Third-Degree Heart Block: Causes, Symptoms, and Treatments
Understand the causes, symptoms, urgent care needs, and long-term management of third-degree heart block, the most severe heart block type.
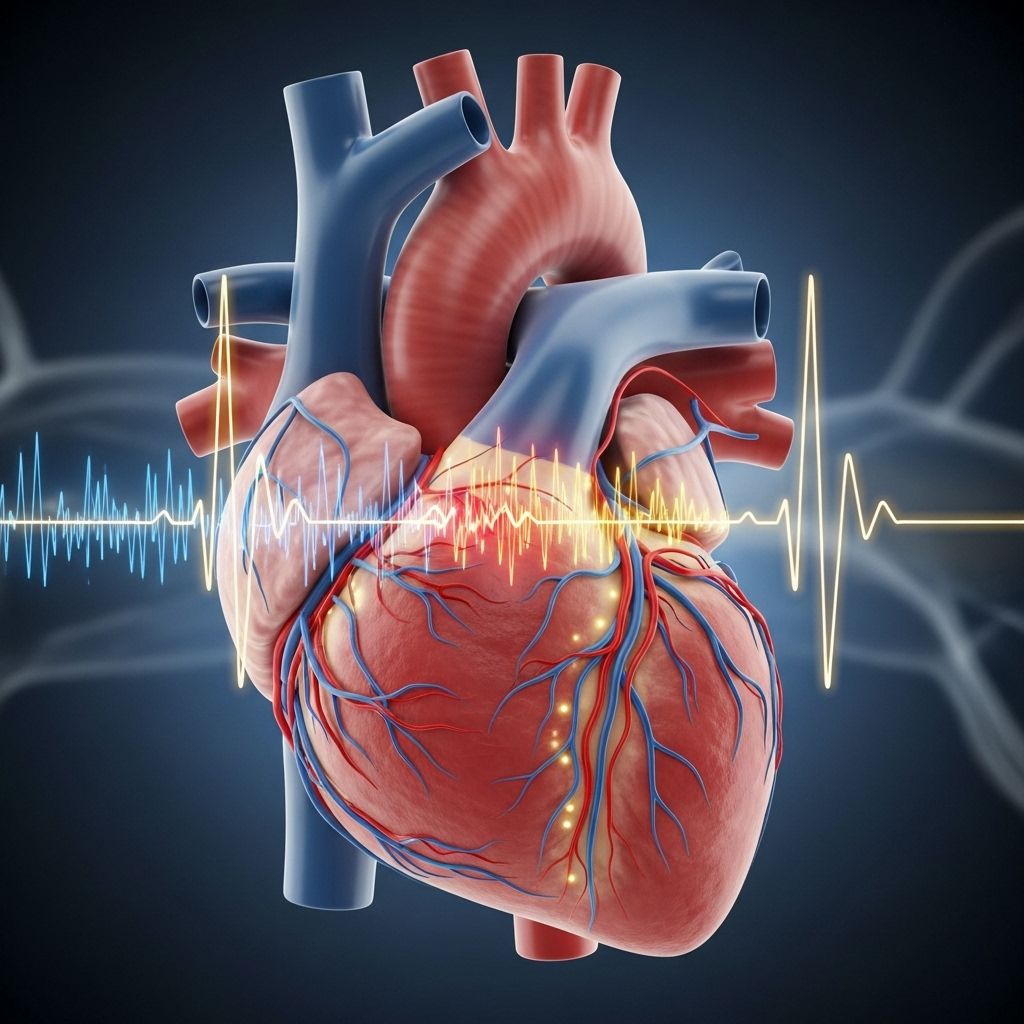
Third-degree heart block, also known as complete heart block, is the most severe type of heart block. It occurs when the electrical signals from the heart’s upper chambers (atria) cannot travel properly to the lower chambers (ventricles), causing the atria and ventricles to beat independently from one another. This interruption in electrical signaling leads to a dangerously low and often irregular heartbeat, significantly impairing the heart’s ability to pump blood throughout the body.
This condition is considered a medical emergency and requires immediate attention and prompt treatment, as it can result in sudden cardiac arrest and death if not managed quickly.
