Thyroid Eye Disease (TED): Causes, Symptoms, Risks, and Vision Loss FAQ
An in-depth guide to the causes, phases, symptoms, risk factors, and vision complications of thyroid eye disease (TED), including expert answers to frequently asked questions.
Thyroid Eye Disease (TED): Comprehensive Overview
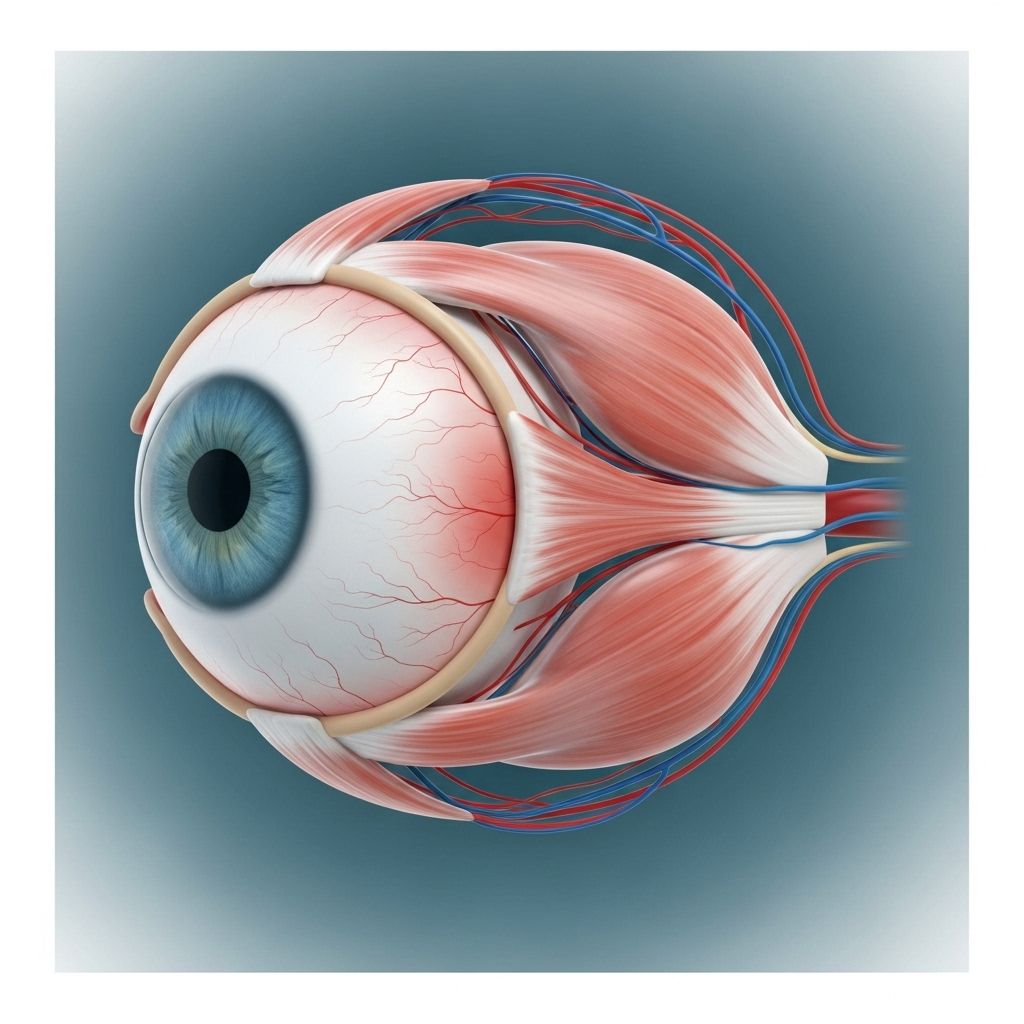
Thyroid eye disease (TED) is a complex autoimmune condition primarily impacting the tissues around the eyes. Known by several names—including Graves’ ophthalmopathy and Graves’ eye disease—TED is characterized by progressive inflammation, swelling, and abnormalities involving the muscles and fat behind the eye. While TED most commonly develops in people living with Graves’ disease and hyperthyroidism, it can also occur in those with normal or low thyroid hormone levels. Importantly, TED is a distinct disease and may persist even if the underlying thyroid condition is controlled.
Understanding TED is essential due to its potential to cause vision changes, appearance changes, and, in rare cases, vision loss. This article explores the causes, symptoms, phases, risk factors, and critical FAQs related to TED.
What is Thyroid Eye Disease (TED)?
TED is an autoimmune disorder. The immune system mistakenly attacks the tissues—including muscles and fat—behind the eye. This abnormal response leads to swelling, inflammation, and sometimes permanent changes within the eye socket.
