Torticollis (Wryneck): Causes, Symptoms, Diagnosis, and Treatment
A comprehensive guide to understanding, diagnosing, and managing torticollis (wryneck) in children and adults.
Torticollis, also known as wryneck, is a condition marked by an abnormal, often painful, twisting or tilting of the neck. This comprehensive guide explores the types, signs, underlying causes, diagnostic strategies, and available treatment options for torticollis, offering evidence-based insights for both congenital and acquired forms.
What Is Torticollis (Wryneck)?
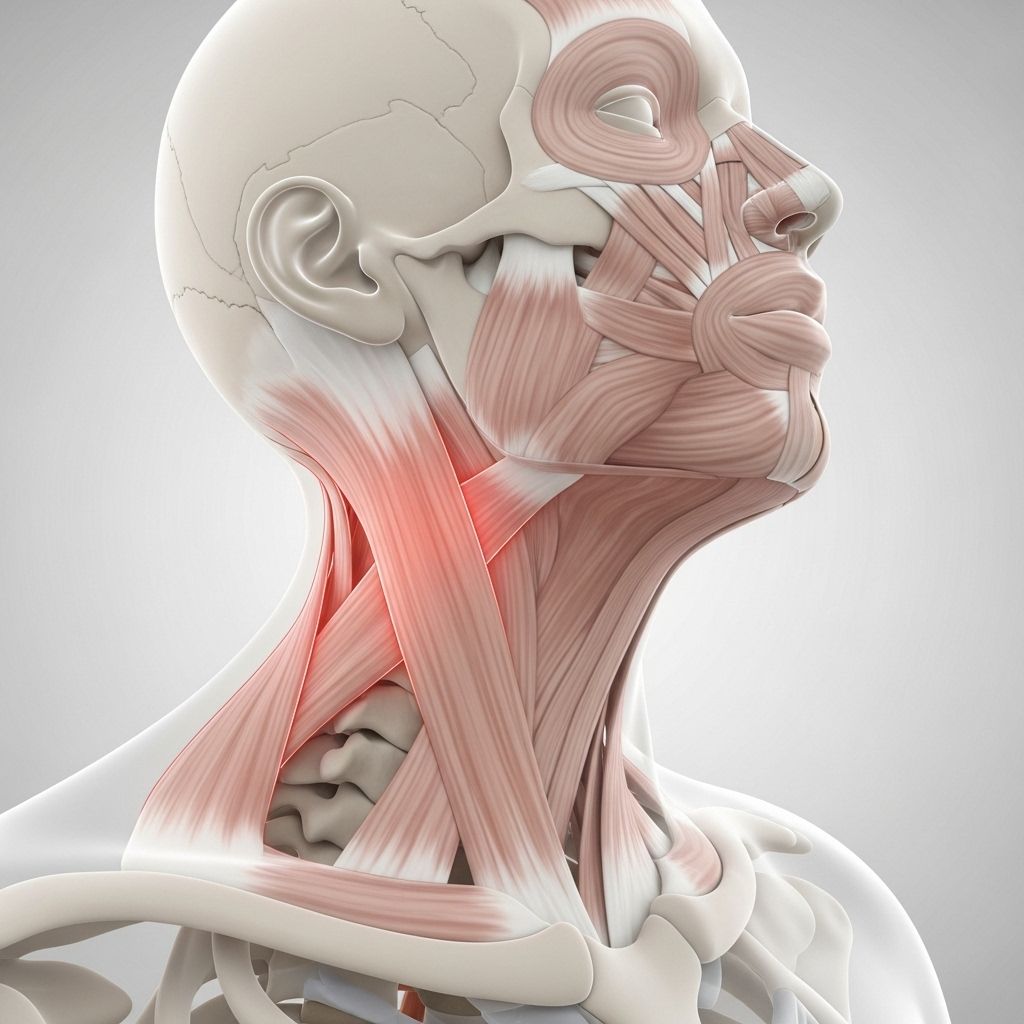
Torticollis is a musculoskeletal condition in which the neck muscles contract involuntarily or are tight, causing the head to rotate, tilt, or twist to one side. The term “wryneck” describes the visual effect—an angled or rotated position of the head and neck. Torticollis may be present at birth (congenital) or develop later (acquired), and it can range in severity from mild discomfort to significant restriction in neck movement and persistent pain.
