Understanding T-Cell Leukemia: Symptoms, Diagnosis, Treatment, and Prognosis
An in-depth guide to T-cell leukemia: symptoms, causes, diagnosis, treatment options, and long-term outlook for patients.
What to Know About T-Cell Leukemia
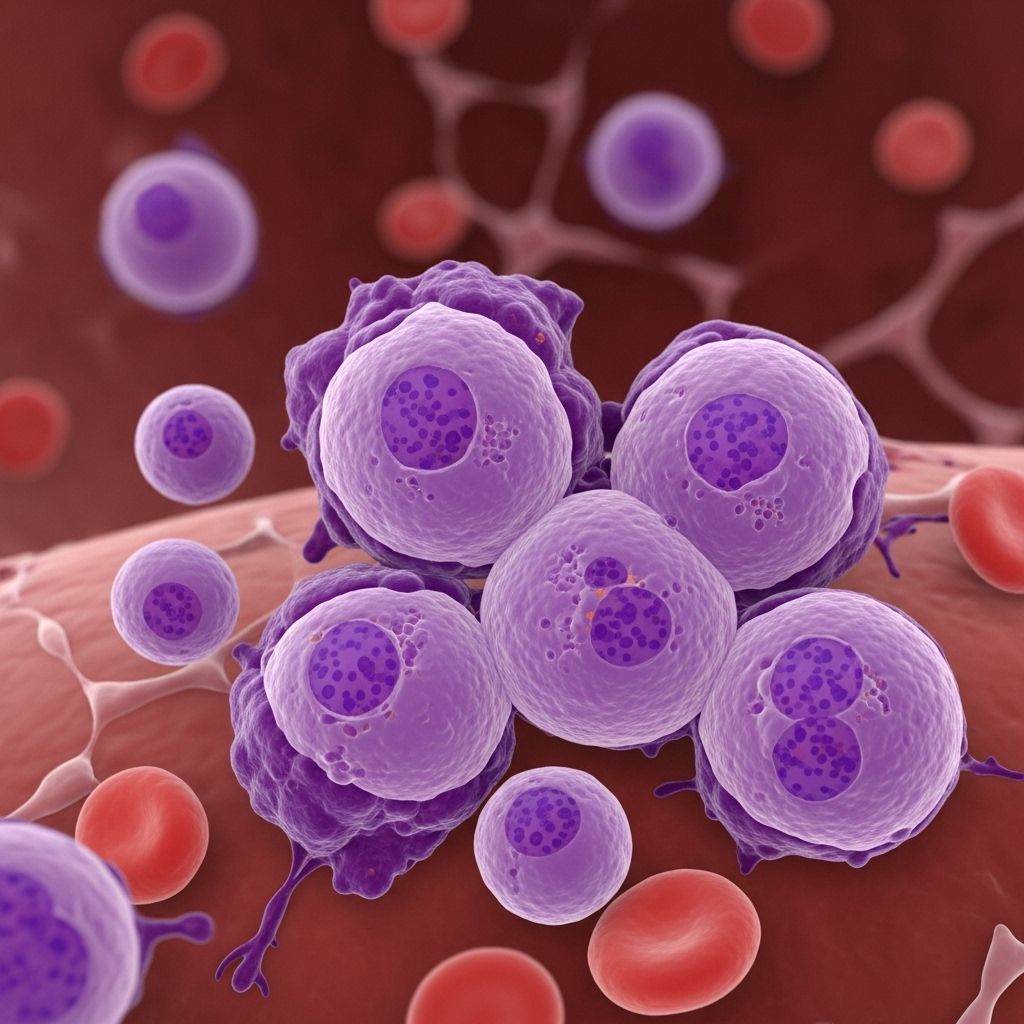
T-cell leukemia is a rare but aggressive cancer that affects a specific kind of white blood cell known as T-cells. These cells play a critical role in defending the body against infections and disease. The disease disrupts your body’s immune system by causing unchecked growth of abnormal T-cells, which crowd out healthy blood cells and undermine normal bodily functions.
- T cells are a type of lymphocyte, a white blood cell responsible for immune defense.
- Abnormal growth and division caused by damaged DNA in T-cell precursors are the basis of this disease.
- The most studied T-cell leukemia type is prolymphocytic leukemia (T-PLL), though other subtypes exist, such as T-cell acute lymphoblastic leukemia (T-ALL).
T-cell leukemia often requires prompt diagnosis and aggressive treatment due to its fast progression and potentially life-threatening consequences.
What Is T-Cell Leukemia?
