Treatment Options for Peripheral Artery Disease (PAD): Comprehensive Guide
Explore the latest therapies, lifestyle changes, medications, and procedures for effectively managing Peripheral Artery Disease (PAD).
Treatment Options for Peripheral Artery Disease (PAD)
Peripheral artery disease (PAD) is a common circulatory condition in which narrowed arteries reduce blood flow to the limbs, resulting in symptoms such as leg pain, numbness, and increased risk of cardiovascular complications. Effective management of PAD is vital for improving quality of life and reducing the risk of severe complications such as heart attack and stroke. While PAD cannot be completely cured, a combination of lifestyle changes, medications, and surgical procedures can help control symptoms and slow disease progression.
Understanding PAD and Its Impact
PAD develops due to the buildup of fatty deposits, or plaque, inside arteries that carry blood to your legs and feet. As circulation declines, muscles and tissues don’t get enough oxygen, which can lead to pain and other issues. If left untreated, PAD may progress to critical limb ischemia or increase the risk of cardiovascular events.
Lifestyle Modifications for PAD Management
Making healthy lifestyle choices is the cornerstone of PAD treatment, especially in early and moderate disease stages. The goal is to improve vascular health, minimize risk factors, and slow the progression of arterial narrowing.
- Quit Smoking: Smoking is the leading modifiable risk factor for PAD. Quitting smoking substantially improves circulation and reduces the risk of heart attack and stroke.
- Eat a Heart-Healthy Diet: Focus on whole grains, fresh fruits, vegetables, lean proteins, and healthy fats (such as avocado and olive oil). Limit sodium, cholesterol, trans fats, and added sugars to help manage blood pressure and cholesterol levels.
- Exercise Regularly: Moderate, consistent physical activity enhances circulation, helps manage weight, and improves overall cardiovascular health. Walking programs, supervised exercise therapy, and aerobic exercise are recommended.
- Maintain a Healthy Weight: Achieving or maintaining a healthy body mass index (BMI) reduces stress on the cardiovascular system and enhances mobility.
- Limit Alcohol Intake: Reduce or eliminate alcohol consumption to further lower cardiovascular risk.
- Manage Stress: Chronic stress can adversely affect heart health, so stress-management techniques such as yoga, meditation, and relaxation exercises can be beneficial.
Physical Activity for PAD
Exercise, especially walking, is shown to improve PAD symptoms by encouraging development of collateral blood vessels and increasing the distance a person can walk without pain. Supervised exercise programs are often more effective, helping people safely increase activity while monitoring symptoms.
- Walking until mild discomfort, resting, and repeating for up to 30–60 minutes most days
- Participation in structured cardiac rehabilitation programs
- Consistent light-to-moderate exercise to build endurance and muscular strength
Medications for PAD
Medications are recommended to manage PAD symptoms, control underlying risk factors, and prevent complications. The specific drug regimen depends on individual needs, comorbidities, and symptom severity.
- Antiplatelet Agents: Aspirin or clopidogrel are commonly prescribed to reduce the risk of blood clots and lower the likelihood of heart attacks and strokes.
- Cholesterol-Lowering Drugs: Statins like atorvastatin or simvastatin help reduce plaque buildup by lowering LDL cholesterol.
- Blood Pressure Lowering Agents: ACE inhibitors, beta-blockers, and calcium channel blockers are used to manage high blood pressure, a major risk factor for PAD and cardiovascular events.
- Medications to Improve Pain-Free Walking: Cilostazol and pentoxifylline may be prescribed to improve walking distance and reduce leg pain.
- Diabetes Management: Strict glucose control is crucial for PAD patients with diabetes.
