Understanding T-Cell Acute Lymphoblastic Leukemia: Symptoms, Causes, and Treatments
An in-depth guide to T-cell acute lymphoblastic leukemia (T-ALL) covering causes, symptoms, diagnosis, treatment, and prognosis.
T-Cell Acute Lymphoblastic Leukemia: Your Comprehensive Guide
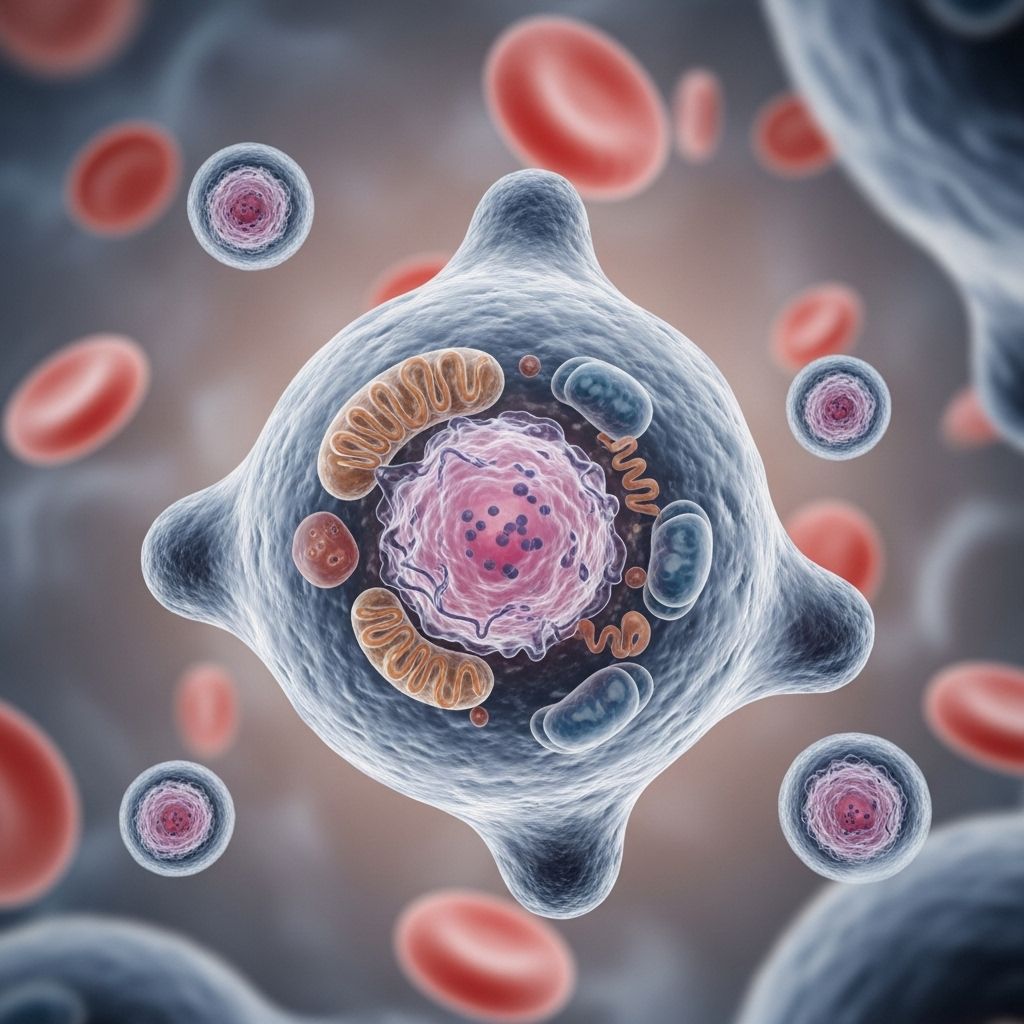
T-cell acute lymphoblastic leukemia (T-ALL) is an aggressive blood cancer that arises from immature T-cells in the bone marrow. This detailed guide explores what T-ALL is, its possible causes, symptoms, diagnosis, treatment, and outlook, providing essential knowledge for anyone navigating this condition.
What Is T-Cell Acute Lymphoblastic Leukemia?
Leukemia is a broad category of blood cancers caused by the uncontrolled production of abnormal or immature blood cells in the bone marrow. There are two major ways leukemias are classified:
- Acute: Develops and progresses quickly if not treated.
- Chronic: Develops slowly and progresses over a longer period.
