Stress and Anxiety: Their Impact on IBS and How to Find Relief
Learn how stress and anxiety influence IBS symptoms, and discover practical ways to manage both mind and gut health together.
Stress and Anxiety: Their Impact on Irritable Bowel Syndrome (IBS)
Irritable bowel syndrome (IBS) is a complex digestive disorder characterized by symptoms such as abdominal pain, cramping, bloating, diarrhea, and constipation. While its exact cause remains elusive, research has firmly established that both stress and anxiety play a significant role in the development, persistence, and severity of IBS symptoms. This article delves into the intricate relationship between mental health and IBS, explains the underlying biological mechanisms, and offers practical strategies for relief.
Understanding the Connection: Stress, Anxiety, and IBS
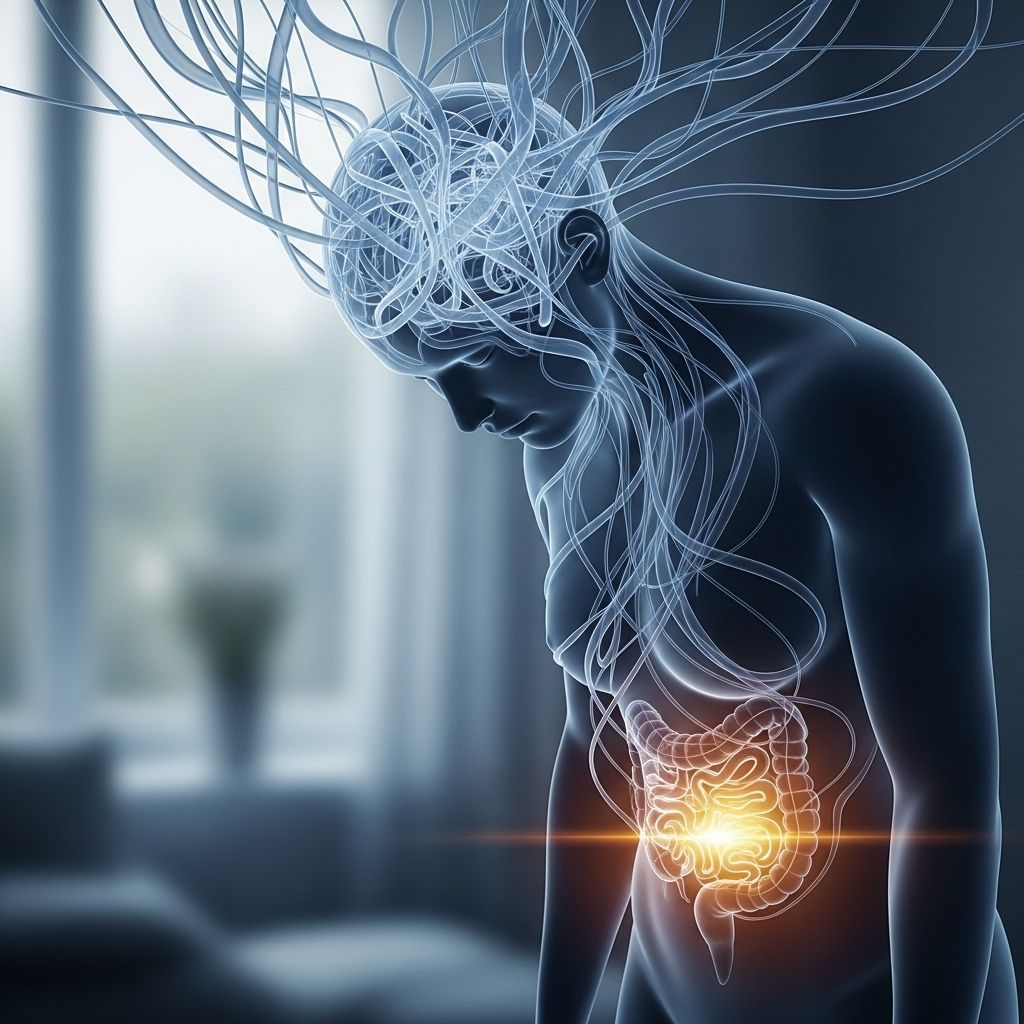
Experts have long recognized the profound interaction between the mind and the gastrointestinal system. The relationship is so striking that it’s now common to refer to the gut-brain axis, emphasizing the ongoing two-way communication between the digestive tract and the brain.
- Psychological stress can independently produce IBS-like symptoms, even in the absence of physical illness.
- People with IBS often report higher rates of anxiety and depression compared to the general population.
- Chronic stress is known to exacerbate IBS flare-ups and contribute to the overall severity of symptoms.
The Gut-Brain Axis: What Is It?
The gut-brain axis refers to the complex interplay of hormones, nerves, and immune signals that connect your gut and brain bidirectionally. This pathway means that emotional states like stress and anxiety can directly impact your digestion, and vice versa.
- Nerves: The central and enteric nervous systems communicate signals about pain, motility, and secretions.
- Hormones: Chemicals such as cortisol and adrenaline, produced in response to stress, alter gut function.
- Immune factors: Immune responses in the gut can influence and be influenced by stress hormones and brain activity.