Table of Contents
- Overview of Third-Degree Heart Block
- What Causes Third-Degree Heart Block?
- Symptoms of Third-Degree Heart Block
- Diagnosis
- Treatment Options
- Prognosis and Outlook
- Prevention and Risk Reduction
- Frequently Asked Questions
- When to Seek Emergency Help
Overview of Third-Degree Heart Block
Heart block refers to the disruption of the heart’s electrical system. The electrical system controls the timing and sequence of your heartbeats. In third-degree heart block, the interruption is so severe that no electrical impulses pass between the atria and the ventricles. Consequently, both chambers beat independently, with the ventricles relying on slow, alternate signals, resulting in a slow, inefficient heartbeat.
- Third-degree heart block = complete disconnection between upper and lower heart chambers
- Most serious type of heart block, distinct from first- and second-degree blocks
- Requires prompt emergency intervention
What Causes Third-Degree Heart Block?
Third-degree heart block has a variety of possible causes. It is often linked to underlying heart disease, but can also result from other medical conditions, surgical procedures, or even medication side effects.
- Heart attack (myocardial infarction): Damage to the heart tissue disrupts electrical pathways.
- Cardiomyopathy: A disease that weakens the heart muscle, interfering with signal transmission.
- Myocardial fibrosis: Scarring of the heart tissue hampers the passage of electrical impulses.
- Open heart surgery: Procedures can sometimes damage the heart’s electrical system.
- Valve disease: Problems with the heart valves may impact conduction pathways.
- Lyme disease: Certain infections, such as Lyme disease, can cause temporary or permanent blockages in the conduction system.
- Medications: Some heart and blood pressure medications can affect the electrical system and cause blocks.
- Other infections or systemic diseases: Inflammation from illnesses can interfere with signaling.
Additional factors increasing the risk include:
- High blood pressure
- High blood sugar (diabetes)
- Family history of heart block: Some rare hereditary forms exist, but most cases are not inherited.
- Congenital heart block: Present at birth, often linked to autoimmune conditions in the mother, such as lupus or Sjogren’s syndrome.
Symptoms of Third-Degree Heart Block
Individuals with third-degree heart block often experience a slow or faint pulse. Because the normal electrical connection is disrupted, both parts of the heart operate separately, leading to an insufficient blood supply to the body.
The most common symptoms include:
- Dizziness or lightheadedness
- Fatigue
- Fainting (syncope)
- Chest pain or discomfort
- Shortness of breath
- Confusion, drowsiness, or difficulty concentrating
- Feeling unusually tired
Symptoms can develop suddenly and may be severe. The severity of symptoms can escalate quickly and, without rapid treatment, can lead to sudden cardiac arrest.
Diagnosis
Diagnosing third-degree heart block is a medical emergency and is typically performed in an emergency department or acute care setting. Immediate diagnosis is critical for initiating life-saving interventions.
- Physical examination: Health care providers may find a very slow, irregular, or faint pulse.
- Electrocardiogram (ECG or EKG): The gold standard diagnostic tool. It records the heart’s electrical signals and can clearly show the dissociation between atrial and ventricular activity.
- Blood tests: To rule out underlying causes such as a heart attack, electrolyte imbalances, or infections.
- Imaging: Tests like echocardiography (ultrasound of the heart) may be used to assess heart structure and function.
Treatment Options
Third-degree heart block requires immediate treatment. The goal is to restore normal heart rhythm and ensure that blood is adequately pumped to the body’s organs.
Acute Emergency Care
- Call emergency services (911) at the first sign of suggestive symptoms.
- Temporary pacing: Insertion of temporary pacemaker leads or pads to artificially stimulate the heart until a long-term solution is arranged.
- Use of medications such as atropine, epinephrine, or dopamine to temporarily raise the heart rate. These may provide short-term improvement but are not definitive treatments.
Long-Term Treatments
- Permanent pacemaker placement: The mainstay of treatment for most people with third-degree heart block. A pacemaker is a small device inserted under the skin that sends electrical impulses to maintain a normal heart rhythm.
- Medication review: Stopping or adjusting any medications that may be responsible for the block.
