Twin-to-Twin Transfusion Syndrome (TTTS): Causes, Diagnosis, Treatment, and Outlook
Understand Twin-to-Twin Transfusion Syndrome (TTTS), a rare complication affecting identical twin pregnancies, its diagnosis, treatment, and long-term outcomes.

Twin-to-Twin Transfusion Syndrome (TTTS)
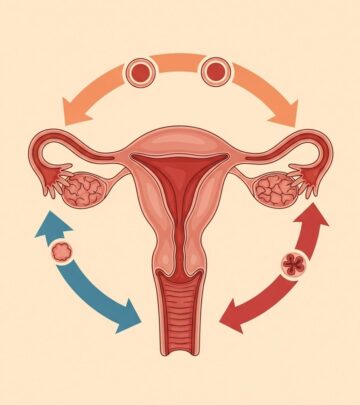
Twin-to-Twin Transfusion Syndrome (TTTS) is a rare but potentially life-threatening condition that can develop during pregnancy in identical twins who share a placenta. In TTTS, abnormal blood vessel connections within the shared placenta cause an uneven exchange of blood between the twins, putting both at significant health risks. Early recognition, close monitoring, and appropriate interventions greatly improve outcomes for both babies.
What is Twin-to-Twin Transfusion Syndrome?
TTTS is a complication seen exclusively in identical (monochorionic) twin pregnancies where both fetuses share a single placenta but have separate amniotic sacs. In about 10-15% of monochorionic twin pregnancies, an imbalance in blood supply develops through abnormally connected blood vessels in the placenta, leading to the condition known as TTTS.
In this syndrome:
- The donor twin provides some of its blood supply to the other fetus, resulting in reduced blood volume, less urine production, smaller bladder, and less amniotic fluid (oligohydramnios).
- The recipient twin receives excess blood, leading to increased blood volume, an enlarged bladder, excessive urine production, and too much amniotic fluid (polyhydramnios).
Without intervention, TTTS can progress quickly and may threaten the health or survival of one or both fetuses.
Who is at Risk?
TTTS is unique to monochorionic twin pregnancies, occurring when identical twins share a single placenta. The risk is not related to maternal actions, genetics, or environmental factors. Instead, it arises from the number and type of blood vessel connections in the shared placenta.
- Occurs in about 15% of monochorionic twin pregnancies.
- More likely in monochorionic-diamniotic twins—twins that share a placenta but each has its own amniotic sac.
- The condition is random and cannot be predicted or prevented by prenatal vitamins, diet, or any specific maternal activity.
Causes of TTTS
TTTS is caused by abnormal, imbalanced blood vessel connections—primarily arterio-venous anastomoses—in the shared placenta.
- Placental Blood Vessel Connections: In monochorionic twin placentas, it is normal to find vascular connections between the two fetal circulations. Typically, these are balanced; however, when the net flow of blood is unidirectional from one twin to the other, TTTS develops.
- Donor and Recipient Twin: The twin that loses blood (donor) becomes smaller and has a reduced amount of amniotic fluid, while the recipient twin becomes larger with excess amniotic fluid.
- Etiology Specifics: Donor twins experience hypovolemia (low blood volume), activating hormonal pathways that decrease urine production and shrink the bladder. Recipient twins develop hypervolemia (high blood volume), which can overwork their heart and cause excess urine production.
The precise trigger for why some pregnancies develop severe imbalances remains unknown, but it is not due to genetic defects or anything the parents did or did not do.
Symptoms and Presentation
The symptoms of TTTS manifest in both the mother and the developing fetuses. While there are often no signs or symptoms in the mother, in some cases, the following may be noticed:
- Rapid increase in belly size due to excessive amniotic fluid (polyhydramnios)
- Feeling out of proportion or more uncomfortable than expected for the stage of pregnancy
- Mild tightening or contractions in the uterus
On ultrasound, classic features of TTTS in twins include:
- One twin (donor) with a small or absent bladder and low amniotic fluid (oligohydramnios)—sometimes referred to as the “stuck twin” sign, where the baby is pressed against the wall of the uterus
- One twin (recipient) with a large bladder and excess amniotic fluid (polyhydramnios)
- Significant size difference between the twins as the donor slows in growth
- Possibility of heart strain or heart failure in the recipient twin due to blood volume overload
Diagnosis of TTTS
TTTS is typically diagnosed through prenatal ultrasound examinations during the second trimester.
