Third-Degree Heart Block: Causes, Symptoms, Diagnosis, and Treatment
Understand the most serious form of heart block — how it occurs, is diagnosed, and treated, plus key symptoms and risk factors.
What is Third-Degree Heart Block?
Third-degree heart block, also called complete heart block or third-degree atrioventricular (AV) block, is the most severe form of heart block. It represents a dangerous failure in the heart’s electrical conduction system, where signals between the upper chambers (atria) and lower chambers (ventricles) are completely disrupted.
This means the atria and ventricles beat independently, leading to a very slow heart rate and severely reduced ability to pump blood throughout the body. Left untreated, third-degree heart block can be fatal and is considered a medical emergency.
Prompt intervention, including emergency medical care and pacemaker insertion, is crucial for survival and quality of life.
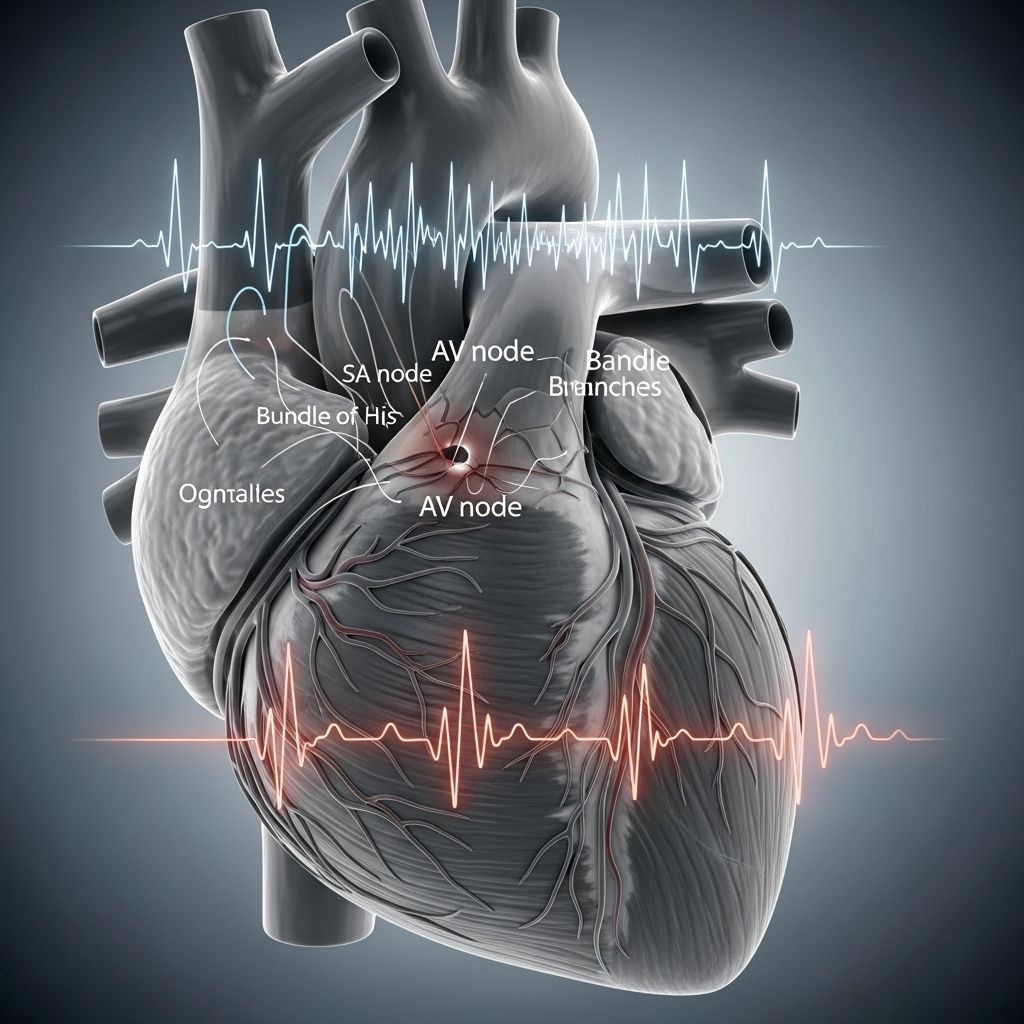
How Does the Heart’s Electrical System Work?
The heart beats in response to electrical signals that originate in the sinoatrial (SA) node, travel through the atria, and then pass through the atrioventricular (AV) node to the ventricles. This coordination ensures the chambers beat in a synchronized manner, pumping blood efficiently.
In third-degree heart block, this transmission fails entirely at the AV node: impulses from the atria never reach the ventricles. The ventricles rely on a much slower “escape rhythm” — an emergency backup that cannot match normal heart rates — causing pronounced bradycardia (slow heartbeat).
