Third-Degree Heart Block Treatment: Pacemakers, Medications, and Prognosis
Explore treatment options for third-degree heart block, including pacemakers, medications, and prognosis for patients with this serious cardiac condition.
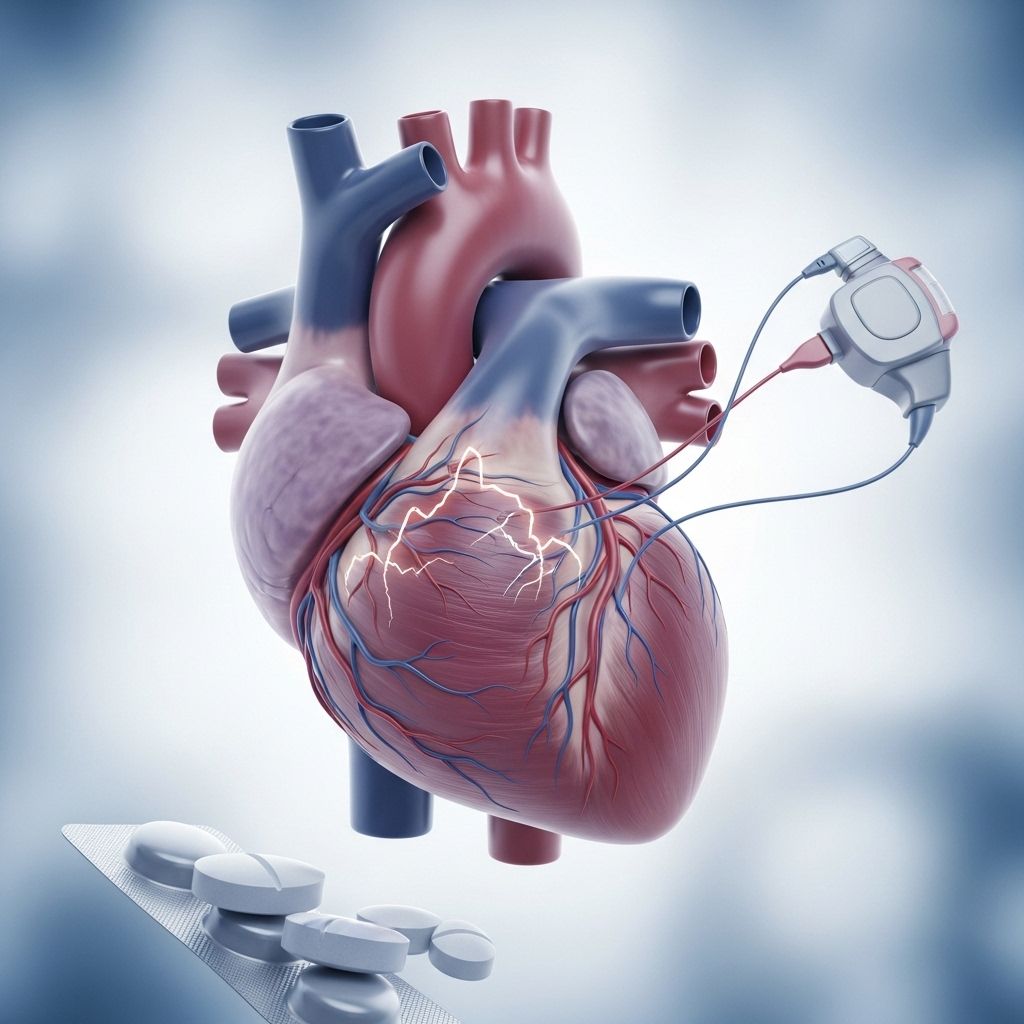
Third-degree heart block, also known as complete heart block, is a potentially life-threatening condition that severely impairs the electrical activity responsible for your heart’s rhythm and function. When left untreated, it may lead to cardiac arrest, syncope, or sudden death. This article explores the main treatment strategies, including pacemaker implantation, medication therapy, and addresses the prognosis for people affected by this serious cardiac disorder.