- Initial clue is the observation that one twin has excess amniotic fluid while the other’s is low.
- Doppler ultrasound may reveal abnormal blood flow patterns in umbilical cord and vessel structures, as well as signs of heart strain in the recipient twin.
- Other features may include differences in bladder size and fetal growth patterns.
TTTS is most commonly detected between 16 and 26 weeks, but it can be diagnosed at any time after the first trimester. Regular and specialized monitoring is critical in monochorionic twin pregnancies to detect TTTS early.
Staging of TTTS
TTTS is classified into five stages according to the Quintero staging system:
| Stage | Description |
|---|---|
| Stage I | Minimal changes: Oligohydramnios in donor (<2 cm deepest pocket) and polyhydramnios in recipient (>8 cm deepest pocket for <20wks, >10cm >20wks), bladder in donor is visible |
| Stage II | Donor bladder no longer visible on ultrasound, but Dopplers are not yet abnormal |
| Stage III | Abnormal Doppler studies (absent/reversed flow in umbilical artery, ductus venosus, or umbilical vein pulsations) |
| Stage IV | Presence of hydrops (fluid buildup in one or both twins) |
| Stage V | Demise (death) of one or both twins |
This staging helps inform the urgency and choice of treatment.
Treatment Options for TTTS
Treatment approaches for TTTS depend on severity, stage, gestational age, and overall health of the mother and fetuses. Management is best performed by a fetal medicine specialist experienced in high-risk twin pregnancies.
- Close Monitoring: Mild cases (Stage I) may only require intensive monitoring with frequent ultrasounds and exams.
- Amnioreduction: Removal of excess amniotic fluid from the recipient twin’s sac through a needle (akin to amniocentesis) for symptom relief and to reduce preterm labor risk. This does not treat the underlying blood vessel abnormality but can manage symptoms.
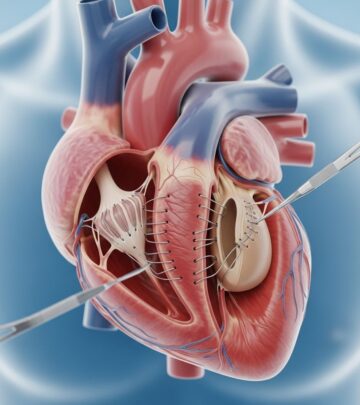
- Laser Photocoagulation of Placental Vessels: The gold-standard treatment for moderate to severe cases. A fetoscope (tiny camera with a laser) is inserted through the mother’s abdomen to directly view the placenta and seal off abnormal blood vessel connections. This procedure corrects the root cause and improves outcomes for both twins.
- Septostomy: Creating a small hole in the shared amniotic membrane to balance fluid levels. This is less commonly used.
- Early Delivery: If the pregnancy is far enough along and the babies’ survival is more likely, delivery may be recommended.
Close observation is often required even after treatment, as recurrences or new complications can occur.
Risks, Prognosis, and Complications
The outcomes in TTTS depend on several factors, including the severity of the syndrome, gestational age at diagnosis and intervention, and whether effective treatment is available.
- Without treatment, severe TTTS has a survival rate below 10% for both twins.
- After treatment, particularly laser therapy, 60-70% will have both twins survive, and about 85-90% will have at least one baby survive.
- Premature birth is a frequent complication, as increased amniotic fluid puts pressure on the cervix.
- Recipient twins can suffer heart problems due to fluid and blood overload; donor twins are at risk for growth restriction and organ damage from low blood flow.
