Understanding TNM Staging in Lung Cancer: A Comprehensive Overview
Explore how the TNM system classifies lung cancer and guides critical treatment decisions.
Understanding TNM Staging in Lung Cancer
Lung cancer remains one of the most prevalent and serious cancers worldwide. Accurate staging is crucial for determining a patient’s prognosis and the best treatment approach. One of the universally adopted systems for staging lung cancer is the TNM staging system. This article provides a detailed overview of TNM staging, its components, how it differs from other methods, and what it means for people diagnosed with lung cancer.
What Is the TNM Staging System?
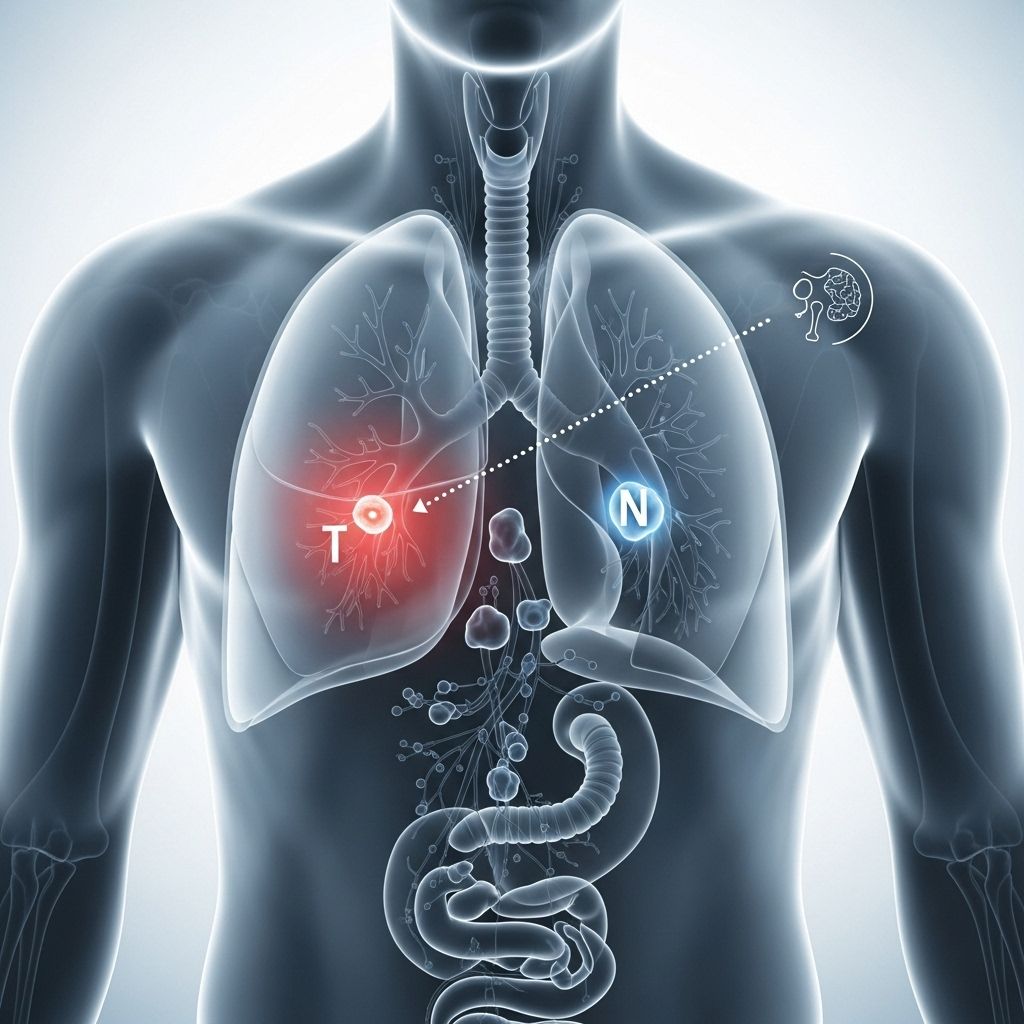
The TNM system is a standardized method used by oncologists to describe the extent and severity of many types of cancer, including lung cancer. The letters TNM stand for:
- T—Tumor: Describes the size and extent of the primary tumor.
- N—Node: Indicates whether cancer has spread to the nearby lymph nodes.
- M—Metastasis: Specifies whether the cancer has spread to distant organs or tissues.
