Understanding the Brain-Gut Connection: How Your Gut Health Influences Mind and Body
Discover how the gut and brain communicate, influencing emotional wellbeing, overall health, and disease prevention.
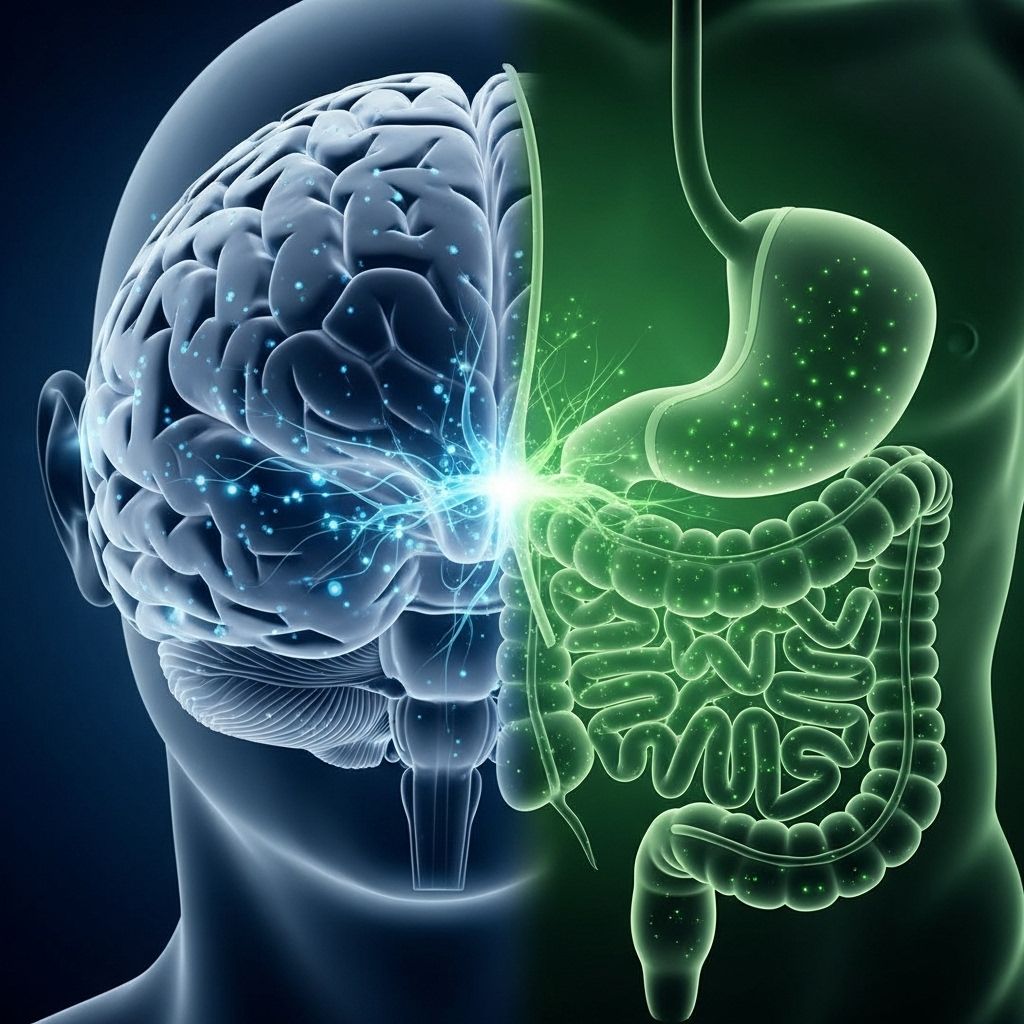
The Brain-Gut Connection: An Introduction
The relationship between the gut and the brain has become one of the most compelling areas in modern medical research. This intricate connection plays a crucial role in mental and physical health, influencing not only digestion but also mood, immunity, and disease risk. Recent studies highlight that the pathways linking the gut and the brain comprise complex systems involving direct nerve signaling, neurotransmitters, and the vast ecosystem of microbes populating the digestive tract.
This article explores the science behind the brain-gut connection, details how it affects wellbeing, and offers practical insights for nurturing a healthier gut—and mind.
What Is the Brain-Gut Axis?