Leukemias are further grouped by the type of blood cells they affect:
- Lymphocytic leukemias: Originate in lymphocytes, which become natural killer (NK) cells, T-cells, and B-cells.
- Myeloid leukemias: Originate in myeloid cells, precursors of red blood cells, certain white blood cells, and platelets.
| Chronic | Acute | |
|---|---|---|
| Myeloid | Chronic myeloid leukemia (CML) | Acute myeloid leukemia (AML) |
| Lymphocytic | Chronic lymphocytic leukemia (CLL) | Acute lymphoblastic leukemia (ALL) |
T-ALL is a subtype of acute lymphoblastic leukemia (ALL) specifically affecting immature T-cell progenitors. In T-ALL, the bone marrow produces a large number of immature T-cells (also called lymphoblasts), which crowd out healthy blood cells and compromise the immune system.
How Does T-ALL Develop?
T-ALL develops when stem cells in the bone marrow acquire genetic mutations that cause them to proliferate uncontrollably and fail to mature into healthy T-cells. As a result:
- Abnormal T-cells accumulate in the bone marrow, blood, and sometimes in organs like the lymph nodes, liver, or spleen.
- Healthy blood cell production falls, leading to symptoms like anemia, infection, and bleeding.
Who Is at Risk?
- T-ALL is less common than B-cell ALL, representing about 10-15% of childhood and up to 25% of adult ALL cases.
- It affects both children and adults, with a slight male predominance.
Causes and Risk Factors
The exact cause of T-ALL is unknown, but several risk factors and genetic factors have been identified:
- Environmental exposures: Ionizing radiation and chemicals like benzene may increase risk.
- Genetic syndromes: Conditions such as Down syndrome, neurofibromatosis, and certain other inherited disorders.
- Viral infections: Some viruses, such as the human T-lymphotropic virus type I (HTLV-1), have been linked to certain leukemias.
- Genetic mutations: Changes in bone marrow stem cell DNA, especially mutations affecting cell growth and survival pathways.
Still, most cases of T-ALL do not have a clearly identifiable risk factor.
Symptoms of T-Cell Acute Lymphoblastic Leukemia
Symptoms of T-ALL develop quickly due to the rapid increase in immature abnormal cells. Key symptoms include:
- Frequent infections (due to low healthy white blood cell count)
- Easy bruising or bleeding (from low platelet count)
- Fatigue, weakness, or pale skin (caused by anemia)
- Fever
- Bone pain or joint pain
- Swollen lymph nodes
- Abdominal swelling (from enlarged liver or spleen)
- Shortness of breath
Sometimes, T-ALL cells can infiltrate the chest, causing swelling of the thymus or mediastinum, which may press on airways or major blood vessels, leading to cough, chest pain, or breathing difficulties.
How Is T-ALL Diagnosed?
The diagnostic process for T-ALL typically includes:
- Medical history and physical exam
- Blood tests: Complete blood count (CBC) to check for abnormal levels of blood cells
- Bone marrow aspiration and biopsy: To identify abnormal T-cells and confirm diagnosis
- Immunophenotyping: Detects specific cell markers to determine the type of leukemia
- Cytogenetic and molecular testing: To reveal genetic mutations that may guide treatment choices
- Imaging studies: Such as X-rays, ultrasound, or CT scans to assess involvement of the chest, liver, spleen, or lymph nodes
- Lumbar puncture: To check for leukemia cells in the cerebrospinal fluid
Types and Subtypes of T-ALL
T-ALL can be classified according to the stage of T-cell development affected and certain molecular features.
- Early T-cell precursor (ETP) ALL: A unique, high-risk subtype with distinct genetic and immunophenotypic characteristics. ETP-ALL exhibits features of both T-cells and myeloid cells and is often more challenging to treat.
- Other subtypes: Defined by the expression patterns of T-cell markers and specific genetic mutations, such as NOTCH1, CDKN2A, or abnormalities in signaling pathways (e.g., RAS pathway, JAK/STAT, PI3K/AKT).
Treatment Options for T-ALL
Treatment for T-ALL is intensive and typically involves several phases. The approach depends on a combination of factors, including age, overall health, genetic features of leukemia cells, and the response to initial therapy. Main treatments include:
1. Chemotherapy
Chemotherapy is the foundation of T-ALL treatment. It destroys rapidly dividing cells, including cancerous and some healthy cells. A typical regimen includes:
- Induction phase: Intense chemotherapy to reduce leukemia cells to undetectable levels.
- Consolidation phase: Further chemo to eliminate remaining cells and prevent relapse.
