Tetralogy of Fallot: Comprehensive Guide to a Congenital Heart Defect
Understand Tetralogy of Fallot: Causes, symptoms, diagnosis, treatments, and living with this congenital heart defect.
Tetralogy of Fallot (TOF): A Comprehensive Overview
Tetralogy of Fallot (TOF) is the most common form of cyanotic congenital heart disease, representing a significant portion of cases in pediatric cardiology. It is defined by four heart abnormalities present at birth, all of which affect the flow of blood through the heart and to the rest of the body. This guide provides an in-depth look at the anatomy, symptoms, causes, diagnostic approach, treatment, and life with Tetralogy of Fallot.
What is Tetralogy of Fallot?
Tetralogy of Fallot is a rare, complex heart defect that involves four key structural heart abnormalities. These combined defects reduce the oxygen content of blood pumped to the body, leading to cyanosis—a bluish coloring of the skin due to insufficient oxygenation. TOF is a congenital condition, meaning it is present at birth, and is the most common cyanotic heart defect seen beyond infancy.
- Accounts for approximately 10% of all congenital heart diseases.
- Named for its four (“tetra-“) distinct heart abnormalities.
- Most frequently diagnosed in infancy due to visible symptoms but can go undiagnosed until later childhood or even adulthood in milder cases.
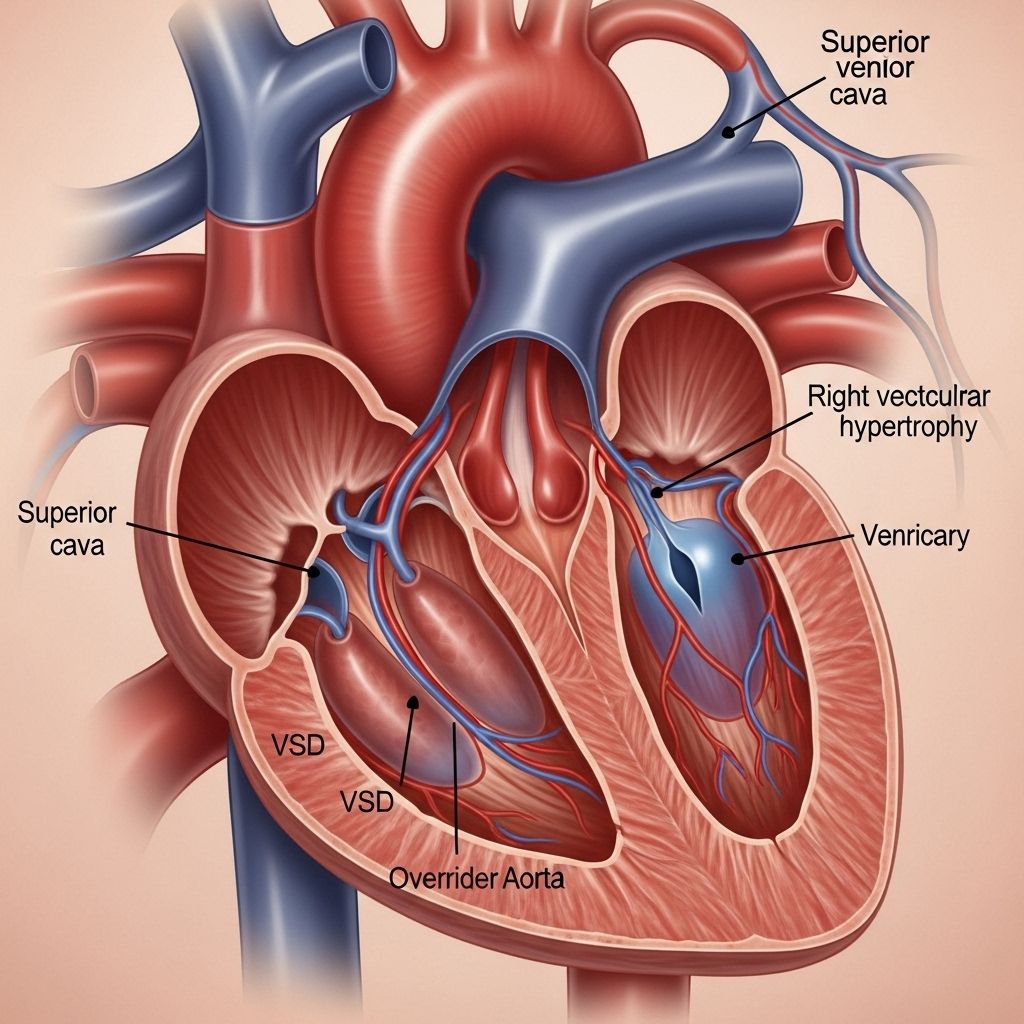
The Four Abnormalities of Tetralogy of Fallot
The classic features of TOF are highlighted below, each contributing to impaired blood flow and oxygenation:
| Abnormality | Description | Effect on Heart Function |
|---|---|---|
| Ventricular Septal Defect (VSD) | A large hole in the septum (wall) between the left and right ventricles | Allows mixing of oxygen-poor and oxygen-rich blood, reducing overall oxygenation |
| Pulmonary Stenosis | Narrowing of the right ventricular outflow tract and/or pulmonary valve | Obstructs blood flow from the right ventricle to the lungs, lowering oxygen pick-up |
| Overriding Aorta | The aorta is positioned above the VSD and receives blood from both ventricles | Increases mixing of oxygen-poor blood into the systemic circulation |
| Right Ventricular Hypertrophy | Thickening of the muscular wall of the right ventricle | Develops as the right ventricle must work harder to overcome pulmonary stenosis |
In addition to these classic findings, some patients may also have a right-sided aortic arch or, less commonly, an atrial septal defect (hole between the upper chambers).
Causes and Risk Factors
The precise cause of Tetralogy of Fallot remains largely unknown. It arises due to improper development of the fetal heart during pregnancy. Genetic and environmental factors may play a role, and in some cases, there may be an association with chromosomal disorders.