- Treatment of underlying conditions: Addressing infections, adjusting other medical conditions, or correcting electrolyte imbalances.
Pacemaker therapy is individually tailored. Most devices today can sense and respond to the heart’s own activity, delivering electrical impulses only when required. Some people may need more complex devices or additional therapies if they have other heart rhythm problems in addition to third-degree block.
Potential Complications of Treatment
Pacemakers are generally very safe but can be associated with certain complications:
- Pacemaker syndrome: Symptoms of fatigue or discomfort due to the way the pacemaker coordinates the heartbeats.
- Infection or bleeding: Rare but possible following pacemaker insertion.
- Lead displacement: Movement of the wires that connect the pacemaker to the heart may require repositioning.
Prognosis and Outlook
The prognosis of third-degree heart block depends on the rapidity of diagnosis and treatment, the presence of underlying heart disease, and general health status.
- Without treatment: The outlook is poor, with a high risk of sudden cardiac arrest and death.
- With prompt treatment: Most people can return to normal activities. Modern pacemakers allow for a good quality of life and long-term outcomes are generally favorable.
- Ongoing management: Regular follow-up with a cardiologist is required to monitor pacemaker function and overall heart health.
Prevention and Risk Reduction
While not all cases of third-degree heart block can be prevented, addressing modifiable risk factors can help reduce overall risk.
- Manage high blood pressure: Control blood pressure through lifestyle changes and medication if needed.
- Control blood sugar levels: Especially important for people with diabetes or prediabetes.
- Treat underlying heart conditions: Regular cardiac care and medication adherence.
- Monitor medication use: Take all medications as prescribed and report side effects to your doctor promptly.
Frequently Asked Questions (FAQs)
What is the difference between third-degree and lesser heart blocks?
First- and second-degree blocks indicate partial interruption of electrical flow, usually with some retained connection between the atria and ventricles. Third-degree block is a complete interruption: the chambers beat independently and the risk is much greater.
Can third-degree heart block ever go away by itself?
Rarely, if caused by a reversible condition such as medication side effects or Lyme disease, the block might resolve with treatment of the underlying problem. However, in most cases, a pacemaker is necessary for long-term management.
Is a pacemaker always needed?
Most cases require permanent pacemaker implantation, especially if the block is due to permanent damage or if symptoms are severe.
Can children have third-degree heart block?
Yes. Third-degree heart block can be congenital (present at birth), especially if the mother has an autoimmune condition such as lupus or Sjogren’s syndrome. It may also occur in older adults due to progressive disease.
How is life different after a pacemaker?
Today’s pacemakers are reliable and unobtrusive. Most people can resume normal physical activities, work, and travel. Regular check-ups are necessary to ensure the device functions optimally.
When to Seek Emergency Help
Third-degree heart block is a true medical emergency. Immediate medical attention is required if you or someone you are with experiences:
- Sudden chest pain
- Fainting or nearly fainting
- Severe shortness of breath
- Confusion, weakness, or sudden drowsiness
- Symptoms that rapidly worsen
If any of these symptoms are present, call emergency services (911 in the United States) immediately or get to the nearest emergency department.
Other Times to Contact Your Doctor
- Minor episodes of lightheadedness or unexplained fatigue
- Ongoing symptoms despite treatment
- New symptoms related to your heart rhythm
Summary
Third-degree (complete) heart block is a life-threatening heart rhythm disorder where electrical signals fail to travel between the heart’s chambers. Quick recognition, emergency intervention, and, most often, pacemaker implantation are vital for recovery. Understanding symptoms, risk factors, and the urgency of this condition can help save lives and support long-term heart health.
References
- https://www.ummhealth.org/health-library/understanding-third-degree-heart-block
- https://en.wikipedia.org/wiki/Third-degree_atrioventricular_block
- https://www.healthline.com/health/heart-disease/3rd-degree-heart-block
- https://my.clevelandclinic.org/health/diseases/17056-heart-block
- https://www.ncbi.nlm.nih.gov/books/NBK545199/
- https://litfl.com/av-block-3rd-degree-complete-heart-block/
Read full bio of Sneha Tete