The brain-gut axis refers to the bidirectional communication network between the central nervous system (including the brain) and the enteric nervous system (the ‘brain in your gut’). This network is responsible for controlling digestion and significantly impacting mood and health. Scientists have identified several key components in this axis:
- Nerves: The enteric nervous system contains 200–600 million neurons, which communicate with the brain via the vagus nerve—a major pathway that transmits signals in milliseconds.
- Neurotransmitters: The gut produces approximately 90% of the body’s serotonin and nearly half of its dopamine, both crucial for mood regulation and cognitive focus.
- Gut Microbiota: Trillions of microbes in the gut interact with both bodily and neural processes, shaping local and distant disease risks.
Bidirectional Communication
This two-way system means that not only can psychological stress or brain conditions affect gut function, but disturbances in the gut can also manifest as mental health concerns. Symptoms such as anxiety or depression often occur alongside gastrointestinal issues like irritable bowel syndrome (IBS), colitis, and inflammatory bowel disease.
The Enteric Nervous System: The ‘Second Brain’
The enteric nervous system, embedded throughout the gastrointestinal tract, is sometimes called the second brain due to its complexity and autonomy. It manages the mechanics and sensations of digestion—such as peristalsis or the sensation of ‘butterflies in the stomach’ during stress.
- The ENS houses hundreds of millions of nerve cells, allowing it to operate independently, but it communicates closely with the central nervous system.
- Its ability to produce and respond to neurotransmitters explains why gut disorders frequently overlap with emotional symptoms.
Neurotransmitters: The Chemical Link Between Gut and Brain
Among the most influential gut-brain messengers are neurotransmitters. Serotonin and dopamine, often associated with mood, focus, and happiness, are synthesized in large part by the gut:
- Serotonin: Over 90% is produced by cells in the digestive tract, which helps regulate mood, calm the mind, and serves as a natural antidepressant.
- Dopamine: About half originates from the gut, affecting motivation, attention, and emotional stability.
These neurotransmitters travel through blood and nerve pathways, highlighting how gastrointestinal health can translate to cognitive and emotional wellbeing.
The Microbiome: Microbial Conversations with the Brain
The gut microbiome consists of trillions of microorganisms, including bacteria, viruses, and fungi, residing within the digestive tract. These communities are far from passive passengers—they are crucial for digestion, immunity, and, surprisingly, for mental health.
- Positive Microbes: Beneficial bacteria support enzymatic breakdown of food, vitamin synthesis, and protection against pathogens.
- Microbiome Diversity: A balanced and diverse microbial ecosystem is linked to better emotional regulation, reduced inflammation, and lower disease risk.
- Dysbiosis: An imbalance or loss of healthy bacteria may contribute to mood disorders, inflammatory conditions, weight gain, and even cardiovascular issues.
Microbe-to-Brain Signals
- Microbes produce short-chain fatty acids and other metabolites that influence the production of neurotransmitters and the immune response.
- They shape the permeability of the gut wall, potentially allowing foreign substances to interact with the body, sometimes triggering immune reactions or toxicity.
How Gut Health Influences Disease Risk
Disruptions in the brain-gut axis have been implicated in a wide range of conditions that extend far beyond digestion:
- Mental Health Disorders: Chronic depression, anxiety, schizophrenia, and autism spectrum disorders show strong correlations with gut microbiome changes and altered neurotransmitter levels.
- Diabetes and Heart Disease: The gut may signal metabolic disorders, affect insulin resistance, and drive cardiovascular risk.
- Immune Conditions: Poor gut barrier function can invite inflammation, contributing to disorders like autoimmune disease.
- Cancer: Some evidence links microbiome composition and gut inflammation with cancer risk.
Functional Bowel Disease and Psychosocial Symptoms
Patients with functional bowel disease frequently report additional psychosocial symptoms such as depression or anxiety. Treatments addressing both the brain and gut often yield the most promising results, as medications can affect neurotransmitter activity in both systems.
Stress, Digestion, and the Brain-Gut Axis
Stress is a primary disruptor of the brain-gut axis. The physiological response to stress can:
- Alter gut motility, leading to symptoms like diarrhea or constipation.
- Increase sensitivity in the gut, exacerbating pain or discomfort.
- Reduce the diversity and number of beneficial gut bacteria.
This explains why stressful life events may trigger digestive problems—and why managing stress brings tangible benefits to intestinal health.
