Superior Segmental Optic Nerve Hypoplasia: Symptoms, Diagnosis, and Insights
Explore symptoms, diagnosis, causes, and risk factors of Superior Segmental Optic Nerve Hypoplasia, a rare optic nerve condition linked to maternal diabetes.
Superior Segmental Optic Nerve Hypoplasia: Understanding a Rare Eye Condition
Superior Segmental Optic Nerve Hypoplasia (SSOH) is an uncommon congenital optic nerve disorder, primarily recognized by distinctive changes in the upper segment of the optic disc. Although its symptoms are typically mild or absent, SSOH can sometimes lead to subtle alterations in vision, most frequently in individuals whose mothers had diabetes during pregnancy. Awareness and accurate diagnosis of SSOH are essential for preventing misdiagnosis, particularly confusion with conditions such as glaucoma.
What is Superior Segmental Optic Nerve Hypoplasia?
SSOH is a congenital anomaly affecting the superior segment of the optic nerve head. Its hallmark is the underdevelopment of nerve fibers in the upper part of the optic disc, resulting in localized thinning and potential vision changes. The optic nerve, responsible for transmitting visual information from the retina to the brain, fails to develop normally in affected individuals, yet most experience little to no loss of overall visual function.
- Prevalence: SSOH is rare, with studies estimating an occurrence of less than 1% in the general population.
- Course: The condition is non-progressive and typically remains stable throughout life.
- Alternative Names: SSOH may also be referred to as “topless disc syndrome”.
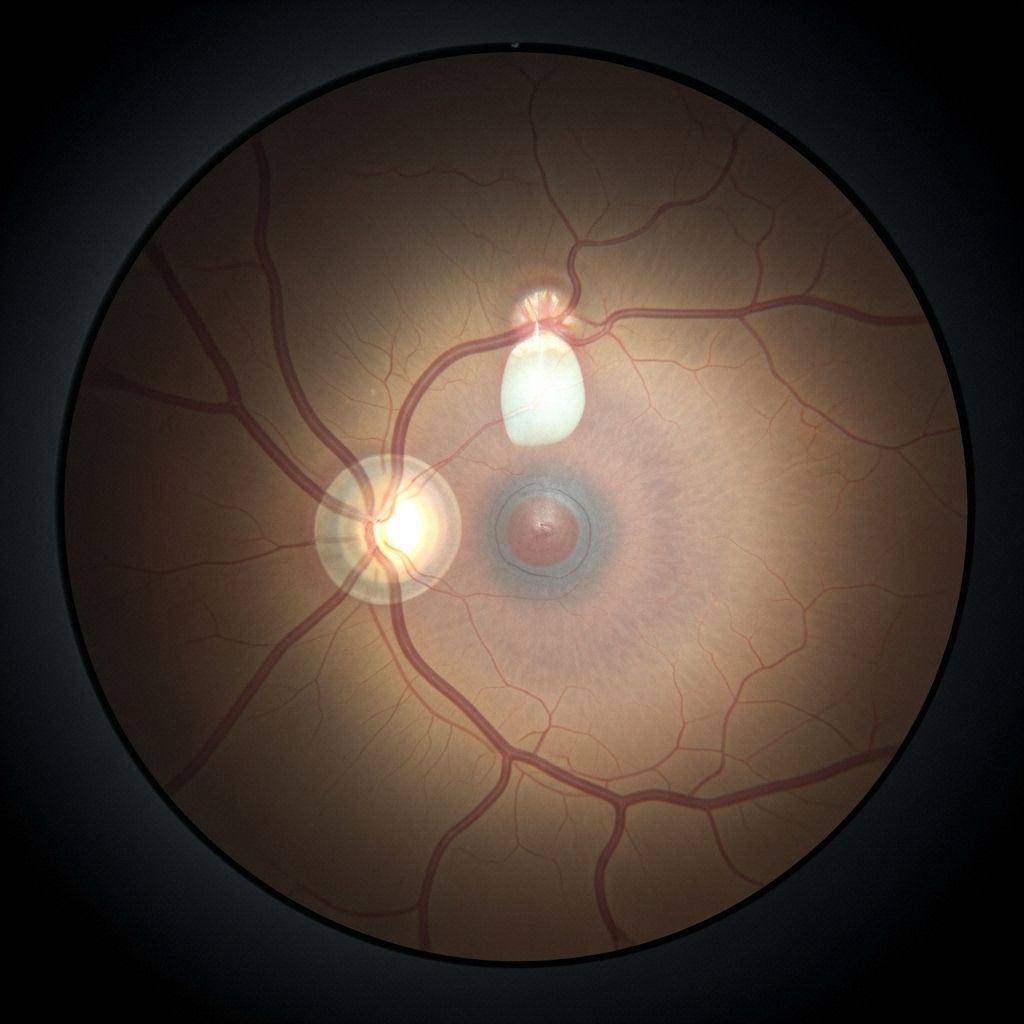
Signs and Diagnostic Features of SSOH
Advanced eye imaging, such as Optical Coherence Tomography (OCT), allows clinicians to distinguish SSOH from other optic nerve disorders, especially glaucoma. Though not all patients show every sign, four classic features define SSOH:
- Superior central retinal artery entrance: The central retinal artery enters the upper part of the optic disc, unlike its typical path.