- Maintenance phase: Lower-intensity treatment to maintain remission and minimize relapse risk.
Common chemotherapy drugs for T-ALL include:
- Steroids (e.g., prednisone, dexamethasone)
- Vincristine
- Cyclophosphamide
- Anthracyclines (e.g., doxorubicin)
- Methotrexate
- 6-Mercaptopurine
- Cytarabine
- L-asparaginase
2. Targeted Therapy
Some patients may benefit from targeted therapies that block specific proteins or pathways involved in T-ALL growth. Examples include:
- Agents targeting the NOTCH1 pathway (for patients with NOTCH1 mutations)
- JAK inhibitors (for JAK/STAT mutations)
- Other emerging agents studied in clinical trials
3. Stem Cell (Bone Marrow) Transplant
High-risk or relapsed T-ALL may be treated with an allogeneic stem cell transplant (transplant using donor stem cells). This is usually considered after achieving remission with chemotherapy and is not suitable for all patients due to risks and eligibility requirements.
4. Central Nervous System (CNS) Prophylaxis
CNS involvement is a risk in T-ALL. Treatment often includes intrathecal chemotherapy (delivered directly into the spinal fluid) to prevent or treat CNS disease.
5. Supportive Care
- Blood transfusions for anemia or low platelets
- Antibiotics to prevent or treat infections
- Management of side effects such as nausea, mouth sores, and organ toxicity
Prognosis and Survival Rates
Prognosis is influenced by age, genetic mutations, initial response to treatment, and other factors:
- Children: Long-term survival rates of up to 80% with modern therapies
- Adults: Lower survival, around 40-50% due to higher toxicity and relapse rates
- About 20% of children and more adults experience relapse or refractory disease
- A minority of cases, particularly with high-risk genetic profiles, may not respond as well to standard therapies
Prognosis is best when T-ALL is diagnosed early and responds rapidly to induction therapy, with minimal residual disease (MRD) after initial chemotherapy being a strong positive predictor.
Living With T-ALL: Coping, Follow-up, and Support
The journey with T-ALL can be long and physically demanding. Survivors require ongoing follow-ups:
- Regular blood tests to detect recurrence
- Ongoing monitoring for late effects of treatment (e.g., heart, liver, or bone issues)
- Psychosocial support to help cope with emotional challenges
Support can come from:
- Oncology social workers and counselors
- Leukemia or cancer support organizations
- Peer support groups and survivorship programs
Frequently Asked Questions (FAQs)
Q: How is T-ALL different from B-cell acute lymphoblastic leukemia?
A: T-ALL affects immature T-cell progenitors, while B-cell acute lymphoblastic leukemia (B-ALL) affects B-cell precursors. Treatments and outcomes may vary due to differences in cell biology and genetic features.
Q: What are the early warning signs of T-ALL?
A: Common early signs include frequent infections, unexplained bruising or bleeding, persistent fevers, fatigue, bone pain, and swollen lymph nodes.
Q: Can T-ALL recur after treatment?
A: Yes. Relapse occurs in about 20% of children and a higher percentage of adults. Surveillance and follow-up care are critical to detect and address recurrence early.
Q: Are there newer therapies or clinical trials available for T-ALL?
A: Research is ongoing. New targeted therapies, immunotherapies, and combination regimens are under investigation. Patients with relapsed or refractory T-ALL may have access to clinical trials of novel agents.
Q: Is a stem cell transplant always necessary?
A: No. Transplants are often reserved for high-risk or relapsed patients, particularly if they do not respond fully to standard chemotherapy or have poor prognostic markers.
Key Takeaways
- T-ALL is an aggressive but increasingly treatable form of leukemia affecting T-cell development.
- Early diagnosis and multi-phase therapy are essential for achieving remission and preventing relapse.
- Ongoing research continues to improve survival rates, especially for relapsed and high-risk cases.
- Support systems and routine follow-up care are crucial for the physical and emotional health of survivors and their families.
References
- https://www.healthline.com/health/leukemia/t-cell-acute-lymphoblastic-leukemia
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8447273/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8394887/
- https://www.medicalnewstoday.com/articles/t-cell-acute-lymphoblastic-leukemia
- https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2020.00273/full
- https://www.healthline.com/health/acute-lymphocytic-leukemia-all
- https://www.healthline.com/health/leukemia/childhood-all-leukemia
- https://www.nature.com/articles/bcj201753
Read full bio of Sneha Tete