Dietary and Lifestyle Strategies for a Healthy Brain-Gut Axis
Improving gut health can significantly influence mental health and overall well-being. Several practical steps include:
- Fiber-Rich Diet: Aim for 15–20 grams of fiber daily from fresh fruits, vegetables, beans, whole grains, and bran cereals. Fiber supports healthy microbiota and forms soft, bulky stool for optimal digestion.
- Hydration: Drink plenty of water to promote regular bowel movements.
- Physical Activity: Regular exercise ensures gut motility and supports microbial diversity. Even 20 minutes daily can be beneficial.
- Behavioral Changes: Heed the urge to defecate, make time for bathroom breaks, and avoid holding in bowel movements, which can stress the gut.
- Review of Medications: Some drugs can disrupt gut function; consult a healthcare provider for alternatives if constipation or gut problems arise.
- Probiotics: Consuming foods with live cultures like yogurt may support microbiome balance.
Table: Gut Health Strategies and Their Benefits
| Strategy | Gut Impact | Mental Health Impact |
|---|---|---|
| High-Fiber Diet | Forms bulkier stool, supports healthy bacteria | Improved mood via increased serotonin production |
| Hydration | Facilitates regular bowel movements | Prevents discomfort, lowers stress response |
| Exercise | Promotes gut motility, aids microbial diversity | Reduces anxiety and depression risk |
| Probiotics | Balances microbiome, supports digestion | Potential cognitive and mood benefits |
FAQs about the Brain-Gut Connection
Q: What is the brain-gut axis?
A: The brain-gut axis is the two-way communication network between the central nervous system (brain and spinal cord) and the enteric nervous system in the digestive tract, impacting gut function, mood, and overall health.
Q: How do neurotransmitters in the gut affect emotional wellness?
A: Serotonin and dopamine produced in the gut help regulate mood, alleviate anxiety, and provide natural antidepressant effects, demonstrating the gut’s influence over emotional states.
Q: Can an unhealthy gut cause mental health problems?
A: Yes. Imbalanced gut microbiota or disrupted neurotransmitter production can contribute to depression, anxiety, and other psychiatric disorders. Similarly, the gut can be affected by stress or mental illness, worsening gastrointestinal symptoms.
Q: Which foods support a healthy brain-gut connection?
A: Foods rich in fiber, prebiotics, and probiotics—such as fruits, vegetables, whole grains, beans, and fermented foods—support beneficial bacteria and healthy neurotransmitter production.
Q: How can I relieve constipation and support gut health?
- Include high-fiber foods in your diet.
- Drink adequate water daily.
- Be physically active—aim for at least 20 minutes each day.
- Take time for regular bowel movements and avoid ignoring the urge.
- Review medications with your doctor to avoid causative agents.
Looking Ahead: The Future of Brain-Gut Research
The scope of brain-gut research is expanding rapidly. Innovative centers like the Johns Hopkins Food, Body & Mind Center are investigating how gut health relates to chronic illnesses ranging from diabetes and heart disease to cancer and psychiatric disorders. New therapies—including dietary interventions, pharmaceuticals targeting neurotransmitter systems, and microbiome modulation—are emerging as promising ways to optimize both mental and physical wellbeing.
Summary: Why the Brain-Gut Connection Matters
- The brain and gut communicate constantly, shaping digestion, immunity, and emotions.
- Gut microbiota and neurotransmitters like serotonin influence mood and disease risk.
- Stress and poor gut health can trigger digestive and emotional problems.
- Diet, lifestyle, and medication review are key to supporting a balanced brain-gut axis.
- Ongoing research promises new preventive and therapeutic strategies for complex health challenges.
Through deeper understanding and daily lifestyle choices, every person has the power to nurture a healthy gut—and, by extension, a healthy mind.
References
- https://www.hopkinscim.org/breakthrough/winter-2014/food-body-mind/
- https://www.jhunewsletter.com/article/2018/11/its-not-all-in-your-head-the-brain-and-gut-connection
- https://blogs.pathology.jhu.edu/pathology/the-brain-in-your-gut
- https://cdhf.ca/en/constipation-and-the-brain-gut-axis/
- https://magazine.publichealth.jhu.edu/2021/gut-microbiome-and-brain
- https://www.scirp.org/reference/referencespapers
- https://livea.com/blog/2022/03/28/how-does-gut-health-affect-brain-health/
Read full bio of medha deb












