Thoracic Outlet Syndrome: Causes, Symptoms, Diagnosis, and Treatment
A comprehensive guide to thoracic outlet syndrome—its origins, presentation, diagnosis, and management strategies for patients and caregivers.
Thoracic Outlet Syndrome: An In-depth Overview
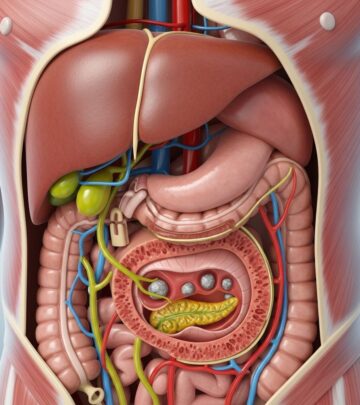
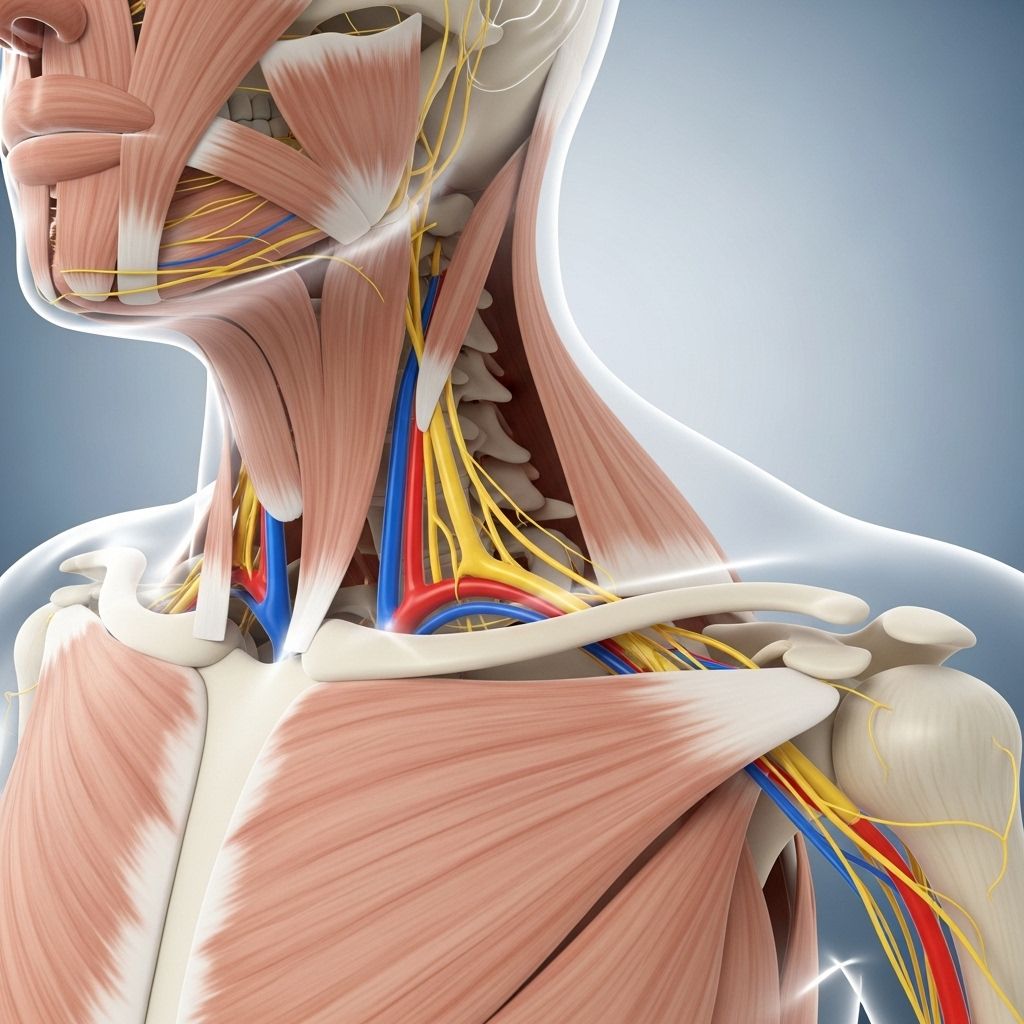
Thoracic outlet syndrome (TOS) is a complex condition characterized by the compression of nerves or blood vessels in the area between your collarbone and first rib, known as the thoracic outlet. This region serves as a critical passageway for the brachial plexus, major arteries, and veins that travel from your neck to your arm. Irritation or compression in this area can result in a variety of symptoms ranging from pain and tingling to weakness and vascular compromise.