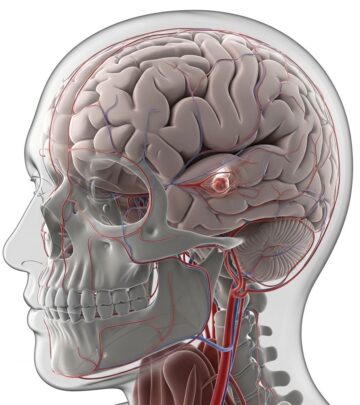
- After birth, surviving twins may face short- or long-term issues such as neurological injury, heart defects, or kidney problems.
With timely diagnosis and advanced treatment at specialized centers, the majority of TTTS pregnancies now result in at least one healthy surviving baby, and many have two healthy survivors.
Living with a TTTS Diagnosis: What Parents Need to Know
Learning that your twins may have TTTS can be overwhelming, but early intervention offers a greatly improved outlook today compared with the past. Key things for parents to keep in mind include:
- Frequent Monitoring: Expect rigorous and regular ultrasounds and specialist appointments for close assessment.
- Expert Care: Seek care at a facility with experience in fetal surgery and complicated twin pregnancies whenever possible.
- Emotional Support: Connecting with resources, support groups, and care teams can help families manage the uncertainty and emotional impact.
- After Birth: Surviving twins may need NICU care, and ongoing follow-up will be important, especially in the first years.
Frequently Asked Questions (FAQs)
What causes TTTS?
TTTS is caused by abnormal blood vessel connections in the placenta of monochorionic twins, resulting in unbalanced blood flow. It is not caused by the mother’s actions, genetics, or anything the parents did or did not do.
Can TTTS be prevented?
No. There is currently no way to prevent TTTS, but regular ultrasounds and monitoring in high-risk twin pregnancies improve the chances of early detection and treatment.
How is TTTS different from other twin complications?
TTTS is unique to identical twins who share a single placenta with abnormal blood vessel connections. It is different from growth discordance due simply to nutrient distribution, and from complications seen in fraternal twins (who each have their own placenta).
Is TTTS always fatal?
No. TTTS can be life-threatening if severe and untreated. However, with timely diagnosis and effective treatment (especially laser therapy), the majority of affected pregnancies now result in the survival of at least one child, and often both.
What is the long-term outlook for twins who survive TTTS?
Many twins treated for TTTS have healthy, normal development, especially if the condition is detected early and managed promptly. Some twins may experience long-term complications, particularly if the condition was severe, prolonged, or resulted in preterm birth. Long-term follow-up and support are key.
Key Takeaways
- TTTS is a rare but serious disorder occurring only in monochorionic (identical) twin pregnancies.
- It arises from abnormal blood flow across shared placental vessels, leading to life-threatening differences in fluid and blood volume between twins.
- Early diagnosis, intensive monitoring, and specialized treatments such as laser therapy significantly improve the prognosis.
- Comprehensive follow-up and support are crucial for optimal outcomes for both babies and families.
Resources for Further Information
- Fetal therapy centers with experience in TTTS
- Neonatal intensive care teams for postnatal management
- Support and advocacy groups for parents and families coping with TTTS
References
- https://www.ncbi.nlm.nih.gov/books/NBK563133/
- https://fetus.ucsf.edu/ttts/
- https://www.ssmhealth.com/cardinal-glennon/fetal-care-institute/fetal-conditions-we-treat/twin-abnormalities/twin-to-twin-transfusion-syndrome
- https://www.nationwidechildrens.org/conditions/twin-to-twin-transfusion-syndrome
- https://my.clevelandclinic.org/health/diseases/22985-twin-to-twin-transfusion-syndrome
- https://www.childrenscolorado.org/conditions-and-advice/conditions-and-symptoms/conditions/twin-to-twin-transfusion-syndrome-ttts/
- https://www.yalemedicine.org/conditions/twin-to-twin-transfusion-syndrome
- https://www.mayoclinic.org/medical-professionals/obstetrics-gynecology/news/laser-therapy-for-twin-twin-transfusion-syndrome-offers-best-outcomes/mac-20509521
Read full bio of Sneha Tete