- Genetic factors: Familial cases and certain chromosomal abnormalities, such as DiGeorge syndrome (22q11.2 deletion), may increase risk.
- Maternal factors: Conditions like diabetes, poor nutrition, viral illnesses, or certain medications or substances taken during pregnancy could contribute.
- Most cases occur sporadically with no definite cause identified.
Fetal Heart Development
The heart forms early in fetal development, and Tetralogy of Fallot results from disturbances in the partitioning of the heart chambers and formation of the outflow tracts.
Symptoms and Clinical Presentation
The degree and onset of symptoms in TOF vary depending on the severity of the anatomical defects, especially the extent of right ventricular outflow obstruction. The hallmark symptom is cyanosis—blue or grayish coloration of the lips, skin, and nail beds, reflecting low blood oxygen levels. Other signs and symptoms can include:
- Difficulty breathing, especially during feeding or exertion
- Poor weight gain and growth (“failure to thrive”)
- Easily tired (especially with feeds in infants)
- Clubbing (widening/rounding of the fingertips and toes)
- Heart murmur detected during physical examination
- Tet spells: Sudden episodes of deep cyanosis, shortness of breath, irritability, or fainting, especially during crying or feeding
Special Note: Tet Spells
Tet spells are moments when the oxygen level drops further and can be life-threatening if prolonged. Children may instinctively squat to improve blood flow and relieve symptoms.
How is Tetralogy of Fallot Diagnosed?
Early diagnosis is crucial for optimal management of TOF. The condition may be suspected based on physical findings (heart murmur, cyanosis) and confirmed using imaging and other specialized tests. Diagnosis typically occurs:
- During pregnancy via prenatal ultrasound (fetal echocardiography)
- Soon after birth given evident cyanosis or heart murmur
- On rare occasions, later in life if symptoms were milder and previously missed
Diagnostic Tests
- Echocardiogram (Echo): The primary test to visualize heart structures and blood flow.
- Electrocardiogram (ECG): Evaluates electrical activity and detects right ventricular hypertrophy.
- Chest X-ray: May show a characteristic “boot-shaped” (coeur en sabot) heart.
- Pulse oximetry: Detects low blood oxygen saturation.
- Cardiac catheterization: Used when further evaluation of anatomy or pressures is needed, often before surgery.
Treatment Options for Tetralogy of Fallot
Most children with TOF require surgical repair. Advances in neonatal cardiac care have made early and successful intervention the standard, greatly improving outcomes.
- Complete surgical repair: The preferred approach for most infants, usually performed within the first year of life. This complex open-heart procedure closes the VSD and relieves right ventricular outflow obstruction (removing narrowed muscle/valve tissue).