Leukemia encompasses a group of cancers impacting blood and blood-forming tissues like bone marrow. The primary mechanism is the overproduction of abnormal or immature white blood cells, which then crowd out healthy cells, impeding the body’s ability to combat infections.
T-cell leukemia is specifically characterized by:
- Excess production of immature or abnormal T-cells.
- Impaired development of these cells within bone marrow and the thymus.
Subtypes of T-cell leukemia include:
- T-cell prolymphocytic leukemia (T-PLL): The most frequently studied T-cell leukemia; it’s aggressive and typically presents in older adults.
- T-cell acute lymphoblastic leukemia (T-ALL): More common in children and young adults, accounting for 10–15% of childhood and 25% of adult acute lymphoblastic leukemia cases.
Classification of Leukemia
| Chronic | Acute | |
|---|---|---|
| Myeloid | Chronic Myeloid Leukemia (CML) | Acute Myeloid Leukemia (AML) |
| Lymphocytic | Chronic Lymphocytic Leukemia (CLL) | Acute Lymphoblastic Leukemia (ALL) |
T-ALL is a subcategory of acute lymphoblastic leukemia, originating from immature T-cells.
Symptoms
T-cell leukemia usually presents with non-specific, yet rapidly worsening symptoms. Recognizing these early can help facilitate prompt diagnosis and treatment.
- Persistent fever
- Fatigue and unexplained weakness
- Unusual bleeding or bruising, such as nosebleeds, bleeding gums, or small red spots under the skin (petechiae)
- Recurring infections
- Swollen lymph nodes in neck, groin, or armpits
- Night sweats
- Bone or joint pain
- Unintentional weight loss
- Enlarged spleen or liver, causing abdominal discomfort
Causes and Risk Factors
The precise causes of T-cell leukemia remain unclear, but several risk factors have been identified:
- Genetic mutations in bone marrow stem cells
- Radiation exposure, especially previous cancer treatments involving radiotherapy
- Chemical exposure, including contact with industrial chemicals like benzene
- Certain viral infections such as human T-cell lymphotropic virus (HTLV-1), which predisposes individuals to T-cell leukemia
- Inherited genetic syndromes, for instance Down syndrome and certain immune deficiencies
Most cases occur sporadically with no clear inherited or environmental trigger.
Diagnosis
Diagnosis of T-cell leukemia often follows the presentation of symptoms and is confirmed by analyzing blood and bone marrow samples:
- Physical examination: Looking for lymph node enlargement, spleen or liver swelling, and other physical signs.
- Complete blood count (CBC): Measures numbers of red cells, platelets, and white cells, often revealing a high white cell count.
- Blood smear and differential: Microscopic examination of blood for abnormal cell types.
- Bone marrow biopsy: Extraction and analysis of marrow tissue to confirm abnormal T-cell proliferation.
- Flow cytometry: Special lab tests to identify cell type by surface proteins.
- Genetic and molecular tests: Detection of DNA mutations associated with T-cell leukemia.
Prompt diagnosis is vital, given the speed at which certain T-cell leukemias (notably T-ALL and T-PLL) can progress and threaten life without immediate management.
Subtypes of T-Cell Leukemia
While there are several types of T-cell leukemia, two subtypes are most commonly discussed:
- T-ALL (T-cell Acute Lymphoblastic Leukemia): Aggressive and nearly always requires rapid treatment. More common in children and young adults.
- T-PLL (T-cell Prolymphocytic Leukemia): Also aggressive but typically occurs in older adults and is associated with a very high white blood cell count.
| Subtype | Typical Age Onset | Features | Prognosis |
|---|---|---|---|
| T-ALL | Children (~9 years), Adults (~30 years) | Rapid onset, CNS involvement, mediastinal masses | Children: up to 80% 5-year survival; Adults: <50% |
| T-PLL | Median onset in older adults | Very high white cell counts, rapid progression | Poor; requires aggressive intervention |
Treatment
Treatment strategies for T-cell leukemia are tailored according to disease subtype, stage, patient health, and response to initial therapy. Aggressive intervention is often required, especially for T-ALL and T-PLL.
- Chemotherapy: The mainstay for most T-cell leukemia types, involving single or multiple drugs given orally, intravenously, or directly into the spinal fluid (intrathecal). Children often tolerate stronger chemotherapy regimens than adults.
- Radiation therapy: Used to target leukemia in the thymus, brain, or spinal cord. It utilizes focused energy beams to destroy malignant cells while preserving healthy tissue.
- Targeted therapy: Drugs designed to attack specific proteins or genetic changes seen in leukemia cells, sparing normal cells. Options are still relatively limited for T-cell leukemia.
