Trigeminal Neuralgia: Symptoms, Causes, and Modern Treatment Solutions
Understanding facial pain, diagnosis, and the latest advances in treatments for trigeminal neuralgia—the facial nerve disorder.
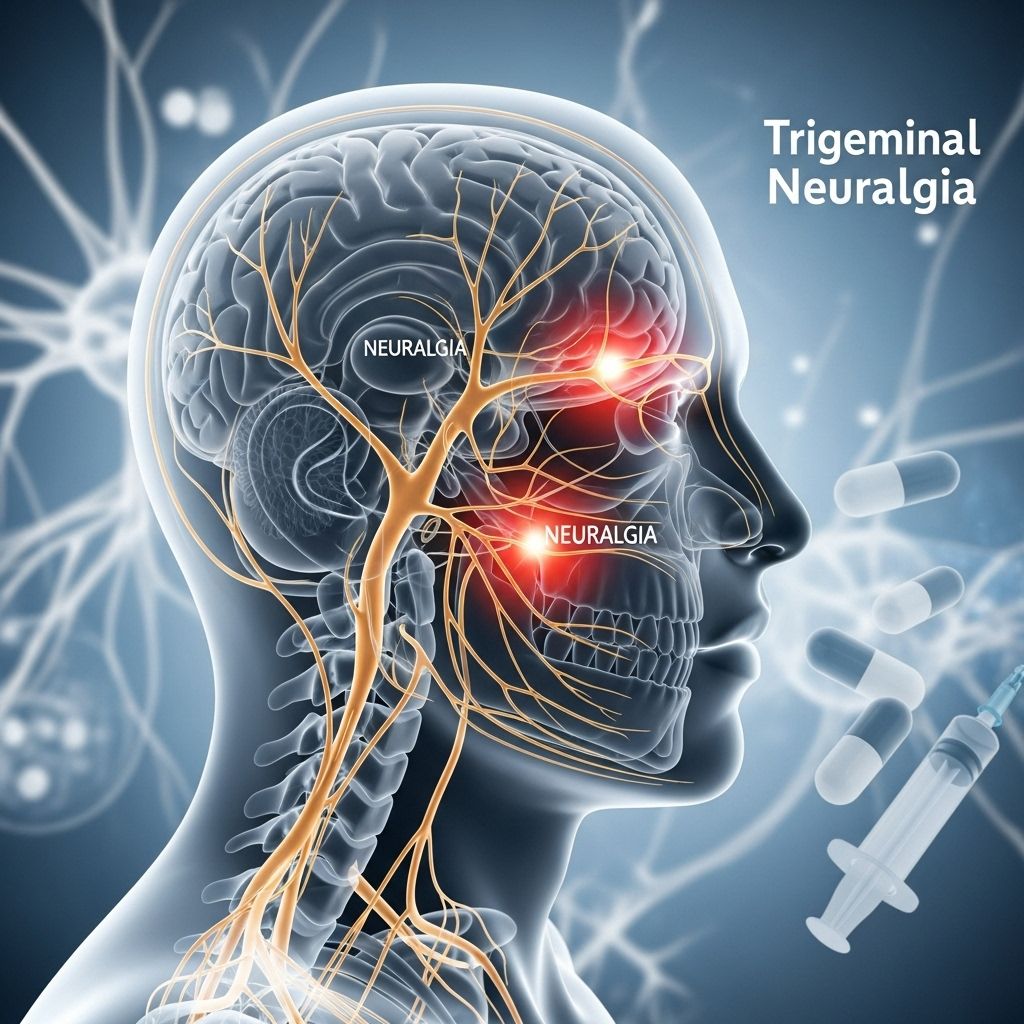
Trigeminal neuralgia is a chronic and sometimes debilitating condition characterized by severe facial pain. Affecting the trigeminal nerve—a critical nerve that transmits sensations from the face to the brain—this disorder can drastically reduce quality of life. Timely diagnosis and the implementation of effective treatment strategies are essential for those living with trigeminal neuralgia.
What is Trigeminal Neuralgia?
Trigeminal neuralgia (TN) is a nerve disorder that causes sudden, severe, electric shock-like or stabbing facial pain. The pain typically involves the lower face and jaw, although it can affect areas around the nose and above the eye. TN is often chronic, meaning it can recur over months or years, sometimes with periods of remission in between attacks.
- Pain is generally unilateral (on one side of the face).
- The condition can be triggered by everyday activities such as brushing teeth, eating, or even a light touch.
- Although not life-threatening, TN can have a profound impact on daily living, emotional wellbeing, and social interactions.