- Temporary (palliative) procedures: Reserved for those in whom full repair is unsafe initially. For example, a Blalock-Taussig shunt may be placed to increase pulmonary blood flow while the baby grows.
What Happens During Complete Repair?
- The surgeon closes the ventricular septal defect with a patch.
- Narrowed sections of the right ventricular outflow tract and/or pulmonary valve are widened or removed to improve blood flow to the lungs.
- If the pulmonary valve is absent or severely malformed (pulmonary atresia), a new pathway may be constructed.
After Surgery
Most children recover well, though ongoing follow-up is necessary. Potential long-term issues can include: pulmonary valve leakage or stenosis, arrhythmias, or need for further surgeries later in life.
Outlook and Long-Term Prognosis
Modern surgical techniques have vastly improved the life expectancy and quality of life for those born with Tetralogy of Fallot. Many individuals go on to live healthy, active lives.
- Lifelong follow-up with cardiologists specializing in congenital heart disease is strongly recommended.
- Potential for late complications, such as arrhythmias (irregular heart rhythms), residual or recurrent pulmonary stenosis, or right ventricular dysfunction, means ongoing surveillance is important.
- Many patients require additional procedures, especially to address pulmonary valve issues, during adolescence or adulthood.
Living with Tetralogy of Fallot
After successful repair, most children can participate in normal activities, attend school, and grow along with their peers. Some key aspects of living with repaired TOF include:
- Regular cardiac check-ups and imaging to monitor heart function
- Careful management during situations that increase heart strain (such as exercise or certain illnesses)
- Antibiotic prophylaxis before some dental or surgical procedures may be advised to prevent endocarditis (heart infection)
- Specialized transition of care from pediatric to adult congenital heart specialists is essential
Physical Activity
Most patients can participate in sports, but some may need to avoid competitive, high-intensity activities depending on heart function and their cardiologist’s recommendations.
Pregnancy and Adulthood
Women with repaired TOF can often have successful pregnancies, but careful planning and specialized medical oversight are needed to minimize risks.
Frequently Asked Questions (FAQs)
Q: What are the four components of Tetralogy of Fallot?
A: The four classic abnormalities are: ventricular septal defect (VSD), pulmonary stenosis, overriding aorta, and right ventricular hypertrophy.
Q: How common is Tetralogy of Fallot?
A: TOF accounts for approximately 10% of all cases of congenital heart disease and is the most common cyanotic congenital heart disorder found beyond infancy.
Q: Can Tetralogy of Fallot be detected before birth?
A: Yes, many cases are suspected during routine prenatal ultrasounds and confirmed by fetal echocardiography. Early diagnosis allows for proper planning of care at birth.
Q: Will my child need more than one heart surgery?
A: Some patients may require additional surgeries in adolescence or adulthood, especially to address pulmonary valve issues or arrhythmias, even after an initial repair.
Q: What is the long-term outlook for someone with repaired TOF?
A: With contemporary surgical techniques and specialty care, the majority of patients with repaired TOF now have a normal or near-normal lifespan and can lead full, active lives.
Resources and Support
Living with or caring for someone with TOF can be challenging. Educational materials and support groups—such as those provided by the American Heart Association, the Children’s Heart Foundation, and local congenital heart defect organizations—are helpful resources for families and adult survivors.
Summary
Tetralogy of Fallot is a serious but increasingly treatable form of congenital heart disease. Understanding its anatomy, symptoms, diagnostic and treatment approaches, and the importance of lifelong follow-up empowers families and patients to achieve the best possible outcomes. Advances in pediatric and adult congenital cardiology continue to improve the prognosis and quality of life for those affected by TOF.
References
- https://www.mayoclinic.org/diseases-conditions/tetralogy-of-fallot/symptoms-causes/syc-20353477
- https://www.pted.org/?id=tetralogyfallot1
- https://rarediseases.org/rare-diseases/tetralogy-of-fallot/
- https://pubmed.ncbi.nlm.nih.gov/7888802/
- https://pure.johnshopkins.edu/en/publications/tetralogy-of-fallot-6
- https://pure.johnshopkins.edu/en/publications/tetralogy-of-fallot-5
Read full bio of medha deb












