Systolic vs. Diastolic Heart Failure: Understanding the Key Differences and Care
Explore the distinctions between systolic and diastolic heart failure, symptoms, diagnosis, treatments, and what this means for your heart health.
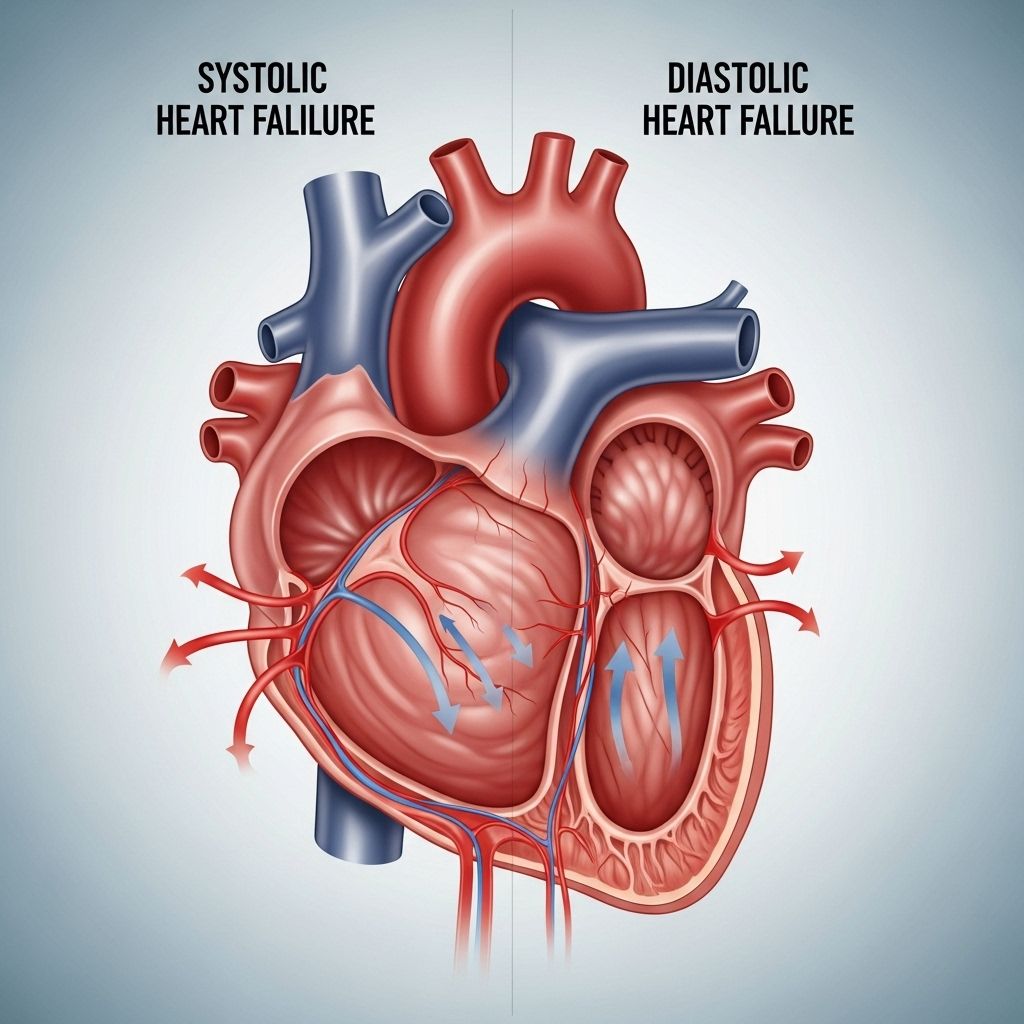
Systolic vs. Diastolic Heart Failure: Whats the Difference?
Heart failure is a complex condition affecting millions worldwide. It is not a single disease, but a syndrome with diverse presentations, primarily categorized as systolic or diastolic heart failure. Understanding the distinctions, symptoms, causes, diagnostic strategies, and treatment options is crucial for effective management and improved quality of life.
What Is Heart Failure?
Heart failure occurs when the heart cannot pump enough blood to meet the bodys needs. This can be caused by problems in the contraction or relaxation phase of the heart cycle, leading to systolic or diastolic heart failure, respectively. Both types can significantly impact health, leading to symptoms such as shortness of breath, fatigue, and swelling in the legs or abdomen.