Each component is assigned a number or letter to denote the degree of cancer involvement. The higher the number, the more advanced the disease. Once the TNM values are determined, they are grouped into stages that help guide treatment and estimate prognosis.
Breaking Down the TNM Categories
Tumor (T)
The T category provides information about the primary lung tumor:
- T0: No evidence of a primary tumor
- Tis: Carcinoma in situ (very early cancer that has not spread)
- T1: Tumor is 3 cm or less and surrounded by lung or visceral pleura (the membrane covering the lung) with no invasion of major airways
- T2: Tumor greater than 3 cm but not more than 5 cm, or involves main bronchus, invades visceral pleura, or is associated with atelectasis (lung collapse)
- T3: Tumor more than 5 cm but not more than 7 cm, or directly invades the chest wall, diaphragm, phrenic nerve, or contains separate tumor nodules in the same lobe
- T4: Tumor more than 7 cm, invades mediastinal organs (heart, great vessels, trachea, esophagus, vertebral body), or involves separate tumor nodules in a different ipsilateral lobe
The T category is essential as it defines the primary tumor’s dimensions and relationship to nearby structures, which impacts potential treatment options like surgery or radiotherapy.
Node (N)
The N category describes if and where the cancer has spread to lymph nodes:
- NX: Lymph nodes cannot be assessed
- N0: No cancer in regional lymph nodes
- N1: Cancer in lymph nodes within the lung or in the area where the lungs join the airway (hilum)
- N2: Cancer in lymph nodes in the center of the chest (mediastinum) on the same side as the affected lung, or below the carina (where the windpipe branches)
- N3: Cancer in lymph nodes on the opposite side of the chest, above the collarbone, or at the top of the lung
Assessing lymph node involvement is vital for accurately staging the cancer and determining whether more aggressive therapy is needed.
Metastasis (M)
The M category assesses whether cancer has spread from the lungs to distant organs or tissues:
- M0: Cancer has not spread to other parts of the body
- M1: Cancer has spread to distant organs or tissues, such as the liver, brain, bones, or other lobe(s) of the lung. The M1 category has further sub-stages:
- M1a: Cancer is in both lungs, in the pleural lining (lining around lungs or heart), or there is fluid around the lung/heart with cancer cells (malignant effusion)
- M1b: Single area of cancer outside the chest, such as in an organ (like the liver or brain) or lymph node
- M1c: Multiple areas of cancer in one or several organs
The presence or absence of metastasis is critical for determining if the cancer can be treated with curative intent, or if therapies will be focused on prolonging life and alleviating symptoms.
How Doctors Use TNM Staging in Lung Cancer
The information gathered from the T, N, and M categories helps healthcare providers:
- Predict prognosis: Higher stages generally correspond to a worse prognosis.
- Guide treatment: Surgery, chemotherapy, radiation, or palliative care may be recommended based on staging.
- Facilitate communication: Using standardized terms allows doctors to discuss cases more clearly.
- Design clinical trials: Grouping by stage ensures patients in research studies are comparable.
Once the T, N, and M values are determined, they are combined into stage groupings (stages 0 through IV) to give an overall picture of the cancer’s extent:
| Overall Stage | Description |
|---|---|
| Stage 0 | Tis, N0, M0 (carcinoma in situ, earliest stage) |
| Stage I | Small, localized tumor with no lymph node involvement or metastasis |
| Stage II | Larger tumor or limited lymph node spread, no distant metastasis |
| Stage III | More extensive tumor or broader lymph node involvement, but no distant metastasis |
| Stage IV | Tumor with distant metastasis (M1), may be in both lungs, pleural lining, or distant organs |
Clinical vsPathologic Staging
There are two main ways to determine the stage of lung cancer:
- Clinical Stage: Based on physical examination, imaging (CT, PET, MRI), and biopsy results before any surgery.
- Pathologic (Surgical) Stage: Determined by examining tissues removed during surgery; sometimes reveals additional cancer involvement.
The pathologic stage is considered more accurate, but many patients are staged clinically if surgery is not performed.
Updates in TNM Staging: The Eighth Edition
The TNM staging system is periodically updated to reflect new research and patterns in cancer recurrence and outcomes. The eighth edition of TNM staging for lung cancer introduced several adjustments, primarily to tumor size categories and metastasis descriptors. It is based on large international databases and is now widely used by cancer centers around the world.
Some key updates in the eighth edition include:
- More refined tumor size distinctions that impact the T category (e.g., changes at 1-cm size intervals).