Up to half of people diagnosed with Graves’ disease may develop TED. However, TED can also occur with other thyroid conditions—such as Hashimoto’s disease (hypothyroidism)—and sometimes develops in those with no abnormal thyroid hormone levels.
Treating thyroid dysfunction often does not resolve TED, making expert care essential for both conditions.
Main Features of TED
- Inflammation and swelling of tissues behind the eye.
- Bulging or protruding eyeballs (proptosis).
- Change in eyelid position (retraction).
- Impaired eye movement or double vision ( diplopia).
- Risk of optic nerve compression and vision loss in severe cases.
Symptoms of Thyroid Eye Disease
Symptoms are primarily caused by the swelling and dysfunction of eye socket tissues and can vary widely between individuals. TED may affect one or both eyes, with symptoms ranging from mild discomfort to severe vision impairment.
Early identification and expert management are crucial for preserving eye health and function.
- Dry, gritty, or irritated eyes
- Redness of the eyes
- Watery or teary eyes
- Puffy eyelids
- Bulging eyes (proptosis), giving a staring or startled appearance
- Eyelid retraction
- Sensitivity to light
- Double vision (diplopia)
- Blurry vision
- Eye pain or pressure
As TED progresses, more severe symptoms may develop:
- Trouble moving eyes and closing eyelids
- Incomplete eyelid closure (risk of corneal exposure)
- Corneal ulcers or scarring
- Loss or dullness of vision due to optic nerve compression or corneal damage
| Common Symptoms | Severe Symptoms |
|---|---|
| Dry, gritty eyes | Trouble closing eyes |
| Redness | Corneal ulcers/scarring |
| Puffy eyelids | Loss of vision (optic nerve compression) |
| Sensitivity to light | Double vision (diplopia) |
| Bulging eyes | Permanent visual changes |
Phases and Progression of TED
Thyroid eye disease progresses through two main phases:
- Active (Inflammatory) Phase: Lasts several months to two years, marked by inflammation, swelling, redness, and rapid symptom changes.
- Chronic (Stable) Phase: Inflammation subsides but scars and lasting changes may persist. Some symptoms may improve, but appearance or vision changes may become permanent.
TED is considered a progressive disease, with some patients experiencing worsening symptoms over time. Not all patients progress to severe phases, but early detection and intervention are vital for minimizing lasting damage.
Causes and Risk Factors
Autoimmunity is the primary underlying cause of TED. The body’s immune system generates antibodies that attack tissues behind the eye, leading to inflammation and swelling.
While the exact reasons for TED development remain unclear, several key risk factors are widely recognized:
- Presence of a thyroid condition such as Graves’ disease (hyperthyroidism) or Hashimoto’s disease (hypothyroidism)
- Previous radioactive iodine treatment for Graves’ disease
- Women are affected more frequently than men
- Middle-aged adults (age 40–60) have higher risk
- Smoking significantly increases risk and severity
Diagnosis of TED
Diagnosis begins with a combination of clinical symptoms and medical history, particularly the presence of a known thyroid disease.
Typical diagnostic steps include:
- Full eye examination to check for proptosis, double vision, eyelid retraction, and corneal damage
- Blood tests for thyroid hormones and autoantibody markers
- Imaging studies (CT, MRI) to assess tissue swelling, muscle enlargement, or optic nerve compression
Impact of TED on Vision
The primary concern with TED is its potential to cause vision impairment and, in rare cases, permanent vision loss. Not every individual with TED will lose vision, but several mechanisms can put vision at risk:
- Optic nerve compression: Swelling of tissues and fat pushes against the optic nerve, which carries visual signals from the eye to the brain. Compression can cause blurring, dullness of color, and, if untreated, permanent vision loss.
- Corneal exposure and ulcers: Difficulty closing eyelids may lead to dryness, unprotected cornea, and, eventually, open sores or ulcers on the eye’s surface. These ulcers can cause scarring and loss of vision if left untreated.
- Diplopia or double vision: Scarred or inflamed muscles can alter eye alignment, resulting in double vision and significant visual discomfort.
Prompt medical care is essential for any new vision changes in TED. Early treatment can help prevent lasting vision loss.
Reducing the Risks of TED and Blindness
While TED cannot always be prevented, several steps may reduce the risk or severity of symptoms and vision loss:
- Quit smoking: Smoking is a major modifiable risk factor for TED and worsens disease progression.
- Maintain good control of thyroid disease with regular endocrinologist visits.
- Report new visual symptoms promptly to an eye care provider, especially if experiencing pain, redness, double vision, or loss of color vision.
- Follow medical advice regarding medications (steroids, immunosuppressants, or biologics) and eye protection.
- Consider eye surgeries if recommended for advanced cases with vision risk.
Frequently Asked Questions about Thyroid Eye Disease and Blindness
Can thyroid eye disease cause blindness?