- Stem cell transplant (bone marrow transplant): Considered for patients achieving remission after chemotherapy. It replaces defective stem cells with healthy ones from a donor or harvested from the patient’s own body before treatment.
- Clinical trials: Some centers offer experimental therapies or investigational drugs not yet part of standard care, providing access to new treatments.
- Supportive care: Addresses symptoms and side effects:
- Antibiotics for infection control
- Blood transfusions for low platelet/red cell counts
- Counseling to manage emotional impact
- Diet and nutritional support
- Pain management and exercise when possible
The choice of treatment depends heavily on individual circumstances, including age, general health, and response to previous therapies. Relapse is common, especially in adults, and may necessitate alternative approaches.
Outlook and Prognosis
T-cell leukemia prognosis varies by subtype, age at diagnosis, the extent of disease, and response to treatment:
- Children with T-ALL: Up to 80% achieve long-term remission with proper treatment.
- Adults with T-ALL: Less than 50% achieve a cure.
- T-PLL: Generally poor prognosis even with aggressive therapy, due to rapid progression and frequent relapse.
Common factors influencing prognosis:
- Early diagnosis and immediate treatment significantly improve outcomes.
- Complete remission after initial therapy leads to better survival rates.
- Relapse within the first two years post-treatment is seen in about one-third of cases, particularly in adults.
- Five-year survival for children is approximately 75%; for adults, around 60%.
Advances in treatment, especially for children, have steadily improved survival rates. However, adult outcomes remain challenging, and relapse management is an ongoing area of research.
Living with T-Cell Leukemia
Managing life with T-cell leukemia involves ongoing medical care as well as lifestyle adjustments to cope with the physical and emotional effects of the disease and its treatments.
- Regular monitoring through blood tests and clinical appointments
- Proactive infection prevention
- Management of treatment side effects (nausea, fatigue, mouth sores, low immunity)
- Support from family, peer networks, and counseling
- Healthy diet, gentle physical activity, and adequate rest
Participation in support groups and connecting with others experiencing leukemia can also provide valuable emotional support.
Summary
T-cell leukemia represents a rare but aggressive group of blood cancers with variable clinical presentations and challenging treatments. Early recognition, prompt diagnosis, and tailored interventions can improve patient outcomes, particularly for children and young adults. Advances in research continue to develop better-targeted therapies, but managing relapse and supporting long-term quality of life remain key considerations.
Frequently Asked Questions (FAQs)
Q: What is the difference between T-cell leukemia and lymphoma?
A: T-cell leukemia originates in the blood and bone marrow, while T-cell lymphoma starts in lymphatic tissues such as lymph nodes. Both involve abnormal growth of T-cells but differ primarily in their site of origin and clinical presentation.
Q: How is T-cell leukemia diagnosed?
A: Diagnosis involves blood tests, bone marrow biopsy, and advanced laboratory analysis (flow cytometry and genetic/molecular testing) to detect abnormal T-cell populations and DNA mutations.
Q: Is T-cell leukemia curable?
A: Cure rates depend on age, subtype, and response to treatment. Children with T-ALL can be cured up to 80% of the time, while adults fare less well. T-PLL remains difficult to cure and typically requires aggressive therapy.
Q: What are the most common symptoms of T-cell leukemia?
A: Unexplained fatigue, frequent infections, bruising or bleeding, swollen lymph nodes, and persistent fever are the key symptoms.
Q: Who is at risk of developing T-cell leukemia?
A: Risk factors include genetic mutations, radiation or chemical exposures, certain viral infections, and genetic syndromes. Most cases, however, arise without a clear inherited risk.
Resources
- Leukemia & Lymphoma Society
- American Cancer Society
- National Cancer Institute
- Support forums and patient advocacy groups
References
- https://leukemiarf.org/leukemia/acute-lymphoblastic-leukemia/t-cell-lymphoblastic-leukemia/
- https://www.healthline.com/health/leukemia/t-cell-acute-lymphoblastic-leukemia
- https://www.healthline.com/health/leukemia/t-cell-leukemia
- https://www.nature.com/articles/s12276-024-01335-7
- https://www.healthline.com/health/video/cll-community-stories-2
- https://www.ncbi.nlm.nih.gov/books/NBK558968/
- https://www.medicalnewstoday.com/articles/321692
- https://californiahealthline.org/news/article/california-expanded-health-coverage-immigrants-medicaid-disenrollment/
- https://www.lymphoma.org/understanding-lymphoma/aboutlymphoma/nhl/atll/
Read full bio of Sneha Tete