Causes of Third-Degree Heart Block
There are various underlying causes for this severe conduction defect. Many cases are linked to heart diseases, but other triggers exist:
- Heart attack (myocardial infarction): Tissue death or damage in the heart can disrupt its electrical system.
- Cardiomyopathy: Diseases thicken, enlarge, or cause scarring in the heart muscle, impeding signal conduction.
- Myocardial fibrosis: Scarring blocks electrical pathways through the heart.
- Open heart surgery and procedural complications: Damage from surgical interventions can injure conduction pathways.
- Valve disease: Abnormalities in heart valves sometimes extend to the conduction network.
- Infections (e.g., Lyme disease): Certain infections inflame or infect heart tissues, interfering with electrical signaling.
- Medication side effects: Drugs such as beta-blockers, calcium channel blockers, or digoxin sometimes block electrical transmission.
- Other infections and inflammatory conditions: e.g., rheumatic fever, sarcoidosis.
- Electrolyte imbalance: Abnormal levels of potassium or magnesium can precipitate heart block in predisposed people.
- Congenital (present at birth): Some infants are born with third-degree heart block, particularly if their mothers had autoimmune conditions (e.g., lupus or Sjogren’s syndrome).
- Family history: Genetics play a role, although inherited heart block is rare.
- Older age: Degeneration of the conduction system tends to occur with aging.
Emerging research also links high blood pressure and high fasting blood glucose as modifiable risk factors associated with raised heart block risk.
Symptoms of Third-Degree Heart Block
Symptoms of complete heart block are often dramatic due to extremely slow and ineffective heartbeats:
- Very slow or faint pulse
- Dizziness or lightheadedness
- Extreme fatigue or tiredness
- Fainting (syncope)
- Chest pain
- Shortness of breath
Some individuals may experience confusion, weakness, or even a sudden loss of consciousness and are at risk for sudden cardiac arrest.
When Is It a Medical Emergency?
Third-degree heart block is always a medical emergency. If you or someone else displays these symptoms — especially if accompanied by fainting, chest pain, or shortness of breath — call 911 (or your emergency services number) immediately or seek urgent medical help.
Diagnosis: How Is Third-Degree Heart Block Identified?
Diagnosing third-degree heart block involves a combination of clinical assessment and investigations:
- Physical examination: Listening to heart rate, rhythm, and pulse; observing for slow pulse and signs of low cardiac output.
- Electrocardiogram (ECG/EKG): The key diagnostic test for heart block. It will reveal atria and ventricles beating independently, with a slow ventricular rhythm.
- Blood tests: Used to check for electrolyte imbalance, underlying infections, or medication levels.
- Imaging (echocardiogram, chest X-ray): May help identify structural heart disease or monitor for complications.
An ECG pattern characteristic of third-degree block is a complete dissociation between P waves and QRS complexes.
Sometimes, additional tests are needed to identify reversible causes, such as metabolic disorders or drug toxicity.
Treatment Options for Third-Degree Heart Block
Third-degree heart block must be treated urgently. The primary goal is restoring reliable heart rhythm and output. Treatment options include:
- Medications for immediate stabilization:
- Atropine: Can increase heart rate temporarily in some forms.
- Epinephrine or dopamine: Used in severe cases to stimulate heart rate.
- Special agents (glucagon, calcium chloride, digoxin immune Fab) may be needed if drug overdose is the cause.
- Permanent pacemaker insertion: The definitive therapy for third-degree block not caused by reversible drug effects. The artificial pacemaker delivers regular electrical impulses to keep the heart beating at a life-sustaining rate.
- Temporary (transcutaneous) pacing: In emergencies, external pacing devices can maintain heart rate until a permanent pacemaker is implanted.
- Stopping or changing medications: If a drug is responsible, discontinuing it can reverse the block in some cases.
In rare circumstances where a reversible cause is identified (such as an infection or electrolyte abnormality), treating the underlying issue may restore normal electrical conduction.
Pacemaker Devices
Most people with third-degree heart block require a dual-chamber pacemaker. This device senses electrical activity in both atria and ventricles and can coordinate their beats. Some may require a biventricular (three-lead) pacemaker for more advanced coordination. Pacemaker correction may sometimes lead to pacemaker syndrome, requiring adjustments or alternative pacing strategies.
Possible Complications of Third-Degree Heart Block
Left untreated or even sometimes despite therapy, third-degree heart block can lead to serious complications:
- Sudden loss of consciousness (syncope)
- Sudden cardiac arrest
- Reduced blood flow to organs, resulting in organ dysfunction
- Pacemaker syndrome in some cases
Some complications are directly related to the underlying cause, pacemaker device, or any persistence of abnormal heart rhythms.
