Essential Tips for Managing Diabetic Macular Edema
Comprehensive guidance on identifying, treating, and living with diabetic macular edema to protect your vision and quality of life.
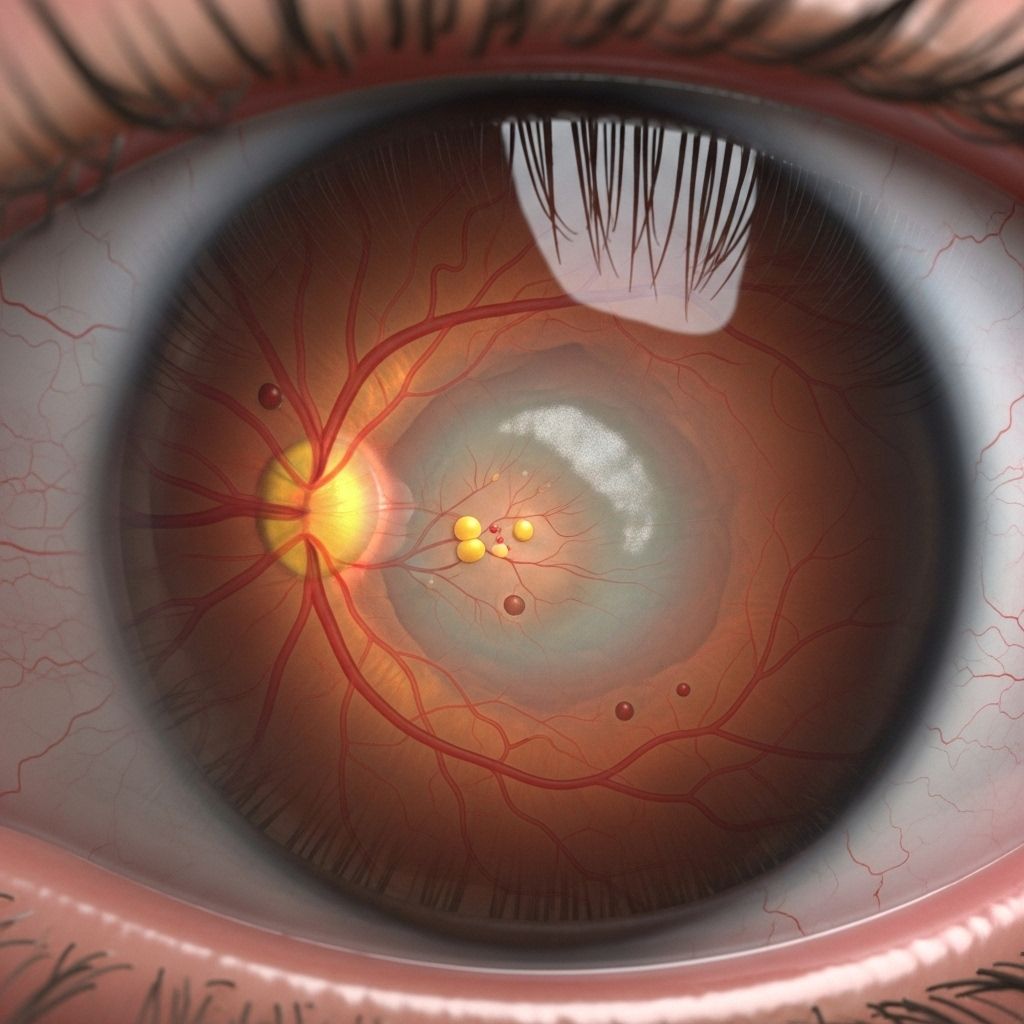
Diabetic macular edema (DME) is a vision-threatening complication of diabetes that results from swelling in the macula, the part of the retina responsible for sharp, central vision. Managing DME effectively requires a blend of medical treatments, lifestyle choices, and ongoing support to minimize vision loss and maintain a high quality of life. Below you’ll find a comprehensive guide to understanding DME, recognizing its symptoms, exploring treatment options, and learning how to live well with DME.
What Is Diabetic Macular Edema?
Diabetic macular edema (DME) is a complication that arises when chronic high blood sugar from diabetes damages small blood vessels in the retina, leading to leakage of fluid in the macula. The swelling diminishes the ability to see fine details, causing central vision loss that can interfere significantly with daily activities.
