Superior Canal Dehiscence Syndrome: Causes, Symptoms, Diagnosis & Treatment
A comprehensive guide to understanding superior canal dehiscence syndrome (SCDS)—its causes, symptoms, diagnostics, and treatment options for better patient care.
Superior Canal Dehiscence Syndrome (SCDS): An Overview
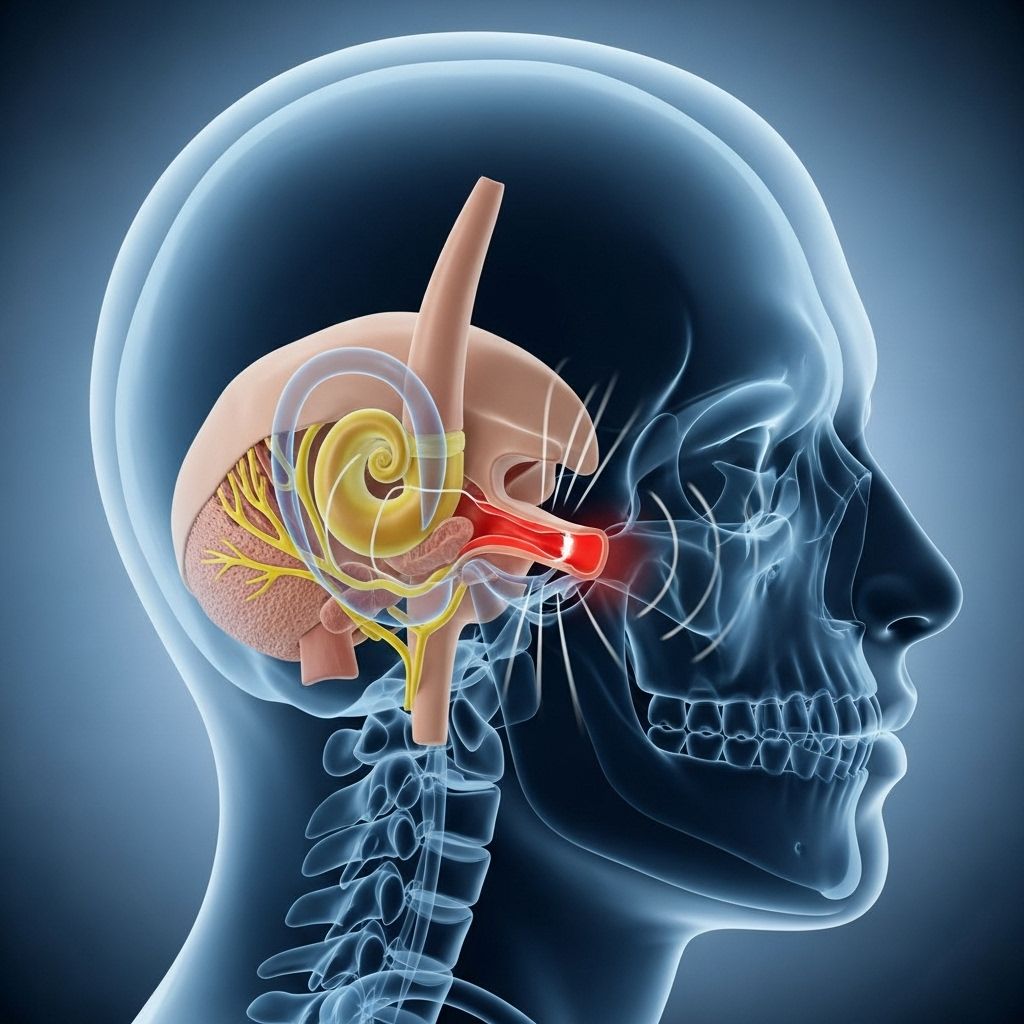
Superior Canal Dehiscence Syndrome (SCDS) is a rare inner ear disorder marked by unusual connections or openings in the bony part of the superior semicircular canal in the vestibular system of the inner ear. This abnormality disrupts the way sound and pressure waves are transmitted, leading to a variety of distinct hearing and balance symptoms. Though SCDS is uncommon, it can significantly affect the quality of life for those who experience it.
What is Superior Canal Dehiscence Syndrome?
The superior semicircular canal is one of three semicircular canals in the vestibular labyrinth, responsible for maintaining balance. SCDS occurs when the thin bone overlying this canal is either missing or thinned, resulting in an opening (dehiscence) that allows abnormal communications between the canal and the brain or cranial cavity. This ‘third window’ effect causes disturbances in the normal flow of fluid and pressure within the inner ear, producing a set of characteristic symptoms.
Causes of Superior Canal Dehiscence Syndrome
While SCDS can occur in anyone, certain risk factors and potential causes have been identified:
- Congenital bone thinning: Some individuals are born with thinner than normal temporal bone over the superior semicircular canal, making them susceptible to dehiscence as they age or when exposed to physical stress.