Types of Torticollis
- Congenital Muscular Torticollis – Results from shortening or tightness of the sternocleidomastoid muscle, typically noticed soon after birth. Commonly caused by fetal positioning or birth trauma.
- Acquired Torticollis – Develops after birth due to muscle spasm, injury, infection, or neurological disease. Acquired cases are varied in cause and often occur in children and adults of any age.
- Temporary (Benign Paroxysmal) Torticollis – Sudden onset of neck spasm, typically resolving on its own within days to a week. Sometimes related to minor injury or sleeping awkwardly.
- Spasmodic Torticollis (Cervical Dystonia) – A rare, chronic neurological disorder where neck muscles contract uncontrollably, causing the head to twist or turn to one side.
Who Is at Risk?
Torticollis can affect people of any age, but certain groups are more susceptible:
- Newborns and infants (for congenital forms)
- Children and adolescents (often temporary, post-injury or infection)
- Adults exposed to trauma, muscle strain, or medication side effects
- Individuals with a family history of muscular or neurological conditions
Causes of Torticollis
- Congenital Causes
- Abnormal infant positioning in the womb
- Birth trauma to neck muscles or blood supply
- Associated congenital conditions (e.g., hip dislocation)
- Acquired Causes
- Muscle or ligament injury in the neck
- Sleeping in an awkward position
- Infections (e.g., throat or ear infection causing secondary muscle spasm)
- Side effects of certain medications or drug toxicity
- Inflammation, such as due to viral or bacterial infection
- Herniated disk or slipped vertebral facet
- Tumors or abscesses causing nerve or muscle disturbance
- Neurological disorders or genetic factors
- Unknown (idiopathic torticollis, when no specific cause is found)
Signs and Symptoms
The primary symptom of torticollis is an abnormal head or neck position. Additional signs vary depending on the underlying cause and duration:
- Pain and tightness on one side of the neck
- Head tilting toward one side and chin turning to the opposite side
- Reduced ability to move the head and neck
- Neck muscle spasms and tenderness
- Stiffness in the neck and shoulders
- Asymmetry of the face and skull in infants (plagiocephaly)
- In children, persistent crying or irritability and feeding difficulties
- In severe cases: fever, difficulty swallowing or breathing, drooling, weakness or numbness in limbs
Special note: Symptoms like fever, increased drooling, difficulty swallowing, visual changes, or limb weakness can be signs of serious underlying problems and require urgent medical assessment.
When to Seek Medical Attention
While torticollis is often benign and self-resolving, certain circumstances demand immediate evaluation:
- Sudden and severe neck pain
- Difficulty breathing, swallowing, or persistent drooling
- Blue or gray discoloration of lips or skin
- Weakness, numbness, or loss of coordination in arms or legs
- Loss of bladder or bowel control
- Progressive worsening of pain or stiffness
- Fever or symptoms of infection
How Is Torticollis Diagnosed?
Diagnosis of torticollis involves a detailed medical history and thorough physical examination. Steps may include:
- Medical History: Review of symptom onset, duration, recent injuries, infections, medication use, and family history.
- Physical Examination: Assessment for head and neck position, muscle tightness, movement limitations, and neurological signs.
- Imaging (if needed):
- X-rays to detect bone abnormalities or trauma
- Ultrasound (especially in infants) to assess muscle structure
- MRI or CT scan when underlying neurological or structural disorders are suspected
- Blood Tests: Used to evaluate infection or metabolic causes, typically if presenting symptoms suggest infection or inflammatory disease.
Treatment Options for Torticollis
Treatment strategies depend on the type (congenital or acquired), cause, and severity of symptoms. Most cases improve with conservative therapy, particularly if addressed early. The key goals are to relieve muscle spasm and pain, restore normal neck function, and prevent long-term complications.
Non-Surgical Treatment Approaches
- Medications: Analgesics, anti-inflammatories, and muscle relaxants to reduce pain and spasm.
- Botulinum toxin injections: For resistant cases (especially spasmodic torticollis), injections can reduce abnormal muscle contractions.
