Treating Coronary Artery Disease: Approaches, Medications, and Lifestyle
Learn about comprehensive strategies for managing coronary artery disease, from lifestyle changes and medication to procedures and ongoing care.
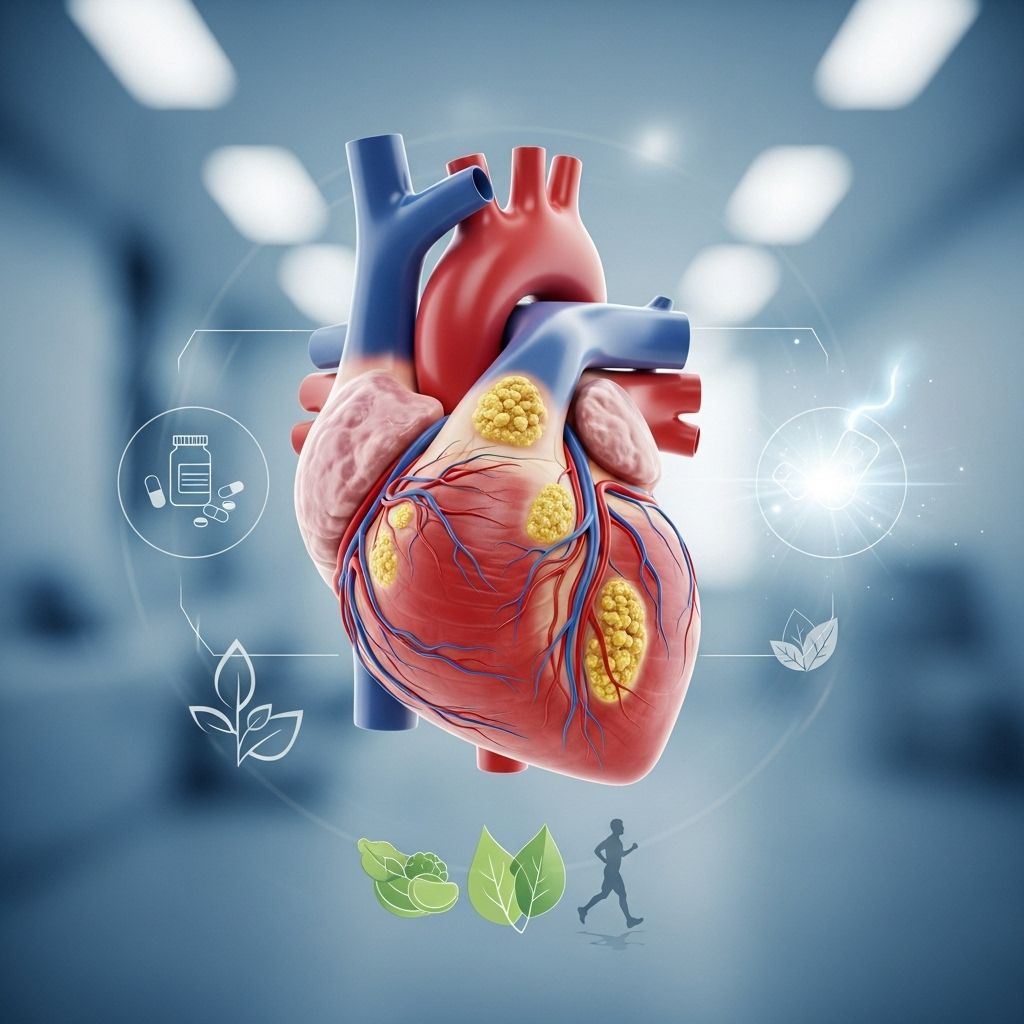
Coronary artery disease (CAD) remains one of the leading causes of illness and death around the globe. Though it has no cure, modern medicine offers a diverse toolkit for managing its symptoms, reducing risk, and improving quality of life. Treatment is most effective when tailored to individual needs, combining lifestyle changes, medications, and, when necessary, medical procedures. This article explores the full landscape of CAD treatment options, with guidance for making choices in partnership with your healthcare provider.
Understanding Coronary Artery Disease
CAD develops when plaque—composed of cholesterol, fat, calcium, and other substances—builds up in the coronary arteries, restricting blood flow to the heart muscle. The resulting decrease in oxygen supply can lead to chest pain (angina), shortness of breath, and, when blood flow becomes critically low, heart attacks. Treatment focuses on slowing the progression of atherosclerosis (plaque formation), managing symptoms, and preventing complications such as heart attack or heart failure.
Lifestyle Changes to Manage CAD
Adopting and maintaining heart-healthy habits forms the first line of defense against CAD progression and complications. These modifications can lower blood pressure and cholesterol, reduce strain on the heart, and alleviate many risk factors that worsen the disease. Key lifestyle changes include:
- Quit smoking: Smoking damages blood vessels, accelerates plaque buildup, and increases the risk of heart attack and stroke. Quitting is one of the most significant steps you can take for heart health.