Understanding Third-Degree Heart Block
Third-degree heart block occurs when electrical signals from your heart’s upper chambers (atria) are completely blocked from reaching the lower chambers (ventricles). This results in a slow or irregular heartbeat, limiting the heart’s ability to pump blood efficiently. Immediate medical attention is vital to restore healthy cardiac function and prevent further life-threatening complications.
Symptoms of Third-Degree Heart Block
- Sudden fainting (syncope)
- Severe bradycardia (abnormally slow heart rate)
- Fatigue, weakness, or dizziness
- Shortness of breath
- Chest pain or discomfort
- Potential for cardiac arrest
Third-degree heart block is the most severe form among the three heart block categories and requires emergency intervention to prevent potentially fatal events.
Treatment Goals for Third-Degree Heart Block
The primary objective of treating third-degree heart block is to restore a healthy heart rate and rhythm, ensuring adequate blood circulation throughout the body. In many cases, it is also crucial to identify and manage any underlying causes—such as infections or drug toxicity—to prevent recurrence.
Main Treatment Options for Third-Degree Heart Block
Therapy typically combines immediate interventions to stabilize the heart rate with longer-term management strategies. The most common treatments include:
- Pacemaker implantation
- Medication therapy (e.g., atropine, antibiotics, catecholamines)
- Transcutaneous pacing (temporary, external pacing)
Pacemaker Implantation
For the vast majority of patients, especially those with persistent third-degree heart block, the implantation of a pacemaker is the gold-standard treatment. Pacemakers are small, battery-powered devices surgically placed near the collarbone. Their flexible leads (wires) extend into heart tissue, where they send regular electrical pulses that maintain a safe heart rate and rhythm.
| Type of Pacemaker | Use Case |
|---|---|
| Temporary Pacemaker | Short-term stabilization before permanent implantation or correction of a reversible cause. |
| Permanent Pacemaker | Long-term solution for irreversible, persistent third-degree heart block or congenital cases. |
Pediatric and Adult Guidelines: Medical societies, including the Heart Rhythm Society and the American Heart Association, recommend permanent pacemakers if the heart block has no reversible cause or if it is congenital and symptomatic. Children with non-reversible heart block benefit from lifelong pacemaker support to maintain healthy cardiac function.
Atropine Medication
Atropine is an anticholinergic drug sometimes administered intravenously to raise heart rate. It works by influencing the atrioventricular (AV) node to improve conduction from atria to ventricles. However, in third-degree heart block’s complete disruption of electrical signals, atropine is often less effective than in milder block types. Nevertheless, it may temporarily revive electrical activity and is usually considered a first-line emergency drug in advanced cardiac life support protocols.
Atropine is given as an initial 1 mg dose IV and can be repeated every 3–5 minutes up to a maximum of 3 mg. If atropine fails, other medications or mechanical pacing may be warranted.
Antibiotics in Heart Block Management
In rare cases, bacterial infections, such as Lyme disease, may trigger third-degree heart block. If Lyme carditis is suspected, intravenous antibiotics like ceftriaxone are used, followed by oral agents such as doxycycline. Restoring normal heart rhythm through antibiotics has, in some documented cases, eliminated the need for pacemaker implantation. However, most third-degree heart block cases are not infection-related.
Transcutaneous Pacing
Transcutaneous pacing (TCP) delivers electrical impulses externally using specialized pads attached to the chest and back. TCP is a noninvasive, temporary emergency measure. It’s commonly used:
- While awaiting permanent pacemaker implantation
- In cases of heart attack-induced heart block as an interim therapy
- When medications are ineffective
This intervention can be uncomfortable or painful, so conscious patients should be sedated. TCP is particularly valuable when immediate rhythm stabilization is necessary.
If TCP fails, transvenous pacing—an internal, temporary pacemaker—is considered. Both are bridge therapies until permanent solutions are implemented.
Catecholamine Hormones and Other Medications
Dopamine and epinephrine infusions are used as second-line options, especially for symptomatic bradycardia associated with heart block. They help increase heart rate and cardiac output temporarily but are rarely successful as standalone treatments in third-degree heart block. These drugs mainly serve to stabilize patients until mechanical pacing interventions can be established.