- Physical Therapy:
- Gentle stretching and strengthening exercises
- Positioning, massage, and supervised movement to improve range of motion
- Parental instruction for home exercises in infants
- Heat and Cold Compresses: Applied to ease muscle spasms and improve comfort.
- Massage: Relief of muscle tightness and pain.
- Neck Braces: Short-term use in some acute cases to support the neck and relieve spasm. Should only be used under medical supervision.
- Antibiotics: For cases stemming from infection (e.g., associated throat or ear infection).
Surgical and Advanced Interventions
- Surgical Correction: Reserved for rare, severe cases unresponsive to therapy (often congenital torticollis). Surgery can release or lengthen the affected neck muscle.
- Management of Underlying Causes: Treatment of tumors, bone abnormalities, neurological conditions, or other contributing factors as appropriate.
Prognosis and Potential Complications
- Most cases of acquired (especially acute) torticollis resolve within 7-10 days with conservative treatment.
- Early intervention in congenital torticollis often leads to full recovery with normal head position and function.
- Delay in treatment, particularly in infants and children, can result in persistent head tilt, facial asymmetry (plagiocephaly), and delays in motor development.
- Chronic or untreated spasmodic torticollis in adults may result in persistent pain and difficulty with daily tasks.
Prevention and Self-Care Strategies
- Minimize risk of neck injury by maintaining proper posture and ergonomics.
- Practice safe sleeping positions to avoid neck strain.
- Follow recommended stretching and physical activity routines, especially after trauma or extended immobility.
- Seek prompt treatment for infections of the head and neck region to reduce risk of secondary torticollis.
- For babies: Encourage tummy time and supervised repositioning to prevent fixed neck postures and flat spots on the head.
Living with Torticollis: Support and Adaptation
- Support from physiotherapists, occupational therapists, and pediatricians is key to optimal recovery for children.
- Consistent home exercises foster improvement and prevent recurrence.
- Adaptive devices, such as pillows or neck supports, may aid comfort during acute flares.
Frequently Asked Questions (FAQs)
Q: Is torticollis a permanent condition?
A: Most cases of torticollis, especially when detected and treated early, are temporary and resolve completely. Chronic cases may persist, especially in neglected or severe neurological causes.
Q: Can torticollis recur?
A: Yes. There is a risk of recurrence, particularly in cases of spasmodic torticollis or when underlying causes are not fully addressed. Consistent therapy can reduce this risk.
Q: Are infants with torticollis at risk for developmental delays?
A: Untreated congenital torticollis can lead to motor development delays and craniofacial asymmetry. Early therapy and parental guidance are vital to minimize risks.
Q: When should I seek emergency care for torticollis?
A: Emergency care is warranted for symptoms such as breathing difficulty, severe neck pain, limb weakness, sudden loss of coordination, or signs of systemic infection (e.g., high fever).
Q: What is the long-term outlook for children with congenital torticollis?
A: With early and consistent physical therapy, the outlook is generally excellent. Most children regain full range of neck motion and normal appearance.
Quick Reference: Torticollis Overview
| Aspect | Description |
|---|---|
| Common Names | Torticollis, Wryneck, Twisted Neck |
| Key Symptoms | Neck pain, head tilt, reduced mobility, spasm |
| Types | Congenital, Acquired, Spasmodic |
| Main Causes | Birth injury, awkward posture, infection, injury |
| Main Treatments | Physical therapy, medication, botulinum toxin, surgery (rare) |
| Prognosis | Generally favorable with prompt treatment |
Resources and Support
- Consult your medical provider for a customized evaluation and treatment plan.
- Pediatric therapists and support groups for families dealing with congenital torticollis.
- National organizations and health info portals for further education.
References
- https://www.ummhealth.org/health-library/torticollis-wry-neck
- https://www.healthline.com/health/torticollis
- https://www.urmc.rochester.edu/encyclopedia/content?contenttypeid=85&contentid=p01389
- https://www.healthdirect.gov.au/torticollis
- https://my.clevelandclinic.org/health/diseases/22430-torticollis
- https://orthoinfo.aaos.org/en/diseases–conditions/congenital-muscular-torticollis-twisted-neck
- https://www.childrenshospital.org/conditions/torticollis
- https://patient.info/bones-joints-muscles/neck-pain/torticollis-twisted-neck
Read full bio of Sneha Tete