- Adopt a heart-healthy diet: Focus on foods rich in fruits, vegetables, whole grains, lean proteins (such as fish and skinless poultry), legumes, and healthy fats (like those found in avocados, olive oil, and nuts). Reduce intake of saturated and trans fats, simple sugars, red meats, and salt.
- Be physically active: Engage in moderate-intensity exercise (such as brisk walking or swimming) for at least 30 minutes most days of the week, as approved by your healthcare provider.
- Achieve and maintain a healthy weight: Excess body weight increases strain on the heart and is linked to elevated cholesterol, blood pressure, and risk of diabetes.
- Get enough sleep: Aim for 7–9 hours of quality sleep nightly to support cardiovascular health and overall well-being.
- Manage stress: Relaxation techniques such as yoga, meditation, deep breathing, or counseling can help control stress that may aggravate heart disease.
Benefits of Lifestyle Change
- Lowers blood pressure and cholesterol levels.
- Reduces the risk of heart attack, stroke, and cardiac events.
- Improves overall quality of life.
- May reduce dependence on medications over time.
Medications for Managing CAD
Medications play an essential role in managing CAD, targeting several underlying factors, from high cholesterol and blood pressure to blood clot risk and symptoms like angina. Your doctor will develop a medication plan personalized to your unique risk factors, age, and overall health.
Types of Medications Used in CAD
| Medication Type | Purpose | Potential Side Effects |
|---|---|---|
| Statins | Lower LDL (“bad”) cholesterol and slow plaque buildup. | Muscle pain, weakness, digestive problems, headaches, dizziness, sleep issues. |
| Beta-blockers | Reduce blood pressure, slow heart rate, lessen heart’s oxygen demand, lower risk after heart attack. | Dizziness, fatigue, cold extremities, gastrointestinal issues. |
| Blood thinners (e.g., aspirin, anticoagulants) | Reduce blood clot risk, preventing heart attacks and strokes. | Bleeding, bruising, stomach upset. |
| ACE inhibitors | Lower blood pressure, improve outcomes in people with CAD, support heart function. | Cough, dizziness, elevated blood potassium. |
| Calcium channel blockers | Relax and widen blood vessels, lower blood pressure, slow heart rate. | Swelling, constipation, fatigue. |
| Nitroglycerin (patches, sprays, tablets) | Relieve angina by dilating blood vessels and reducing heart workload. | Headache, flushing, dizziness. |
Some people may need to try different medicine combinations or dosages to find the most effective regimen with manageable side effects. Always report new or worsening symptoms to your doctor.
Medical Procedures to Treat Coronary Artery Disease
For those whose arteries are significantly narrowed or blocked, or whose symptoms are not controlled with medications and lifestyle changes, procedures may be required to restore adequate blood flow to the heart. Several options are available, each tailored to the severity of the disease and the patient’s overall health.
Percutaneous Coronary Intervention (PCI) / Angioplasty
Often called angioplasty, PCI is a minimally invasive procedure in which a thin, flexible tube (catheter) with a balloon on the tip is inserted into an artery and guided to the blockage. The balloon is inflated to compress plaque against the artery wall and improve blood flow. Most often, a tiny wire mesh tube called a stent is inserted to keep the artery open.
- Benefits: Less invasive, quick recovery (usually same-day or next-day discharge), immediate symptom relief.
- Risks: Bleeding, vessel damage, restenosis (recurrence of narrowing), allergic reaction to contrast dye.
Coronary Artery Bypass Grafting (CABG)
CABG, or heart bypass surgery, may be recommended for severe blockages or multiple affected arteries. In this major operation, a healthy blood vessel from the leg, arm, or chest is used to create a new route for blood to flow around the blocked arteries.
- Benefits: Long-term improvement in blood flow, relief from angina, reduction in risk of heart attack and death in certain populations.
- Risks: Infection, bleeding, reaction to anesthesia, long recovery time (usually 5 days or more in hospital), memory or cognitive changes.
Coronary Endarterectomy
This surgical technique is sometimes combined with CABG for people with severe, diffuse plaque in their arteries and persistent angina. The surgeon removes plaque from the artery wall to improve blood flow. It is reserved for the most complex blockages not managed with stents or bypass alone.
Heart Transplant
For individuals with end-stage CAD unresponsive to other treatments, a heart transplant may be considered. This involves replacing the damaged heart with one from a healthy donor. Transplants are uncommon and considered only when the heart is severely weakened and the person is otherwise healthy enough for surgery and lifelong immune suppression.