Common PAD Medications Table
| Medication | Purpose | Common Side Effects |
|---|---|---|
| Aspirin / Clopidogrel | Reduce blood clot risk | Bleeding, gastrointestinal discomfort |
| Statins | Lower LDL cholesterol | Muscle pain, liver enzyme changes |
| ACE Inhibitors | Lower blood pressure | Cough, dizziness |
| Cilostazol | Improve walking ability | Headache, diarrhea |
| Pentoxifylline | Reduce leg pain | Nausea, dizziness |
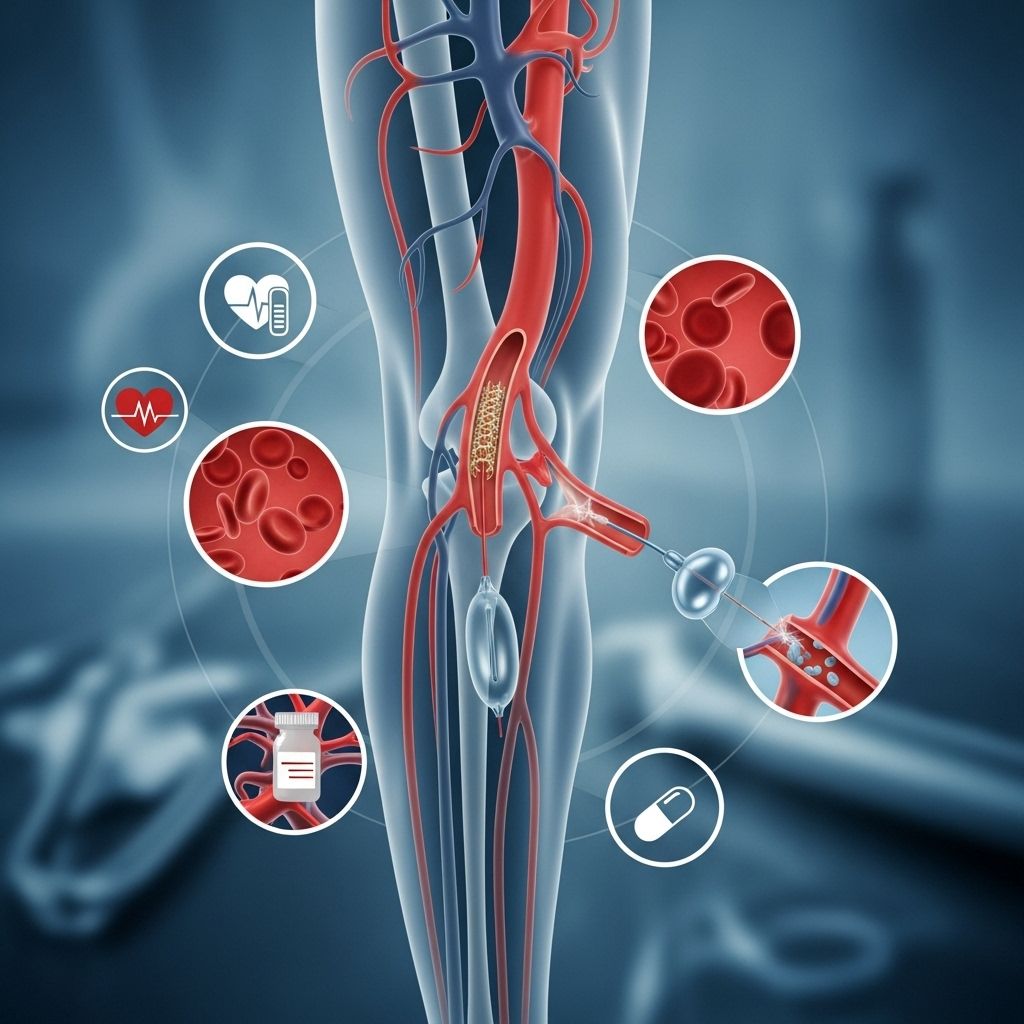
Surgical and Invasive Procedures for PAD
When symptoms are severe or do not improve with conservative management, surgical or minimally invasive treatments may be recommended. These interventions aim to restore blood flow to affected limbs and reduce the risk of tissue damage.
- Angioplasty and Stenting: Balloon angioplasty widens narrowed arteries, and stents are placed to keep arteries open. This minimally invasive procedure improves circulation quickly with a short recovery time.
- Atherectomy: This procedure removes plaque from inside arteries using a special device. It may be combined with angioplasty or stenting.
- Arterial Bypass Surgery: Bypass grafting creates an alternative pathway for blood to flow around blocked arteries using a vessel from another part of the body. This is reserved for severe blockages that cannot be treated with less invasive methods.