- Superior disc pallor: Noticeable paleness in the upper part of the optic disc, indicating reduced nerve fibers.
- Superior peripapillary halo: A halo appears around the upper optic disc due to structural changes in surrounding tissue.
- Superior peripapillary nerve fiber thinning: OCT detects thinning of the nerve fibers above the optic disc.
The presence of these signs aids ophthalmologists in making a clear diagnosis, helping distinguish SSOH from other visual field disorders such as glaucoma and other forms of optic nerve hypoplasia.
How SSOH Affects Vision
Most people diagnosed with SSOH report mild or no symptoms. Since the optic nerve transmits signals to the brain, any loss or compromise in nerve fibers can limit the information received from the retina, but SSOH typically spares the majority of vision. The main visual consequence is an impairment of the inferior (bottom) visual field, because development is compromised in the superior optic nerve segment.
- Blurring or blind spots may occur in the lower half of visual field.
- Most daily activities, including reading and navigation, remain unaffected.
- Deficits are usually only noticed during routine visual field testing or if vision is lost in one eye.
- Some individuals may stumble or have subtle difficulties with lower vision, but often do not notice any problems unless specifically tested.
Causes and Risk Factors for SSOH
The exact cause of SSOH remains unclear, though several risk factors have been proposed. The leading risk factor is maternal diabetes, which is strongly associated with an increased likelihood of SSOH in offspring.
| Risk Factor | Details |
|---|---|
| Maternal diabetes | Most common risk factor; mothers diagnosed with diabetes are more likely to have children with SSOH. |
| First trimester bleeding | Associated with vascular disruptions that may affect optic nerve development. |
| Maternal smoking and drug use | Impacts blood flow and fetal development, increasing risk for congenital conditions. |
| Young maternal age | Higher risk group for certain congenital anomalies, including optic nerve hypoplasias. |
| Low maternal weight gain or loss | May contribute to developmental challenges. |
| Preterm labor and first pregnancy | Early developmental challenges can increase risk. |
While genetic mutations have been investigated, their contribution is minor compared to environmental and maternal factors. Some researchers cite *vascular disruption* as a potential cause, referring to temporary interruptions in fetal blood supply that can impair optic nerve development.
Differentiation From Glaucoma and Other Eye Disorders
SSOH is frequently misdiagnosed as glaucoma due to shared features like thinning of nerve fibers and visual field defects. However, there are important distinctions:
| Feature | SSOH | Glaucoma |
|---|---|---|
| Location of nerve fiber thinning | Superior (upper) segment | Inferotemporal segment |
| Course | Non-progressive | Usually progressive |
| Visual field loss | Inferior visual field | Typically arcuate defects or paracentral loss |
| Key imaging features | Superior disc pallor, superior peripapillary halo | Generalized or regional thinning without halo |
Precise diagnosis through imaging and careful clinical assessment prevent unnecessary treatment, such as glaucoma medications, which are not indicated for SSOH.
Symptoms and Associated Conditions
Although SSOH alone rarely causes significant symptoms, the broader category of optic nerve hypoplasia can involve additional health concerns:
- Uncontrollable eye movements (nystagmus), common in generalized optic nerve hypoplasia.
- Misalignment of the eyes (strabismus).
- Potential neurodevelopmental abnormalities in rare cases where hypoplasia is part of a broader syndrome.