Systolic Heart Failure
Systolic heart failure, also known as heart failure with reduced ejection fraction (HFrEF), arises when the heart muscle, particularly the left ventricle, cannot contract effectively. As a result, the heart fails to eject a sufficient amount of blood with each beat.
Ejection fraction (EF) measures how much blood the left ventricle pumps out with each contraction. In systolic heart failure, the EF typically falls below 40%.
Key Symptoms of Systolic Heart Failure
- Shortness of breath, especially on exertion or when lying flat
- Persistent fatigue or weakness, even after resting
- Swelling (edema) in the legs, ankles, or abdomen
- Increase in body weight due to fluid retention
- Clear, frothy cough that may worsen at night
- Difficulty sleeping while lying down
- Confusion or trouble concentrating
- Decreased urine output
- Poor appetite or feeling full quickly
How Systolic Heart Failure Is Diagnosed
- Physical Examination: A healthcare provider checks for signs of fluid overload, abnormal heart sounds, and lung congestion.
- Echocardiogram: This imaging test measures ejection fraction. An EF below 40% is suggestive of systolic heart failure.
- Blood Tests: Checking for markers like B-type natriuretic peptide (BNP) can help assess heart failure severity.
- Other Imaging: X-rays or MRI may be used to evaluate heart size, structure, and function.
Diastolic Heart Failure
Diastolic heart failure, also known as heart failure with preserved ejection fraction (HFpEF), happens when the left ventricle becomes stiff and cannot relax properly between heartbeats. This stiffness impairs the hearts ability to fill with blood, even though the ejection fraction may appear normal (typically >50%).
Key Symptoms of Diastolic Heart Failure
The symptoms of diastolic heart failure largely overlap with those of systolic heart failure and include:
- Shortness of breath, particularly during activity or lying down
- Fatigue and weakness
- Swelling of the lower legs and abdomen
- Sudden weight gain from fluid buildup
- Frequent urge to urinate at night
- Rapid or irregular heartbeat
How Diastolic Heart Failure Is Diagnosed
- Imaging: An echocardiogram usually shows a normal ejection fraction, but additional tests are needed to detect stiffness or impaired filling of the ventricle.
- Medical History: Many people with diastolic heart failure are older or have conditions such as high blood pressure, diabetes, obesity, or kidney disease.
- Other Diagnostic Criteria: Doctors consider symptoms, imaging findings, and other markers to confirm the diagnosis.
Diastolic vs. Systolic Heart Failure: A Comparison
| Aspect | Systolic Heart Failure | Diastolic Heart Failure |
|---|---|---|
| Main issue | Weakened contraction (pumping problem) | Stiffness and impaired relaxation (filling problem) |
| Ejection fraction (EF) | Reduced (< 40%) | Normal or near-normal (≥ 50%) |
| Common in | Younger individuals; often men | Older adults; frequently women |
| Risk factors | Heart attack, coronary artery disease, cardiomyopathy | Hypertension, aging, diabetes, obesity, sleep apnea |
| Heart muscle changes | Ventricle dilates and weakens | Ventricle stiffens and often thickens |
| Typical symptoms | More systemic (weakness, reduced perfusion) | More congestion-related (shortness of breath) |
Shared Features and Overlap
Although systolic and diastolic heart failure are classified differently, they share many symptoms and underlying mechanisms. Some people may have forms that involve both impaired contraction and relaxation. Both types frequently lead to right-sided heart failure if untreated.
Recent research suggests that systolic and diastolic heart failure exist on a continuum—not as wholly separate diseases. Some patients exhibit features of both, especially as the disease progresses.
Left-Sided Heart Failure
Both systolic and diastolic heart failure are subtypes of left-sided heart failure. The left ventricle is responsible for pumping oxygen-rich blood to the body. Dysfunction here—whether through weakness (systolic) or stiffness (diastolic)—can eventually strain the right side of the heart, leading to right-sided heart failure and wider complications.
