eyes
- Sudden changes in urination
- Unexplained fatigue or weakness
- Nausea, vomiting, or persistent loss of appetite
- Shortness of breath
These may be signs of progressing kidney involvement or other serious complications.
Diagnosis of Kidney Disease in Type 1 Diabetes
Early diagnosis can slow the progression of diabetic kidney disease and support better long-term outcomes.
- Annual Screening: People with type 1 diabetes for more than five years should undergo annual kidney function and urine protein tests.
- Urine Tests: Measure levels of albumin (a protein) to detect microalbuminuria or macroalbuminuria.
- Blood Tests: Assess glomerular filtration rate (GFR) and serum creatinine to evaluate kidney function.
- Blood Pressure Monitoring: High blood pressure can be both a cause and complication of kidney disease.
Early CKD usually starts with microalbuminuria; as it progresses, the amount of protein in the urine increases and GFR declines.
Treatment and Management Strategies
While kidney damage cannot be reversed, early intervention can significantly slow or halt progression. Treatment focuses on:
- Optimizing Blood Sugar Control: Consistent glucose management reduces further nephron damage.
- Managing Blood Pressure: Keeping blood pressure below 130/80 mmHg is strongly recommended.
- Medications:
- ACE inhibitors and ARBs—these help protect the kidneys even if you do not have high blood pressure.
- Other antihypertensive agents, if needed.
- Statins for cholesterol control.
- Healthy Lifestyle Choices:
- Eat a balanced, low-salt diet with adequate fruits, vegetables, and lean proteins
- Get regular exercise
- Maintain a healthy weight
- Avoid smoking and excess alcohol
- Regular Monitoring: Frequent blood and urine tests to track kidney health
- Dialysis or Kidney Transplant: For end-stage kidney disease, dialysis or transplantation may be necessary.
Table: Stages of Kidney Disease and Treatment Approaches
| Stage | eGFR (ml/min/1.73m2) | Key Features | Treatment Focus |
|---|---|---|---|
| 1 | >90 | Normal function, possible proteinuria | Blood sugar & BP control, lifestyle |
| 2 | 60-89 | Mild decline | Same as above, ACEi/ARB |
| 3 | 30-59 | Moderate decline | More frequent monitoring, med adjustments |
| 4 | 15-29 | Severe decline | Prepare for dialysis/transplant |
| 5 | <15 | End-stage | Dialysis or transplantation |
Life Expectancy and Quality of Life
Chronic kidney disease lowers life expectancy, especially if not managed effectively. When kidney disease progresses to end-stage, both dialysis and transplantation carry significant risks and impact quality of life. However, diligent control of blood sugar and blood pressure, plus healthy living, can help many people with diabetes and kidney disease lead longer, healthier lives.
Prevention: Protecting Your Kidneys When You Have Type 1 Diabetes
Proactive kidney care is essential for people with type 1 diabetes. Steps include:
- Carefully managing blood sugar with insulin and healthy eating
- Monitoring blood pressure and keeping it within target range
- Having annual kidney function tests as recommended
- Taking medications as prescribed for diabetes, blood pressure, and cholesterol
- Making lifestyle adjustments—such as quitting smoking, staying active, and maintaining a healthy weight
Frequently Asked Questions (FAQs)
How long does it take for type 1 diabetes to damage kidneys?
Kidney damage can begin as early as 2 to 5 years after a diabetes diagnosis, but it often takes longer to reach a stage where symptoms appear. Regular annual screening is recommended after five years with type 1 diabetes.
What is typically the first sign of diabetic kidney disease?
The first detectable sign is often protein in the urine (microalbuminuria). Visible symptoms, such as swelling in the hands, feet, or around the eyes due to fluid retention, can also appear as the disease progresses.
Can kidney damage from type 1 diabetes be reversed?
No, kidney damage cannot be reversed. However, with strict diabetes management and healthy lifestyle choices, further progression may be slowed or prevented. Early intervention is critical.
How does diabetes cause kidney failure?
Persistently high blood sugar damages tiny blood vessels in the kidneys, which impairs their ability to filter blood and leads to waste buildup. Over time, this can progress to kidney failure, requiring dialysis or transplant.
Does taking too much insulin damage kidneys?
Insulin itself does not directly harm the kidneys. However, insulin is necessary for controlling blood glucose, and inadequate blood sugar management (not excessive insulin) is what contributes to kidney damage.
Does type 2 diabetes affect the kidneys as well?
Yes, both type 1 and type 2 diabetes can cause kidney disease, as both conditions are associated with prolonged high blood sugar levels that harm kidney tissue.
Key Takeaways
- Kidney disease is a common complication of type 1 diabetes and develops gradually due to persistent high blood sugar.
- Early diagnosis is crucial—regular testing helps detect kidney damage before symptoms emerge.
- Optimal management of blood sugar and blood pressure is key to slowing the progression of kidney disease.
- Prevention strategies include healthy lifestyle, medication management, and regular screening.
If you have type 1 diabetes, discuss your individual kidney disease risk and preventive care plan with your healthcare provider.
References
- https://www.healthline.com/health/kidney-disease/type-1-diabetes-and-kidney-disease
- https://www.heart.org/en/health-topics/diabetes/diabetes-complications-and-risks/kidney-disease–diabetes
- https://diabetesjournals.org/care/article/45/12/3075/147614/Diabetes-Management-in-Chronic-Kidney-Disease-A
- https://www.kidney.org/kidney-topics/diabetes-and-kidney-disease-stages-1-4
- https://www.medicalnewstoday.com/articles/172179
- https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/diabetic-kidney-disease
- https://www.healthline.com/health/video/ckd-stages
- https://www.youtube.com/watch?v=XUnRopZmYJs
- https://aakp.org/programs-and-events/aakp-healthline/
Read full bio of Sneha Tete