- Genetic predisposition: Family history may increase risk due to inherited structural vulnerabilities.
- Aging: Progressive thinning of the temporal bone with age can make the bone more susceptible to forming an opening.
- Minor head trauma: Accidents or injuries may fracture or thin the bone, leading to dehiscence.
- Pressure-altering events: Activities such as weight lifting, excessive straining, scuba diving, or flying, where frequent changes in pressure occur, can contribute to bone weakness or cause a pre-existing thin area to open.
- Tumors: Benign or malignant growths may erode the bone overlying the canal.
Who Gets Superior Canal Dehiscence Syndrome?
SCDS is rare, affecting fewer than 2% of the general population. Men and women appear to be affected equally, with the average age at diagnosis around 45 years old. The condition may develop at any age but is most often identified when symptoms become bothersome enough to prompt evaluation. Some individuals with dehiscence remain asymptomatic for years or may never develop noticeable symptoms.
Symptoms of Superior Canal Dehiscence Syndrome
SCDS produces a range of vestibular (balance-related) and auditory (hearing-related) symptoms, which can sometimes be misattributed to other inner ear disorders. The symptoms can be variable and may be triggered by changes in pressure, movement, or even loud sounds.
- Autophony: An uncomfortably loud or distorted perception of one’s own voice, breathing, heartbeat, or even eye movement. Some individuals may hear body noises such as chewing, swallowing, or footstep sounds from within.
- Hearing Loss: Usually affecting low frequencies, this may mimic other middle ear conditions such as otosclerosis. SCDS makes patients more sensitive to bone-conducted sounds.
- Vertigo and Dizziness: Sensations of spinning, lightheadedness, or disequilibrium, especially triggered by loud noises (Tullio phenomenon), pressure changes, coughing, sneezing, or straining.
- Oscillopsia: The illusion that the environment or objects around are bouncing or moving, particularly when the head is in motion or exposed to certain sounds.
- Pulsatile Tinnitus: Hearing a rhythmic ‘whooshing’ or pulsing sound in sync with one’s own heartbeat.
- Aural Fullness: A constant feeling of pressure or fullness in the ear.
- Hyperacusis: A heightened sensitivity to sounds, causing noises to seem abnormally loud.
- Nystagmus: Repetitive, involuntary eye movements typically triggered by sound or pressure changes.
- Headaches and Migraines: Some people experience increased headaches, possibly due to muscular tension from compensating for hearing loss or inner ear disturbances.
- Fatigue and Brain Fog: Persistent tiredness and difficulty concentrating may arise as the brain works extra hard to interpret conflicting sensory information from a malfunctioning inner ear.
Triggers of SCDS Symptoms
- Loud sounds (Tullio phenomenon)
- Changes in middle ear or intracranial pressure (coughing, sneezing, straining, heavy lifting)
- Rapid changes in barometric pressure (air travel, scuba diving)
Complications and Related Issues
If left untreated, SCDS symptoms can interfere with daily life—driving, walking, working, and communicating may become challenging. In some cases, SCDS may trigger or worsen vestibular migraines, headaches characterized by dizziness and heightened sensitivity to light, sound, or movement. It is crucial to accurately distinguish between SCDS and vestibular migraine, as their management strategies differ.
Diagnosing Superior Canal Dehiscence Syndrome
Diagnosis of SCDS requires a combination of careful clinical assessment, history taking, and the use of advanced imaging and inner ear function tests. Because SCDS symptoms often overlap with other ear disorders, accurate diagnosis is essential to guide effective treatment.
Diagnostic Process
- Clinical Evaluation: The clinician reviews the patient’s medical history and notes detailed descriptions of symptoms—especially triggers, duration, and impact on daily life.
- Physical Examination: Ear and neurological exams help to rule out other causes of hearing loss or vertigo.
- Specialized Tests:
- High-resolution CT scan: Specific scans of the temporal bone provide clear images to detect thinning or absence of the bone over the superior semicircular canal.
- Vestibular Evoked Myogenic Potential (VEMP) Test: Measures how sound and vibrations affect balance organs, helping to detect abnormal conductance pathways in the canal.
- Hearing (Audiometry) Evaluation: Determines the pattern and extent of hearing loss, helping distinguish SCDS from other middle ear diseases.
Other diagnostic tools may include balance testing (videonystagmography) and specialized pressure tests to measure how changes in ear pressure or sound induce symptoms.
Treatment Options for Superior Canal Dehiscence Syndrome
The treatment plan for SCDS is individualized, depending on the severity of symptoms and their impact on the patient’s quality of life. Not all cases require surgery; milder symptoms may be managed through conservative strategies.
Conservative Management
- Observation: If symptoms are minimal or infrequent, careful monitoring and avoidance of symptom triggers may be sufficient.