- If the hypothalamus is also underdeveloped, associated symptoms can include temperature instability, issues with hunger and thirst regulation, and hormone imbalances such as hypothyroidism or diabetes.
Diagnosis and Evaluation of SSOH
Most cases of SSOH are identified incidentally during routine eye exams. The evaluation typically includes:
- Direct Fundoscopy: Allows visualization of the optic nerve and detection of pallor or structural abnormalities.
- Optical Coherence Tomography (OCT): Provides cross-sectional imaging of the retinal nerve fiber layer, revealing thinning and other structural signs.
- Visual Field Testing: Assesses function, identifying any deficits in the inferior field that correlate with SSOH.
- Family and Maternal History: Asking about maternal diabetes or other risk factors can aid in diagnosis.
A critical aspect is distinguishing SSOH from progressive optic nerve diseases. Unlike glaucoma, SSOH does not progress, and the prognosis for vision is generally excellent.
Management and Prognosis
There is no specific treatment for SSOH, as the condition is stable and rarely impairs overall vision. Instead, the focus is on correct diagnosis and ongoing monitoring. Patients should have regular eye exams but require no intervention unless other, unrelated eye conditions are found.
- Most individuals live normal lives without limitations.
- Vision typically remains stable.
- Patient education is vital to avoid anxiety and unnecessary treatments often prescribed for misdiagnosed glaucoma.
Frequently Asked Questions (FAQs)
Q: Is Superior Segmental Optic Nerve Hypoplasia inherited?
A: SSOH is not typically inherited. Its strongest known association is with maternal diabetes during pregnancy rather than with genetic mutations.
Q: Can SSOH worsen over time?
A: No, SSOH is a congenital, non-progressive condition. Most people have stable vision throughout their lives.
Q: How can SSOH be distinguished from glaucoma?
A: SSOH displays structural and functional changes mainly in the superior part of the optic disc, with corresponding inferior field defects and specific imaging features such as superior disc pallor and peripapillary halo. Glaucoma typically affects the inferotemporal region and is progressive in nature.
Q: What should I do if I’ve been diagnosed with SSOH?
A: No treatment is necessary unless other eye conditions are present. Continue with routine eye exams and consult your ophthalmologist if there are any changes in your vision.
Q: Are children with mothers who have diabetes at higher risk?
A: Yes, maternal diabetes is a significant risk factor that raises the likelihood of SSOH.
When to Consult an Eye Doctor
- Noticeable vision changes or field loss, especially if you have risk factors such as family history or maternal diabetes.
- Unexplained stumbling, tripping, or difficulty seeing objects in the lower visual field.
- Routine eye exams are key for early detection of all optic nerve conditions.
Summary Table: Key Points about SSOH
| Aspect | Details |
|---|---|
| Definition | Congenital defect resulting in underdevelopment of upper optic nerve fibers |
| Prevalence | Very rare (<1%) |
| Symptoms | Mild or none; inferior visual field defect possible |
| Risk Factors | Maternal diabetes, vascular disruptions |
| Diagnosis | Fundoscopy, OCT, clinical history |
| Course | Non-progressive, stable vision |
| Treatment | No treatment required; regular follow-up |
Superior Segmental Optic Nerve Hypoplasia is a rare, generally mild optic nerve condition, most often associated with maternal diabetes. Accurate diagnosis relies on advanced imaging and clinical awareness, ensuring effective management while preventing unnecessary interventions. Early recognition by eye care professionals is critical to distinguish SSOH from more serious pathologies such as glaucoma, reinforcing the importance of routine comprehensive eye examinations.
References
- https://www.healthline.com/health/eye-health/superior-segmental-optic-nerve-hypoplasia
- https://pubmed.ncbi.nlm.nih.gov/35189184/
- https://journal.opted.org/article/superior-segmental-optic-nerve-hypoplasia-a-teaching-case-report/
- https://www.webmd.com/eye-health/what-is-optic-nerve-hypoplasia
- https://eyewiki.org/Superior_Segmental_Optic_Nerve_Hypoplasia_(SSONH)
- https://my.clevelandclinic.org/health/diseases/optic-nerve-hypoplasia-includes-septo-optic-dysplasia
- https://rarediseases.org/rare-diseases/optic-nerve-hypoplasia/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3576022/
Read full bio of medha deb