Alternative and Complementary Approaches
Some individuals explore alternative therapies to complement conventional treatment. These may include specific vitamins, nutritional supplements, acupuncture, or mind–body techniques. While some approaches—such as omega-3 fatty acids—may offer cardiovascular benefits, most alternative therapies are not substitutes for established treatments. Always consult your doctor before adding supplements or alternative therapies, as they may interact with prescribed medications or cause side effects.
Cardiac Rehabilitation and Ongoing Recovery
If you have suffered a heart attack, undergone heart surgery, or have advanced CAD, cardiac rehabilitation is highly recommended. Cardiac rehab is a medically supervised program designed to help you recover, regain strength, and reduce the risk of recurrent events. The typical program includes:
- Personalized exercise training to improve cardiovascular fitness.
- Education about heart health, nutrition, and safe physical activity.
- Guidance on managing medications and lifestyle risk factors.
- Emotional and psychological support to deal with anxiety, depression, or stress related to heart disease.
Most cardiac rehab programs last about 12 weeks and are covered by insurance if prescribed by your doctor. Participation can significantly reduce your risk of stroke, future heart attacks, depression, and cardiac death.
Long-Term Management: Living Well with CAD
Chronic diseases like CAD require ongoing management, regular check-ups, and active engagement in self-care. In addition to medication and lifestyle adherence, be sure to:
- Keep routine appointments with your healthcare team.
- Monitor blood pressure, cholesterol, and blood sugar if advised.
- Report any new or worsening symptoms, such as chest pain, shortness of breath, or swelling in the legs.
- Ask your doctor about vaccinations that help protect your heart, such as annual flu shots or pneumococcal vaccines.
Complications of Untreated CAD
If unmanaged, CAD can lead to serious, potentially fatal complications:
- Heart attack (myocardial infarction): Occurs if a coronary artery becomes fully blocked by a blood clot. Emergency treatment is required to minimize heart muscle damage and save lives.
- Heart failure: The heart is too weak or stiff to pump blood effectively, leading to symptoms such as fatigue, swelling, and shortness of breath.
- Arrhythmias: Abnormal heart rhythms that can cause palpitations, dizziness, or fainting.
- Sudden cardiac death: A catastrophic event resulting from abrupt loss of heart function.
Early diagnosis, regular monitoring, and diligent management are vital to lower your risk of these life-threatening outcomes.
Frequently Asked Questions (FAQs)
Q: Can coronary artery disease be cured?
No, CAD cannot be cured, but with treatment and lifestyle measures, many people can manage symptoms, slow or stop progression, and enjoy an active life.
Q: What are early warning signs of CAD?
Early signs may include chest pain (angina), shortness of breath, pain in the arms or jaw, or increased fatigue with exertion. Many people have no symptoms until a blockage causes a heart attack.
Q: How often should I see my doctor if I have CAD?
Appointments depend on symptoms and disease severity, but regular check-ups—at least annually, or more frequently if recommended—are crucial to monitor risk factors and adjust treatment.
Q: Are there natural treatments for CAD?
While certain lifestyle habits (like healthy eating and exercise) are “natural” ways to manage CAD, other alternative therapies should never replace prescribed medicine or procedures. Consult your doctor before starting supplements or herbs.
Q: What are the risks of advanced CAD medical procedures?
Procedures such as angioplasty and bypass surgery, while generally safe and effective, do carry risks like bleeding, infection, blood clots, or—rarely—stroke or heart attack. All procedures should be discussed in detail with your cardiologist to understand individual benefits and risks.
Key Takeaways
- CAD is a chronic condition best managed through a mix of lifestyle changes, medications, and medical procedures tailored to individual risk.
- Core strategies include quitting smoking, improving diet, increasing physical activity, and carefully managing blood pressure and cholesterol.
- Multiple medication classes—statins, beta-blockers, blood thinners, ACE inhibitors—address different aspects of the disease and risk factors.
- Severe or unresponsive CAD may require procedures such as PCI, coronary artery bypass, or, in rare cases, a heart transplant.
- Ongoing cardiac rehabilitation, regular check-ups, and attention to new symptoms are critical to long-term success.
Discuss your personal risk and options with your doctor to create an effective, individualized treatment plan. Early action and consistent management can make a profound difference in your heart health and longevity.
References
- https://www.webmd.com/heart-disease/coronary-artery-disease
- https://www.healthline.com/health/coronary-artery-disease/coronary-artery-disease-treatments
- https://www.medicalnewstoday.com/articles/184130
- https://www.healthline.com/health/coronary-artery-disease
- https://www.healthline.com/health/video/how-to-prevent-heart-disease-according-to-a-cardiologist
- https://www.medicalnewstoday.com/articles/237191
- https://www.cedars-sinai.org/newsroom/healthline-therapy-vs-antidepressants–which-is-best-for-people-with-heart-disease/
- https://www.healthline.com/health/video/a-cardiologist-explains-what-your-diet-does-to-your-heart
Read full bio of medha deb