- Cause: Damage to retinal blood vessels due to diabetes, resulting in fluid accumulation in the macula.
- Risk factors: Poorly controlled blood sugar, elevated blood pressure, having diabetes for a long duration, and kidney disease.
- Impact: Blurred or distorted vision, difficulty recognizing faces or reading, dull or faded colors, which can impair independence and safety.
Recognizing Symptoms and Getting Diagnosed
Early detection of DME significantly increases the chances of slowing or stopping its progression. Knowing the warning signs and seeking prompt evaluation is crucial.
- Common symptoms:
- Blurry or wavy vision at the center of your field of view
- Difficulty reading or recognizing faces
- Colors appear faded or washed out
- Sudden changes in vision
- When to see a doctor: If you experience these symptoms, arrange a comprehensive eye exam as soon as possible, especially if you have a known history of diabetes.
Eye specialists use several diagnostic tools to confirm DME, including:
- Dilated eye exam: Allows a detailed view of the retina using special drops.
- Optical coherence tomography (OCT): Produces cross-sectional images of the retina to confirm swelling.
- Fluorescein angiography: A special dye highlights blood vessel leaks during imaging.
Treatment Options for Diabetic Macular Edema
Prompt and tailored treatment for DME is vital to protect and possibly improve vision. Treatment plans can be multifaceted and are personalized according to the severity and response to therapy.
1. Managing Blood Sugar and Blood Pressure
Strict control of blood glucose and blood pressure remains the cornerstone for preventing DME and reducing further vision loss. Following your diabetes care team’s advice is essential.
- Adhere to prescribed diabetes medications and insulin regimens.
- Monitor blood sugar levels regularly and adjust your diet accordingly.
- Work with your healthcare provider to manage blood pressure, as hypertension worsens retinal swelling.
- Attend regular follow-up visits for monitoring and adjustments.
2. Anti-VEGF Injections
Anti-VEGF (vascular endothelial growth factor) medications have revolutionized DME treatment by targeting proteins that promote abnormal blood vessel growth and leakage.
- How it works: Inhibits VEGF, stabilizing and preventing new, weak blood vessels from leaking.
- Administration: Medication is injected directly into the eye by a retinal specialist after numbing the area.
- Common medications:
- Aflibercept (Eylea)
- Bevacizumab (Avastin)
- Ranibizumab (Lucentis)
- Faricimab (Vabysmo) – blocks both VEGF and Angiopoietin-2 (Ang-2) for potentially longer effects
- Frequency: Typically monthly injections for several months, then less frequent depending on response.
- Benefits & limitations: Can reverse swelling and improve vision for many people, but not everyone responds fully; not recommended in pregnancy.
3. Laser Therapy
Laser treatment (focal/grid laser photocoagulation) has been used for decades to seal leaking blood vessels in the retina:
- Purpose: Prevents further leakage by closing off abnormal retinal blood vessels.
- Procedure: Outpatient procedure using focused light energy; typically painless but may leave small blind spots in vision.
- Effectiveness: Helps protect remaining vision and can slow the progression of vision loss.
- Current role: Often used for specific forms of DME or when anti-VEGF therapy alone is insufficient.
4. Corticosteroid Treatment
Corticosteroids can reduce retinal inflammation and leakage:
- Types: Injections or implants that slowly release steroid medication over time.
- Indication: Typically offered when anti-VEGF treatments are ineffective or if there are contraindications.
- Considerations: May increase risk of cataracts and elevated eye pressure; regular monitoring is essential.
5. Other Emerging and Complementary Therapies
- Bispecific antibody drugs, such as those targeting both VEGF and Ang-2, offer additional options for some patients.
- New drugs and combination therapies continuously evolve as research provides more insights into DME mechanisms.
Living with Diabetic Macular Edema
While medical interventions are important, addressing daily challenges through assistive tools and emotional support is just as vital for preserving independence.
Low Vision Aids and Vision Rehabilitation
If DME has already affected your eyesight:
- Magnifying glasses, screens and stands enable easier reading or crafting.
- Telescopic lenses help with distance viewing, such as watching TV or identifying signs.