This article explores the causes, risk factors, symptoms, diagnostic methods, and treatment options for TOS, and answers frequently asked questions about living with and managing the syndrome.
What Is Thoracic Outlet Syndrome?
Thoracic outlet syndrome encompasses several disorders caused by the compression of the neurovascular structures (nerves and blood vessels) traversing the thoracic outlet. These components include:
- The brachial plexus (major nerve bundle supplying the arm and hand)
- The subclavian artery (artery to the arm)
- The subclavian vein (major vein draining the arm)
Disruption can occur in any or all of these structures, causing a diverse range of symptoms and necessitating tailored diagnostic and therapeutic approaches.
Types of Thoracic Outlet Syndrome
| Type | Structures Involved | Prevalence | Common Symptoms |
|---|---|---|---|
| Neurogenic TOS | Nerves (brachial plexus) | Most common (>90%) | Pain, numbness, tingling, weakness |
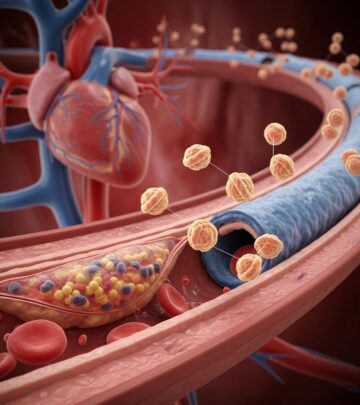
| Venous TOS | Veins (subclavian vein) | Less common | Swelling, cyanosis, blood clots |
| Arterial TOS | Arteries (subclavian artery) | Rarest | Coldness, color changes, claudication |
| Mixed/unspecified TOS | Multiple or unclear | Variable | Symptoms overlap |
Causes of Thoracic Outlet Syndrome
The underlying causes of thoracic outlet syndrome frequently relate to changes in the anatomy or function of the structures bordering the outlet:
- Congenital abnormalities such as a cervical rib (an extra rib above the first rib)
- Poor posture—hunched or slouched shoulders can decrease the outlet space
- Injury or trauma—fractures, dislocations, or soft tissue trauma to the neck, collarbone, or upper chest
- Repetitive arm movements—occupational or athletic activities (e.g., swimming, heavy lifting, construction) that strain the shoulder and neck c
- Muscular hypertrophy—such as in bodybuilders, enlarged muscles can crowd the passage
- Scar tissue formation after surgery or injury narrowing the outlet
Secondary causes may include muscle weakness (e.g., trapezius deficiency), large breasts, or cervical trauma.
Risk Factors
Certain risk factors make thoracic outlet syndrome more likely to develop, including:
- Gender (more common in females)
- Poor muscle development
- Chronic poor posture, prolonged desk work
- Previous injury to the chest or neck
- Participation in sports or jobs involving repetitive overhead arm movement
- Obesity
Signs and Symptoms of Thoracic Outlet Syndrome
Symptoms vary considerably depending on the structures compressed and their severity. Classic symptoms may include:
- Pain radiating from the neck to the shoulder, arm, and hand
- Numbness or “pins-and-needles” sensations in the fingers
- Weakness in the hand or arm
- Tingling and/or loss of sensation
- Swelling or discoloration of the arm or hand
- Coldness or pale color in fingers (suggestive of arterial involvement)
- Prominent veins or blood clots in the arm (venous involvement)
Symptoms may worsen with activity, lifting objects, or raising arms overhead, and can be persistent or intermittent.
How Is Thoracic Outlet Syndrome Diagnosed?
Because TOS symptoms may be shared with other conditions (such as rotator cuff injuries, cervical spine disorders, or carpal tunnel syndrome), diagnosis relies on a careful combination of physical examination, symptom evaluation, and diagnostic testing:
- Physical examination—palpation of the neck, shoulder, and arm; provocative maneuvers to reproduce symptoms
- Patient history—assessment of posture, occupation, sports activity, and prior injuries
- Imaging tests:
- X-rays to detect cervical ribs, fractures, or abnormal bone growth
- MRI or CT scan for assessment of soft tissues, muscles, and vascular structures
- Ultrasound (especially for vascular TOS)
- Vascular studies—arteriography, venography to look for vessel compromise
- Electrodiagnostic studies—EMG or nerve conduction studies if nerve involvement suspected
Diagnosis may be challenging, as many patients have normal imaging or test results, and diagnosis often relies primarily on symptom patterns and exclusion of other conditions.
Treatment for Thoracic Outlet Syndrome
The primary approach to treatment is conservative (nonsurgical), except in severe cases or when symptoms threaten limb function. The general treatment options include:
1. Conservative Management
- Physical therapy: Specialized exercises to strengthen and stretch the muscles around the shoulder and neck, improve posture, and increase flexibility. PT is regarded as the first-line therapy for neurogenic TOS and can improve pain and nerve symptoms over time.