Is Epinephrine an Option?
Epinephrine, a potent catecholamine hormone, can temporarily support heart function and blood circulation by stimulating cardiac output and raising blood pressure. However, like dopamine and atropine, it seldom reverses established third-degree heart block and is utilized as an interim supportive therapy.
Treating Underlying Causes
Because third-degree heart block is often a complication triggered by other conditions (such as myocardial infarction, drugs, or infections), it’s essential to manage the underlying disease alongside cardiac interventions. This may involve:
- Treating infections with antibiotics
- Discontinuing or reversing medication toxicity
- Addressing structural cardiac abnormalities
If underlying problems persist, even pacing or medication therapies may not succeed until the root cause is resolved.
Prognosis and Living With Third-Degree Heart Block
Most people recover normal or near-normal heart function after a permanent pacemaker is implanted. These devices generally last 8–10 years and may require replacement. With careful cardiology follow-up and management of other heart risks, patients can usually lead functional, active lives.
- Pacemaker patients must periodically check for battery depletion and device malfunction.
- Adopting heart-healthy lifestyle habits—such as a balanced diet, regular exercise, and medication compliance—improves long-term outcomes.
- Cardiologist monitoring is crucial to evaluate device function and address any new symptoms.
Congenital heart block cases (present at birth) require specialized care and early pacing interventions, with regular pediatric cardiology follow-up.
Frequently Asked Questions (FAQs)
Q: Is third-degree heart block a medical emergency?
A: Yes, third-degree heart block is an emergency requiring immediate intervention to prevent sudden cardiac arrest and death.
Q: Can medications alone cure third-degree heart block?
A: In most cases, medications are only temporarily effective, and a pacemaker is needed. Rarely, heart block from infections such as Lyme carditis may resolve fully with antibiotic therapy.
Q: What is the life expectancy with a pacemaker?
A: Pacemaker patients can have a normal life expectancy if the device works properly and underlying cardiac conditions are managed.
Q: Will a pacemaker prevent future heart block?
A: Pacemakers do not treat the underlying cause but maintain proper heart rhythm. Ongoing evaluation for other cardiac risks is essential.
Q: Are there risks associated with pacemaker implantation?
A: Although serious risks are uncommon, possible complications include infection, bleeding, device malfunction, and, rarely, displacement of leads.
Q: How often do pacemakers need to be replaced?
A: Most pacemakers last 8–10 years. Periodic checks help determine when replacement is necessary.
Key Takeaways
- Third-degree heart block is a critical arrhythmia requiring emergency intervention.
- Pacemaker implantation is the standard, long-term treatment for most cases.
- Medications (atropine, epinephrine, dopamine) provide short-term support but are rarely definitive alone.
- Transcutaneous pacing bridges the gap until a permanent solution is implemented.
- Addressing underlying causes (e.g., infection, drug toxicity) is crucial for full recovery in selected cases.
- Regular follow-up with a cardiologist supports optimal health and early detection of device issues.
References
- Medically reviewed by Uzochukwu Ibe, MD, MPH — Written by James Roland, Healthline, Jan 6, 2023.
- Heart Rhythm Society Guidelines
- American Heart Association 2018 Guidelines
- Advanced Cardiac Life Support (ACLS) Bradycardia Algorithm
References
- https://www.healthline.com/health/heart-disease/third-degree-heart-block-treatment
- https://www.aclsonline.us/rhythms/complete-heart-block/
- https://www.ncbi.nlm.nih.gov/books/NBK545199/
- https://www.medicalnewstoday.com/articles/third-degree-heart
- https://my.clevelandclinic.org/health/diseases/17056-heart-block
- https://www.heartandstroke.ca/heart-disease/conditions/heart-block
- https://www.medicalnewstoday.com/articles/180986
- https://www.yalemedicine.org/conditions/atrioventricular-block
Read full bio of Sneha Tete