- High-intensity reading lamps improve contrast and visibility for reading and hobbies.
- Large-print materials such as books, newspapers, or labels simplify everyday tasks.
- Closed-circuit television (CCTV) magnifiers project reading material onto a screen for enhanced clarity.
- Digital tools: Smartphones, computers, and tablets with accessibility features can assist with reading, communication, and organization.
Vision rehabilitation specialists can provide skills and strategies for adapting to visual challenges. Personalized training may include:
- Orientation and mobility training for safe navigation
- Daily living skills for cooking, using appliances, managing medication, and self-care
- Assistive technology training
Practical Tips for Prevention and Lifestyle Support
- Maintain regular appointments with your eye doctor and diabetes care provider.
- Keep blood sugar and blood pressure in target ranges, using home monitors as recommended.
- Adopt a balanced diet rich in fruits, vegetables, whole grains, and lean protein.
- Engage in regular physical activity, tailored to your abilities and interests.
- Take medications exactly as prescribed; consult your doctor before making any changes.
- Monitor for new visual changes and report them promptly to your eye care team.
- Seek support from diabetes educators, support groups, or mental health professionals, especially if you are feeling isolated or frustrated.
Frequently Asked Questions (FAQs)
What is the main cause of diabetic macular edema?
DME is caused by damage to the retinal blood vessels due to long-term high blood sugar in diabetes, which leads to fluid leakage and swelling in the macula.
How is diabetic macular edema diagnosed?
Diagnosis involves a comprehensive eye exam, including dilated retinal examination, OCT imaging to assess retinal thickness, and sometimes fluorescein angiography to detect blood vessel leaks.
Can DME be cured?
There is currently no cure for diabetic macular edema, but treatments can stabilize or improve vision and help prevent further vision loss in many people.
Which treatments are most effective for DME?
Anti-VEGF injections are the current first-line therapy; other options like laser treatment and corticosteroids may be used individually or in combination depending on individual needs and responses.
What can I do to prevent diabetic macular edema or prevent it from worsening?
Keeping blood sugar, blood pressure, and cholesterol within target ranges, attending regular eye exams, and following all recommended treatments offer the best chance for preserving your vision.
Resources and Support
- Ask your eye doctor about local or online vision rehabilitation programs.
- Explore technology-based accessibility tools (large font settings, screen readers, contrast enhancement) for independence.
- Utilize reputable organizations such as Prevent Blindness, the American Diabetes Association, or your country’s diabetes/eye health resources for up-to-date information and support networks.
Summary Checklist: Managing Diabetic Macular Edema
| Area | What to Do |
|---|---|
| Blood Sugar Control | Frequent monitoring and adjustment, medication adherence |
| Regular Eye Exams | Yearly (or as recommended) comprehensive dilated eye exams, with OCT tests |
| Treatment Adherence | Receive anti-VEGF, laser, or steroid treatments as prescribed |
| Lifestyle Support | Healthy diet, exercise, control of other health risks |
| Vision Support | Low vision aids and rehabilitation if vision loss interferes with daily life |
| Mental Health | Seek counseling, support groups, or professional help if needed |
Final Thoughts
Diabetic macular edema is a serious but manageable condition when diagnosed early and treated promptly. Maintaining good communication with your healthcare team, remaining vigilant about monitoring your vision, and taking advantage of available rehabilitative resources can help you retain as much independence and quality of life as possible, even if your vision has changed.
References
- https://www.webmd.com/diabetes/diabetic-macular-edema-treatment
- https://www.elmanretina.com/services/treatments-and-services/diabetic-macular-edema/
- https://eyewiki.org/Diabetic_Macular_Edema
- https://preventblindness.org/diabetic-macular-edema-dme/
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/macular-edema
- https://my.clevelandclinic.org/health/diseases/24733-diabetes-related-macular-edema
- https://www.macularsociety.org/macular-disease/macular-conditions/diabetic-macular-oedema/
- https://www.mayoclinic.org/diseases-conditions/diabetic-retinopathy/multimedia/diabetic-macular-edema/img-20124558
- https://www.mdfoundation.com.au/about-macular-disease/diabetic-eye-disease/about-diabetic-macular-oedema/
Read full bio of medha deb