Understanding the Trigeminal Nerve
The trigeminal nerve is the fifth cranial nerve and is primarily responsible for transmitting sensations from the face to the brain. It has three branches:
- Ophthalmic (V1): provides sensation to the forehead and eye area.
- Maxillary (V2): supplies the cheek and upper jaw region.
- Mandibular (V3): covers the lower jaw and chin.
Pain from trigeminal neuralgia can affect any or all of these branches but most often involves the maxillary and mandibular branches.
What Causes Trigeminal Neuralgia?
Several factors can irritate or damage the trigeminal nerve, leading to episodes of extreme pain.
- Vascular compression: Most commonly, a blood vessel sits against and compresses the nerve, wearing away its protective myelin sheath and causing errant pain signals.
- Multiple sclerosis (MS): In people with MS, demyelination (damage to myelin sheath) may affect the trigeminal nerve and trigger symptoms even without vessel compression.
- Tumors: Rarely, a tumor and not a blood vessel causes the nerve compression.
- Other causes: Traumatic injuries, arteriovenous malformations, or other neurological conditions may also provoke TN.
| Potential Cause | Description |
|---|---|
| Vascular Compression | Contact by a nearby artery or vein causes damage to the nerve’s myelin sheath. |
| Multiple Sclerosis | Degenerative nerve sheath disease impairs pain signal control. |
| Tumor | Rarely, compression caused by a tumor at the nerve’s root. |
| Facial Trauma | Injuries or surgical interventions may disturb the nerve directly. |
Who is at Risk for Trigeminal Neuralgia?
While TN can affect anyone, certain factors may increase the risk:
- Age: Most cases occur in people over 50 years old.
- Sex: Women are affected more frequently than men.
- Family History: Rarely, a genetic tendency for the disorder may exist.
- Neurological Conditions: Individuals with MS are at higher risk.
What are the Symptoms of Trigeminal Neuralgia?
Pain from TN is unique in its intensity, duration, and presentation. Some distinguishing features include:
- Sudden onset: Pain occurs abruptly and typically lasts a few seconds to two minutes per episode.
- Unilateral facial pain: Usually affects just one side of the face at a time.
- Trigger points: Activities like smiling, chewing, talking, shaving, or even wind blowing on the face can precipitate an attack.
- Attack frequency: Episodes may happen, stop, and then recur, sometimes increasing in frequency and intensity over time.
- Burning, stabbing, or electric shock-like pain: The pain can be sharp and excruciating, often described as a ‘lightning bolt’ sensation.
Between episodes, some people may experience a dull aching sensation or sensitivity in the affected area.
How is Trigeminal Neuralgia Diagnosed?
Diagnosis of TN is primarily clinical, based on history and neurological examination. However, several steps are involved to ensure accuracy:
- Medical History: Detailed discussion of symptom onset, duration, character, and triggers of pain.
- Physical and Neurological Exams: Checking facial muscle function, reflexes, and sensation.
- Imaging Tests: Magnetic Resonance Imaging (MRI) or Computed Tomography (CT) scans to look for blood vessel compression, tumors, or demyelinating lesions.
- Rule Out Other Conditions: Excluding disorders such as dental problems, temporomandibular joint (TMJ) syndrome, cluster headaches, or sinus issues.
Sometimes, a diagnosis is confirmed through response to medications specifically effective for TN, such as carbamazepine.
How is Trigeminal Neuralgia Treated?
The primary goal of treatment is to alleviate pain and improve function. Treatment may involve medications, minimally invasive procedures, or surgery.
Medications
- Anti-seizure drugs (anticonvulsants): Carbamazepine is the first-line medication; other options include oxcarbazepine, lamotrigine, and phenytoin. These drugs quiet nerve activity and reduce pain signals.
- Muscle relaxants: Baclofen may be prescribed alone or with anticonvulsants, offering additional pain relief in some cases.
- Nerve pain medications: Gabapentin and pregabalin can be considered, particularly if the pain does not respond to standard therapy.
- Botox injections: Emerging evidence suggests botulinum toxin injections may be beneficial for some patients with medication-resistant TN.
Drug side effects may include dizziness, drowsiness, nausea, or allergic reactions. Adjustments or alternative therapies may be required if medication alone is insufficient.
Surgical Procedures
Surgery is considered if medications fail to provide relief or if side effects become intolerable. There are various procedural options with different risk profiles and durations of efficacy:
- Microvascular decompression (MVD): The most definitive surgical treatment. MVD involves moving or removing the blood vessel compressing the trigeminal nerve root. It is effective in many cases but is a form of open brain surgery.