- Activity Modification: Patients are often advised to avoid activities that significantly alter pressure in the ear, such as heavy lifting, forceful nose-blowing, straining, or extreme altitude changes.
- Sound Protection: Use of ear protection (earplugs) in noisy environments can reduce symptoms triggered by loud sounds.
- Vestibular Rehabilitation: Physical therapy and balance exercises may help some individuals minimize dizziness and improve adaptive responses.
Surgical Interventions
For those with severe or persistent symptoms adversely impacting daily life, surgery to repair the defect may be considered. The main surgical approaches are:
- Canal Resurfacing: A surgical procedure in which the defective portion of the bone is covered with a bone graft or other suitable material to restore the barrier between the canal and the cranial cavity.
- Canal Plugging: Filling the affected semicircular canal with a soft tissue or bone plug to stop the abnormal passage of sound and pressure waves. This reduces symptoms but may slightly reduce overall vestibular function on the operated side.
Most surgical interventions are performed through either a middle cranial fossa approach or a transmastoid approach. Each technique has specific advantages and is chosen based on the patient’s unique anatomy and surgeon’s expertise.
Risks and Recovery
- As with any surgery involving the brain and inner ear, risks include infection, hearing loss, vertigo, cerebrospinal fluid leak, or facial nerve injury. Most patients, however, experience significant relief of symptoms with proper surgical care and rehabilitation.
- Recovery time varies but usually involves several weeks of activity restrictions and follow-up.
Frequently Asked Questions (FAQs)
Q: How common is superior canal dehiscence syndrome?
A: SCDS is rare, affecting less than 2% of the population. Many people with anatomical dehiscence remain asymptomatic.
Q: What is the prognosis for someone with SCDS?
A: Most individuals with mild symptoms manage well with observation and lifestyle adjustments. Those who undergo surgery usually experience significant improvement in hearing and balance, with low rates of recurrence.
Q: Can SCDS be confused with other inner ear disorders?
A: Yes. Symptoms often mimic conditions like Meniere’s disease, vestibular migraines, and otosclerosis. Accurate diagnosis by an ear specialist is crucial.
Q: Is SCDS hereditary?
A: There is some evidence of familial clustering, suggesting that genetics and inherited bone structure may play a role, but no definitive genetic link has been established.
Q: What should I do if I suspect I have SCDS?
A: Seek evaluation from an otolaryngologist (ENT specialist) familiar with balance and hearing disorders. Early diagnosis and management can prevent the progression of symptoms and improve quality of life.
Tips and Outlook
- While SCDS cannot always be prevented, avoiding head trauma, controlling activities that rapidly change pressure, and maintaining overall ear health can help reduce risk and manage symptoms.
- Awareness of symptom triggers and early consultation with a specialist can lead to timely diagnosis and effective management.
- Support groups and patient education can be valuable resources for those living with chronic symptoms.
Summary Table: Key Points of SCDS
| Feature | Description |
|---|---|
| What is SCDS? | A defect (opening/thinning) in the bone over the superior semicircular canal causing abnormal hearing and balance symptoms. |
| Main Symptoms | Autophony, vertigo, oscillopsia, hearing loss, aural fullness, pulsatile tinnitus, hyperacusis |
| Triggers | Loud noises, straining, pressure changes, trauma |
| Diagnosis | Clinical history, physical exam, high-resolution CT scan, VEMP test, hearing evaluation |
| Treatments | Observation, activity modification, vestibular rehab, surgery (resurfacing or plugging) |
| Prognosis | Most patients see improvement; surgical treatment has high success but carries typical surgical risks. |
Resources and Support
- Consult with a neurotologist or otolaryngologist experienced in diagnosing and treating SCDS for the most up-to-date care options.
- Join patient advocacy and educational organizations for additional support and the latest research updates.
- Mental health professionals can help those experiencing anxiety or life disruptions due to persistent symptoms.
References
- https://www.dukehealth.org/treatments/ear-nose-and-throat/superior-canal-dehiscence-syndrome
- https://www.pennmedicine.org/conditions/superior-semicircular-canal-dehiscence
- https://en.wikipedia.org/wiki/Superior_canal_dehiscence_syndrome
- https://www.menieres.org.uk/information-and-support/symptoms-and-conditions/superior-canal-dehiscence-syndrome
- https://www.templehealth.org/services/conditions/superior-canal-dehiscence-syndrome
- https://my.clevelandclinic.org/health/diseases/15266-superior-canal-dehiscence-syndrome
- https://rarediseases.org/rare-diseases/superior-semicircular-canal-dehiscence/
- https://www.webmd.com/brain/canal-dehiscence-syndrome
- https://www.youtube.com/watch?v=5QnWfLNUpKk
Read full bio of medha deb