- Endarterectomy: Surgical removal of plaque from artery walls; less common but can be effective for short, localized blockages.
- Amputation: In rare cases where circulation cannot be restored and tissue death occurs, amputation of the affected limb or part may be necessary to protect overall health.
Comparing PAD Surgical Procedures
| Procedure | Purpose | Typical Recovery |
|---|---|---|
| Angioplasty/Stenting | Open narrowed arteries | 1–2 days |
| Arterial Bypass | Redirect blood flow around blockage | 1–2 weeks |
| Atherectomy | Remove built-up plaque | 1–3 days |
| Endarterectomy | Excise arterial plaque | 2–5 days |
| Amputation (if needed) | Remove irreversibly damaged tissue | 1–3 weeks |
Managing Complications and Follow-Up Care
PAD increases the risk of life-threatening complications, including heart attack, stroke, and limb loss. Effective management requires ongoing medical supervision, regular check-ups, and adherence to prescribed therapies. Cardiovascular risk factors such as hypertension, diabetes, and high cholesterol should be closely monitored and controlled.
- Routine follow-up visits to assess symptoms and medication side effects
- Monitoring blood pressure, cholesterol, and blood glucose levels
- Screening for signs of worsening limb ischemia, such as non-healing wounds or increasing pain
- Prompt attention to any signs of infection or tissue damage
- Communication with healthcare providers about any new symptoms or concerns
Frequently Asked Questions (FAQs) about PAD Treatment
Q: Can PAD be completely cured?
A: PAD cannot be cured or reversed, but its symptoms and progression can be managed effectively through lifestyle changes, medications, and, if necessary, procedures.
Q: How important is exercise in treating PAD?
A: Exercise is crucial in managing PAD. Regular walking or supervised activities help improve circulation, reduce symptoms, and build endurance.
Q: Are there any foods I should avoid with PAD?
A: Avoid foods high in saturated fats, trans fats, sodium, and added sugars. Emphasize fruits, vegetables, lean proteins, and whole grains for heart health.
Q: What are the risks associated with PAD procedures?
A: Risks vary by procedure but may include infection, bleeding, or blood clots. Most procedures are safe when performed by experienced teams, and risks are minimized with careful pre- and post-operative care.
Q: How often should I see my doctor if I have PAD?
A: Follow your doctor’s recommendations, which typically involve routine visits every 3–6 months, or sooner if symptoms worsen or complications develop.
Key Takeaways in PAD Management
- Lifestyle modification is the foundation of PAD treatment and can greatly improve vascular health.
- Medications are necessary to manage risk factors and symptoms, and your regimen may change over time.
- Minimally invasive and surgical treatments are available for severe PAD or when conservative methods fail.
- Ongoing monitoring is essential to prevent complications and ensure optimal results from treatment.
- Multidisciplinary care—including your cardiologist, vascular surgeon, and primary care provider—can help address all aspects of the disease and comorbidities.
Additional Resources for PAD Patients
- American Heart Association: PAD patient guides
- Society for Vascular Surgery: PAD educational materials
- Cardiac rehabilitation centers: Supervised exercise programs
- Patient support groups: Connecting with others living with PAD
References
- https://www.healthline.com/health/heart-disease
- https://www.healthline.com/health/coronary-artery-disease/coronary-artery-disease-treatments
- https://lifeprogram.org.au/health-hub/earlysignsofheartdiseaseinmen/
- https://www.medicalnewstoday.com/articles/237191
- https://www.cedars-sinai.org/newsroom/healthline-therapy-vs-antidepressants–which-is-best-for-people-with-heart-disease/
- https://www.healthline.com/health/video/how-to-prevent-heart-disease-according-to-a-cardiologist
- https://www.healthline.com/health/video/a-busy-persons-guide-to-better-heart-health-in-2025
- https://www.healthline.com/health/video/how-to-lower-cholesterol
- https://www.uc.edu/news/articles/legacy/healthnews/2007/02/uc-health-line–what-women-need-to-know-about-heart-attacks.html
Read full bio of medha deb