Prognosis and Outlook
The outlook for third-degree heart block depends heavily on immediate recognition and intervention. With prompt treatment and pacemaker insertion:
- Symptoms such as dizziness, fainting, and fatigue typically resolve.
- People can return to near-normal activity, with a notable improvement in quality of life.
- The risk of sudden cardiac death is dramatically reduced.
Individuals living with pacemakers require regular follow-up for device monitoring and management of any additional heart conditions. If third-degree heart block arises from reversible causes and is cured, prognosis may be better than cases requiring lifelong pacing.
Long-Term Management and Prevention
- Managing underlying risk factors: Control blood pressure, blood sugar, and other heart disease risks to lower chances of heart block.
- Medication monitoring: Regular review by a healthcare professional can reduce medication-induced heart block.
- Lifestyle modifications: Heart healthy diet, regular exercise, and avoiding smoking or substance abuse.
- Regular cardiology check-ups if there is a family history or prior heart events.
- Those with autoimmune conditions should inform their doctors and monitor symptoms during pregnancy.
Frequently Asked Questions (FAQs) about Third-Degree Heart Block
Q: What is the difference between first, second, and third-degree heart block?
A: Heart block refers to impaired conduction between the atria and ventricles.
- First-degree: Signals are delayed but still reach the ventricles.
- Second-degree: Some signals fail to reach the ventricles, resulting in dropped beats.
- Third-degree: No signals pass from the atria to the ventricles; atria and ventricles beat independently.
Q: Is third-degree heart block reversible?
A: Sometimes — if caused by drugs, electrolyte imbalance, or specific infections like Lyme disease — it may resolve with successful treatment. Otherwise, most cases require a permanent pacemaker for correction.
Q: What should I do if I suspect third-degree heart block?
A: Seek emergency medical attention immediately. Symptoms such as fainting, chest pain, and irregular or very slow pulse warrant activation of emergency services (911 or local emergency number).
Q: Can children have third-degree heart block?
A: Yes. It may be congenital, especially if their mothers had autoimmune diseases during pregnancy. Early detection and monitoring are essential for children at risk.
Q: What does the ECG look like in third-degree heart block?
A: The classic finding is a complete dissociation of P waves and QRS complexes — atria and ventricles both generate impulses independent of each other.
Q: Can third-degree heart block lead to cardiac arrest?
A: Yes. The severely slow heartbeat and lack of coordinated pumping can lead to sudden loss of consciousness and even cardiac arrest if not treated promptly.
Summary Table: Third-Degree Heart Block Key Facts
| Aspect | Details |
|---|---|
| Definition | Complete failure of electrical transmission between heart’s atria and ventricles |
| Symptoms | Slow heart rate, fainting, dizziness, fatigue, chest pain |
| Main Causes | Heart attack, cardiomyopathy, infections, surgery, congenital disorders |
| Diagnosis | ECG confirms independent atrial and ventricular rhythms; clinical assessment and blood tests |
| Treatment | Medications (short-term), pacemaker (permanent solution) |
| Prognosis | Excellent with timely pacemaker intervention; high risk if untreated |
| Complications | Sudden cardiac arrest, syncope, organ dysfunction |
When to Call Your Doctor
Contact your healthcare provider immediately if you have:
- Unusual tiredness
- Weakness or dizziness
- Shortness of breath
- Fainting episodes
- Chest pain
- Symptoms not improving or worsening
- Any new or concerning symptoms
For shortness of breath, chest pain, or loss of consciousness, call 911 without delay. Timely intervention can be life-saving.
Outlook and Living with Third-Degree Heart Block
With modern pacemaker therapy, most people with third-degree heart block lead active, fulfilling lives. Regular follow-up and device checks are required. Good management of underlying cardiac risk factors and adherence to a healthy lifestyle also support long-term heart health.
Key Takeaways
- Third-degree heart block is a serious, life-threatening disruption in heart rhythm.
- Causes include heart disease, surgery, infection, medications, and autoimmune effects.
- Symptoms are often dramatic; emergency response is crucial.
- Diagnosis relies on ECG and clinical assessment.
- Most cases require a permanent pacemaker; outcomes are excellent with proper therapy.
- If you recognize symptoms and risk factors, seek medical attention promptly.
References
- https://www.ummhealth.org/health-library/understanding-third-degree-heart-block
- https://en.wikipedia.org/wiki/Third-degree_atrioventricular_block
- https://www.healthline.com/health/heart-disease/3rd-degree-heart-block
- https://my.clevelandclinic.org/health/diseases/17056-heart-block
- https://www.ncbi.nlm.nih.gov/books/NBK545199/
- https://litfl.com/av-block-3rd-degree-complete-heart-block/
Read full bio of Sneha Tete