- Rhizotomy procedures (lesioning): Intentionally damage the pain-transmitting fibers of the nerve to provide relief. These include glycerol injection, balloon compression, and radiofrequency thermal lesioning.
- Gamma Knife radiosurgery: Uses focused radiation to damage the nerve and stop pain signals, offering a non-invasive alternative to surgery.
| Procedure | Description | Pros | Cons |
|---|---|---|---|
| Microvascular decompression | Moves/removes blood vessel from nerve | Long-lasting relief; treats root cause | Requires open surgery; anesthesia risks |
| Balloon compression | Inflates balloon to compress nerve at base of skull | Minimally invasive | Often causes facial numbness; relief may be temporary |
| Glycerol injection | Injects sterile glycerol to damage nerve | Office-based procedure | Temporary numbness, possible recurrence |
| Radiofrequency lesioning | Heats nerve fibers to block pain | Targeted and effective | May need repetition; facial numbness |
| Gamma Knife radiosurgery | Focused radiation on nerve | Non-invasive; outpatient basis | Relief can take weeks/months; numbness possible |
Managing Trigeminal Neuralgia Triggers
Identifying and avoiding triggers is critical for individuals managing TN:
- Avoid strong wind or drafts on the face.
- Use a soft-bristled toothbrush; use lukewarm water when washing the face.
- Chew on the unaffected side; avoid cold or very hot beverages.
- Practice gentle stretching and relaxation techniques.
Living with Trigeminal Neuralgia
TN can lead to emotional and psychological challenges, including anxiety and depression. Self-care, lifestyle adjustments, and emotional support play vital roles in improving everyday life for those living with TN.
- Work closely with your healthcare team to adjust treatments as needed.
- Seek support groups or counseling to cope with chronic pain.
- Monitor medication side effects and report them to your provider.
- Maintain regular gentle physical activity to improve general health and mood.
Frequently Asked Questions (FAQs)
What does trigeminal neuralgia feel like?
Trigeminal neuralgia typically causes sudden, severe, electric shock-like or stabbing pain, usually on one side of the face. Pain attacks last from a few seconds to two minutes and occur multiple times a day or week.
What triggers trigeminal neuralgia pain?
Pain can be triggered by everyday activities such as eating, talking, brushing teeth, shaving, or even light touch and wind on the face.
Is trigeminal neuralgia curable?
TN can often be effectively managed, but long-term cure depends on the underlying cause and treatment strategy. Many patients experience significant relief with medications and/or surgery.
Can trigeminal neuralgia go away on its own?
TN often occurs in episodes, so remission is possible. However, the condition tends to return without treatment, and symptoms can become more frequent and intense over time.
Who diagnoses and treats trigeminal neuralgia?
Trigeminal neuralgia is usually diagnosed and treated by neurologists and neurosurgeons, in consultation with pain specialists and primary care doctors.
Are there any complications with treatments?
Some treatments, particularly surgery and nerve-based procedures, may cause facial numbness, weakness, or—rarely—infection or anesthesia risks. Medication side effects may include drowsiness, imbalance, or allergic reactions.
When Should You Seek Medical Attention?
If you experience unexplained, severe facial pain—especially if it recurs—see a healthcare provider as soon as possible. Early evaluation helps rule out other serious conditions and offers access to effective treatment, improving your quality of life.
Conclusion
Trigeminal neuralgia is a challenging but manageable disorder with a complex array of causes and symptoms. With advances in diagnosis and treatment, most people can substantially reduce their pain and resume normal activities. Effective care often requires collaboration between the individual, healthcare providers, and personal support systems.
References
- https://ufhealth.org/stories/2023/understanding-trigeminal-neuralgia-symptoms-causes-and-treatment-options
- https://www.mayoclinic.org/diseases-conditions/trigeminal-neuralgia/diagnosis-treatment/drc-20353347
- https://www.healthdirect.gov.au/trigeminal-neuralgia
- https://www.aans.org/patients/conditions-treatments/trigeminal-neuralgia/
- https://my.clevelandclinic.org/health/diseases/15671-trigeminal-neuralgia-tn
- https://www.mayoclinic.org/diseases-conditions/trigeminal-neuralgia/symptoms-causes/syc-20353344
- https://www.nhs.uk/conditions/trigeminal-neuralgia/treatment/
- https://www.uchealth.org/diseases-conditions/trigeminal-neuralgia/
Read full bio of Sneha Tete