Risk Factors for Each Type
- Systolic heart failure:
- Heart attack or blocked coronary arteries
- Cardiomyopathy from viral infections, alcohol, or drugs
- Genetic predisposition
- Diastolic heart failure:
- High blood pressure (hypertension)
- Aging and stiffening of the heart muscle
- Diabetes mellitus
- Obesity
- Untreated sleep apnea
- Chronic kidney disease
Treatment Options for Systolic and Diastolic Heart Failure
Treatment for both systolic and diastolic heart failure focuses on improving symptoms, slowing disease progression, and reducing hospitalizations. While there is overlap in strategies, some treatments offer more benefit for one type than the other.
Medications
- Diuretics: Reduce fluid overload and swelling for both types
- ACE inhibitors or ARBs: Lower blood pressure and reduce heart strain (particularly effective in systolic heart failure)
- Beta-blockers: Slow the heart rate, helping both types by reducing heart workload
- Aldosterone antagonists: Help regulate salt and water retention, especially useful in systolic heart failure
- SGLT2 inhibitors: Originally developed for diabetes, now shown to benefit both heart failure types in some patients
- Calcium channel blockers: Sometimes used in diastolic heart failure to help heart muscle relaxation
Other Treatments
- Implanted Devices: Pacemakers, defibrillators, or biventricular pacing for certain cases, especially with arrhythmias or advanced systolic failure
- Surgery: Procedures such as coronary artery bypass or valve repair may be needed
- Heart Transplantation: Reserved for severe, refractory cases
Lifestyle Changes
- Eating a low-sodium, heart-healthy diet
- Maintaining physical activity as tolerated
- Managing weight, blood pressure, cholesterol, and blood sugar
- Quitting smoking and minimizing alcohol intake
- Monitoring symptoms and following up closely with healthcare providers
Living with Heart Failure
People with any type of heart failure can lead fulfilling lives with proper treatment and self-management. Early diagnosis, adherence to treatment, and regular monitoring are essential. Collaborative care teams—including physicians, nurses, dietitians, pharmacists, and therapists—play a vital role in optimizing outcomes.
When to Seek Medical Help
- Worsening shortness of breath or inability to perform daily activities
- Significant, sudden weight gain (over 2–3 pounds in a day or 5 pounds in a week)
- Chest pain or fainting
- Increasing swelling in legs or abdomen
- Irregular or very fast heartbeat
Frequently Asked Questions (FAQs)
Q: Whats the main difference between systolic and diastolic heart failure?
A: Systolic heart failure is due to weakened heart muscle contraction (pumping problem, low ejection fraction), while diastolic heart failure is caused by stiffened heart muscle that cannot relax and fill properly (filling problem, normal ejection fraction).
Q: Can heart failure patients have both systolic and diastolic dysfunction?
A: Yes, many patients have mixed presentations, especially as their heart disease progresses, showing features of both impaired contraction and relaxation over time.
Q: Are the symptoms the same for both types?
A: The symptoms often overlap: shortness of breath, fatigue, swelling, and cough are common to both types, making diagnostic imaging essential.
Q: Who is more at risk for diastolic heart failure?
A: Older adults, especially women, and those with high blood pressure, diabetes, obesity, sleep apnea, and chronic kidney disease have an increased risk for diastolic heart failure.
Q: Can lifestyle changes improve heart failure outcomes?
A: Absolutely. A heart-healthy diet, regular exercise, quitting smoking, and managing blood pressure, cholesterol, and diabetes are essential in improving quality of life and limiting heart failure progression.
Takeaway
Understanding the distinctions between systolic and diastolic heart failure helps guide diagnosis and treatment. Both require ongoing management and lifestyle adjustments. If you experience any signs or symptoms of heart failure, seek medical advice promptly. With advances in treatment and care plans tailored to the type of heart failure, most people can lead longer, healthier lives.
References
- https://www.healthline.com/health/heart-failure/systolic-vs-diastolic
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3891535/
- https://www.bannerhealth.com/healthcareblog/teach-me/the-big-differences-between-systolic-and-diastolic-heart-failure
- https://www.heart.org/en/health-topics/heart-failure/what-is-heart-failure/types-of-heart-failure
- https://www.youtube.com/watch?v=gYubeypr-kU
- https://www.medicalnewstoday.com/articles/systolic-vs-diastolic-heart-failure
- https://my.clevelandclinic.org/health/diseases/22950-diastolic-heart-failure
Read full bio of Sneha Tete