TED can rarely cause permanent blindness, but it happens only if complications—such as optic nerve compression or untreated corneal ulcers—are not managed early. Most people with TED do not become blind, especially with access to modern treatments and regular monitoring.
How quickly can TED cause vision problems?
Vision problems typically develop gradually. Severe cases may experience rapid deterioration if optic nerve compression or corneal damage occurs. Immediate reporting of visual changes (blurriness, pain, changes in color vision) is crucial for effective intervention.
Are TED and Graves’ disease always connected?
Up to half of people with Graves’ disease develop TED. However, TED can also occur with other thyroid diseases (like Hashimoto’s) or rarely in individuals with normal thyroid levels.
What are signs that TED is getting worse?
- Increasing redness, swelling, or pain around the eyes
- Worsening bulging or inability to close eyelids completely
- New or worsening double vision
- Changes in vision clarity or color perception
- Eye surface ulcers or visible scarring
Is the severity of TED related to the severity of thyroid disease?
No, the severity of TED does not always match the severity of thyroid disease or hormone imbalance. Managing thyroid hormone levels is important, but distinct treatments are required for TED symptoms.
Can TED improve after treatment?
Many patients see symptom improvement after the active phase resolves and with appropriate treatment. Some lasting changes—such as scarring, eye misalignment, or eyelid retraction—may persist. Surgery can help correct some appearance or vision changes.
How can I protect my vision if I have TED?
- Receive regular eye checkups, especially if experiencing new symptoms.
- Use lubricating eye drops to protect the cornea.
- Wear sunglasses for light sensitivity and shielding.
- Follow medical advice for TED management, including possible medications or surgical options.
- Quit smoking and maintain thyroid health as directed by your doctor.
Living with Thyroid Eye Disease
Living with TED requires an ongoing partnership between you, your endocrinologist, and your eye care provider. Regular monitoring and treatment adaptations are crucial as symptoms and risks can change over time.
TED impacts daily life, causing changes in appearance, comfort, and, for some, vision quality. Psychosocial support, practical adaptations (such as special eyewear or vision therapy), and ongoing education empower patients to cope with these challenges.
- Monitor your symptoms and promptly report changes.
- Consider psychological support or patient groups to address appearance concerns and emotional health.
- Stay informed about advances in TED treatments, as new therapies can offer better outcomes.
Summary Table: TED Snapshot
| Aspect | Description |
|---|---|
| Definitions | Autoimmune inflammation of eye socket tissues, often linked with Graves’ disease |
| Common Symptoms | Dry, gritty eyes; redness; bulging; double vision; eyelid retraction |
| Vision Threats | Optic nerve compression, corneal ulcers/scarring (rare) |
| Risk Factors | Thyroid disorders, smoking, middle age, female gender, radioactive iodine therapy |
| Prevention | Regular monitoring, quit smoking, expert thyroid management |
When to Seek Immediate Help
- Unexpected decrease in vision or color perception
- Severe or increasing eye pain
- Visible ulcers, open sores, or severe redness
- Complete inability to close the eyelids
Immediate care from an eye specialist is essential for any of these acute symptoms to prevent lasting damage.
Resources for Patients
- Regular consultation with endocrinologists and ophthalmologists
- Access to educational materials from patient advocacy groups
- Support from vision rehabilitation specialists if visual impairment occurs
Expert FAQs: Quick Reference
- Is TED curable? TED is manageable, and many symptoms can improve, especially with early intervention. Some changes may be permanent.
- What treatments are available? Medications (steroids, immunosuppressants, biologics), eye drops, and surgery (for vision-threatening cases).
- Will my appearance go back to normal? Some appearance changes can improve, but scarring or eye misalignment may persist. Surgery may help restore appearance.
- Should people with TED avoid certain activities? Activities causing eye dryness or strain should be minimized. Always wear eye protection outdoors and follow your care provider’s recommendations.
Thyroid eye disease is a complex and evolving condition requiring careful attention to both thyroid health and eye care. Early intervention, smoking cessation, and expert management are vital for reducing risks and maintaining quality of life.
References
- https://preventblindness.org/thyroid-eye-disease/
- https://www.thyroideyes.com/about-thyroid-eye-disease/phases-of-ted
- https://www.upmc.com/services/endocrinology/conditions/thyroid-eye-disease
- https://my.clevelandclinic.org/health/diseases/17558-thyroid-eye-disease
- https://www.aace.com/disease-and-conditions/thyroid/what-thyroid-eye-disease
- https://www.tedimpact.com/thyroid-eye-disease-signs-symptoms
- https://www.fightingblindness.org/diseases/thyroid-eye-disease-ted
- https://news.cuanschutz.edu/ophthalmology/warning-signs-and-treatment-for-thyroid-eye-disease
- https://eyewiki.org/Thyroid_Eye_Disease
Read full bio of medha deb