- Detailed breakdown of metastatic disease (M1a, M1b, M1c) to aid in better prognosis and treatment distinction.
- Lymph node (N) classification remains consistent with previous editions.
Why Are Staging Revisions Important?
Updates help clinicians better stratify risk, tailor therapies, and compare outcomes worldwide. Accurate staging through the latest TNM guidelines ensures the best possible treatment planning for every patient.
TNM Staging Compared to Other Lung Cancer Staging Methods
The TNM system is the primary method used for both non-small cell lung cancer (NSCLC) and, increasingly, small cell lung cancer (SCLC). Previously, SCLC was divided only into:
- Limited-stage: Cancer confined to one side of the chest and within a radiation field
- Extensive-stage: Cancer spread beyond one side or to other organs
The TNM system provides more detailed information, aiding both treatment and research efforts for all lung cancer types.
Why Is Accurate Staging So Important?
Knowing the accurate stage of lung cancer allows clinicians and patients to:
- Identify the most effective therapies (such as surgery for early-stage disease or chemotherapy for advanced stages)
- Enrol in clinical trials suitable for their cancer stage
- Discuss prognosis more accurately
- Avoid unnecessary or ineffective treatments
How Is TNM Staging Determined?
Doctors use a variety of tools and tests to determine the TNM stage, including:
- Physical exams and clinical history
- Imaging studies such as chest X-rays, CT scans, PET scans, and MRI
- Biopsy of lung tissue or lymph nodes
- Laboratory tests (blood tests, pleural fluid analysis)
- Surgery in selected cases to directly assess tissues
The combination of these findings allows doctors to assign the appropriate T, N, and M categories and an overall stage.
Summary Table: TNM Staging at a Glance
| TNM Component | Description | Clinical Relevance |
|---|---|---|
| Tumor (T) | Size of the tumor and local invasion | Guides surgical resectability choices; informs radiation planning |
| Node (N) | Regional lymph node involvement | Determines need for systemic therapy and further imaging |
| Metastasis (M) | Presence and extent of spread to distant organs | Marks a shift from curative to palliative treatment strategies |
Frequently Asked Questions (FAQs)
What does each letter in TNM mean?
T stands for the size and extent of the primary tumor, N for spread to nearby lymph nodes, and M for whether the cancer has metastasized (spread) to distant body sites.
How does TNM staging influence treatment?
Cancer stage influences decisions on surgery, chemotherapy, radiation, or a combination. Early stages may be curable with surgery or local therapies. Higher stages require systemic treatments and often focus on prolonging survival and quality of life.
Can TNM staging change over time?
Yes. If additional findings emerge after surgery or during treatment (such as cancer being more widespread than initially thought), the stage may be updated.
Is TNM staging the same worldwide?
The TNM system is a universally accepted staging system, but local guidelines or resources may introduce small variations in interpretation or practice. Most international cancer centers follow the latest edition of the TNM staging guidelines.
What if I have multifocal lung cancer?
Multiple tumor sites may be staged separately or collectively, depending on whether they represent distinct primary cancers or spread from a single tumor. This situation is complex and evaluated case by case.
Is the TNM system used for all types of lung cancer?
Yes. While previously small cell lung cancer was often staged simply as limited or extensive, most modern guidelines recommend using the TNM system for all types, including NSCLC and SCLC.
Key Takeaways
- The TNM system offers a detailed, standardized way to stage lung cancer, essential for treatment planning.
- “T” assesses tumor size and invasion; “N” assesses lymph node involvement; “M” records distant metastases.
- Updates to staging, such as those in the eighth edition, improve patient stratification and outcomes.
- Staging is determined using imaging, biopsies, and sometimes surgery; accurate staging is critical for personalized care.
If you or someone you love has been diagnosed with lung cancer, ask your care team to explain the TNM components and overall stage, and how that influences your treatment options and outlook.
References
- https://www.cancerresearchuk.org/about-cancer/lung-cancer/stages-types/tnm-staging
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6058324/
- https://www.cancer.org/cancer/types/lung-cancer/detection-diagnosis-staging/staging-nsclc.html
- https://radiologyassistant.nl/chest/lung-cancer/tnm-classification-8th-edition-1
- https://www.lungevity.org/patients-care-partners/navigating-your-diagnosis/lung-cancer-staging
- https://www.mdanderson.org/cancer-types/lung-cancer/lung-cancer-stages.html
Read full bio of Sneha Tete