- Lifestyle changes: Correction of posture, avoidance of overhead sleeping positions, ergonomic adjustments for work activities, and avoidance of repetitive arm movements.
- Medications: Pain relievers, anti-inflammatory drugs, and muscle relaxants may be prescribed to decrease pain and inflammation. In cases of blood clots, blood thinning medications (anticoagulants) or clot dissolving agents (thrombolytics) may be required.
- Injections: Local anesthetics, steroids, or botulinum toxin (Botox) injections may be considered to treat persistent neurogenic pain.
2. Surgical Intervention
- Surgery is reserved for those with severe or persistent symptoms not relieved by conservative measures, or for patients with vascular complications (blood clots, limb-threatening ischemia).
- Procedures may include removal of a cervical rib, scalene muscle resection, or decompression of soft tissue or bone.
- Surgical intervention can involve significant risks and long-term consequences; success rates and disability vary depending on the specific procedure and patient factors.
Postoperative rehabilitation, similar to regular physical therapy, is essential for recovery after surgery and may improve strength and function.
Living with Thoracic Outlet Syndrome
Managing TOS is often a multidisciplinary process, involving collaboration among physical therapists, neurologists, orthopedic surgeons, vascular surgeons, and pain specialists. Long-term outcomes depend on prompt diagnosis, the extent of compression, the underlying cause, and adherence to therapy. Some individuals may experience recurrence of symptoms despite treatment.
Self-care Strategies
- Maintain good posture
- Use ergonomic adjustments at work
- Perform regular physical therapy or recommended exercises
- Avoid carrying heavy loads on the affected shoulder
- Monitor symptoms and seek medical advice if they worsen
Frequently Asked Questions (FAQs)
Q: What causes thoracic outlet syndrome?
A: TOS results from compression of nerves or blood vessels in the thoracic outlet region, most often due to anatomical variations (such as a cervical rib), poor posture, injury, repetitive arm activities, or muscular hypertrophy.
Q: What are the most common symptoms?
A: Common symptoms include pain, numbness, tingling, and weakness in the neck, shoulder, arm, or hand. Vascular TOS may cause swelling, discoloration, or blood clots.
Q: How is TOS diagnosed?
A: Diagnosis is based on physical examination, symptom history, and supportive imaging or nerve studies. Tests such as X-rays, MRI, CT scans, and electrodiagnostics may help rule out other causes.
Q: What treatments are available?
A: Most cases are treated with physical therapy, posture correction, and pain medications. Surgery is sometimes necessary in severe cases, particularly with major blood vessel involvement or structural compression that is not resolved otherwise.
Q: Can thoracic outlet syndrome recur?
A: Symptoms may return in some patients even after physical therapy or surgery, especially if underlying risk factors remain unchanged.
Q: Who treats TOS?
A: Care may include physiatrists, physical therapists, orthopedic surgeons, vascular or thoracic surgeons, and pain medicine doctors.
Prevention and Prognosis
- Prompt recognition and treatment of symptoms can prevent progression.
- Core prevention strategies focus on maintaining good posture, avoiding repetitive strain and trauma, and addressing underlying anatomical issues.
- The majority of patients benefit from conservative therapy, especially physical therapy and lifestyle modification.
- Surgical intervention is reserved for severe or refractory cases and carries varying long-term outcomes.
Key Takeaways
- Thoracic outlet syndrome is a constellation of symptoms secondary to nerve or vessel compression at the neck-shoulder junction.
- Diagnosis depends on symptom assessment, medical history, and exclusion of other causes.
- Most cases are amenable to physical therapy, postural correction, and other conservative treatments.
- Surgery may be required for severe vascular or neurological compromise, but outcomes are variable.
- Long-term management involves coordinated care and lifestyle adjustments.
References
- https://www.hss.edu/health-library/conditions-and-treatments/list/thoracic-outlet-syndrome-tos
- https://www.ncbi.nlm.nih.gov/books/NBK557450/
- https://www.nhs.uk/conditions/thoracic-outlet-syndrome/
- https://www.mayoclinic.org/diseases-conditions/thoracic-outlet-syndrome/diagnosis-treatment/drc-20353994
- https://www.yalemedicine.org/conditions/thoracic-outlet-syndrome
- https://my.clevelandclinic.org/health/diseases/17553-thoracic-outlet-syndrome-tos
- https://www.mayoclinic.org/diseases-conditions/thoracic-outlet-syndrome/symptoms-causes/syc-20353988
- https://www.youtube.com/watch?v=36aqa6FsBAY
Read full bio of Sneha Tete