A growing body of research underscores that IBS is not merely a gut disorder, but a combination of irritable bowel and irritable brain.
How Stress Affects the Digestive System
When you’re exposed to significant or chronic stress, several changes take place in your body, some of which can aggravate IBS symptoms:
- Increased gut sensitivity: Stress heightens awareness of pain and discomfort, making gut sensations more pronounced.
- Altered motility: Nerves that control digestive movements become overactive, sometimes leading to diarrhea, or underactive, resulting in constipation.
- Changes in secretion: Stress can affect the production of digestive juices and mucus, potentially leading to changes in stool consistency and frequency.
- Reduced blood flow: During stressful periods, blood flow diverts away from the intestines, which may contribute to pain and altered bowel habits.
- Disturbed gut microbiota: Chronic stress can lead to dysbiosis—an imbalance in the intestinal bacteria—further worsening IBS symptoms.
The Psychological Toll: Anxiety, Depression, and IBS
IBS often exists alongside psychological conditions like anxiety and depression. The connection is so robust that doctors now recommend screening for mental health issues in anyone with IBS.
| Condition | Rate in IBS Population | Rate in General Population |
|---|---|---|
| Anxiety | 38% | ~19% |
| Depression | 27% | ~13% |
This higher prevalence of mood disorders in people with IBS reinforces the notion that treating both physical and mental symptoms is essential for recovery.
IBS and Mental Health: Cause or Effect?
The direction of the relationship is complex and appears to be bidirectional:
- Anxiety and depression can contribute to developing and worsening IBS.
- IBS symptoms themselves often lead to increased anxiety and low mood, due to the unpredictable and disruptive nature of the disorder.
Impact Beyond the Gut
IBS affects quality of life, work productivity, social activity, and can even lead to conditions such as insomnia, eating disorders, and increased risk of suicidal thoughts. Understanding the complex web of effects underscores the need for a holistic approach to treatment.
Types of IBS and Their Relationship to Anxiety
IBS is classified by the predominant symptom type:
- IBS-D: IBS with diarrhea as the main symptom.
- IBS-C: IBS with constipation as the main symptom.
- IBS-M: Mixed type, with both diarrhea and constipation.
- IBS-U: Unclassified.
While individuals with any IBS subtype are likely to experience higher than average levels of anxiety, research indicates that the prevalence of anxiety does not significantly differ between subtypes—all are impacted when compared to people without IBS.
Why Does Stress Worsen IBS?
Here are the primary mechanisms by which stress, anxiety, and related factors worsen IBS:
- Activation of the Sympathetic Nervous System: Heightened stress responses lead to overactivity of the nerves supplying the gut.
- Hormonal changes: Stress triggers the release of hormones such as cortisol and adrenaline, which can disrupt digestion and contribute to symptoms like pain, bloating, and altered bowel habits.
- Increased gut permeability: Acute and chronic stress both enhance gut permeability, making the digestive tract more sensitive to foods and bacteria.
- Microbiota disruption: Stress-induced changes to the gut microbiome may fuel ongoing inflammation and symptom escalation.
- Mucosal immune activation: Stress alters immune signaling in the digestive tract, possibly intensifying gut pain or sensitivity.
Recognizing and Managing IBS Triggers
Identifying specific triggers for IBS may help in creating a tailored treatment plan. Common triggers include:
- Psychological stress
- Anxiety or major life changes
- Dietary components (spicy foods, caffeine, artificial sweeteners)
- Illness or infection
- Hormonal fluctuations (including menstrual cycle changes)
Because psychological factors can intensify the impact of other triggers, addressing stress management can be a cornerstone of IBS care.
Approaches to Managing Stress and Anxiety in IBS
Given the strong influence of psychological factors, an integrative, holistic approach to care is often most effective. Treatment strategies may include:
1. Lifestyle Modifications
- Regular exercise: Lowers stress hormones and can improve bowel function.
- Balanced diet: Eat regular, fiber-rich meals and avoid known dietary triggers.
- Adequate sleep: Good rest bolsters the brain-gut axis and supports emotional health.
- Limiting caffeine and alcohol: Minimizing these can reduce stomach irritation.
2. Stress Management Techniques
- Cognitive behavioral therapy (CBT): Proven to help reduce IBS symptoms by changing thought patterns related to stress and pain.
- Mindfulness-based stress reduction (MBSR): Practices such as meditation, yoga, and deep breathing promote relaxation.
- Biofeedback: Helps patients recognize and manage physical responses to stress.
3. Medical and Pharmacological Options
- Antidepressants and antianxiety medications: Sometimes prescribed for persistent symptoms when therapy alone is insufficient.
- Targeted gut medications: Depending on symptoms, options include antispasmodics, laxatives, or anti-diarrheal medications.
- Probiotics: May help restore healthy gut bacteria and reduce IBS symptoms, especially when dysbiosis is present.
4. Social and Emotional Support
- Connect with support groups or mental health professionals.
- Awareness of IBS and its impact can reduce stigma and foster understanding among family, friends, and employers.
When to See a Doctor
If you suspect IBS or find your symptoms worsening due to stress or anxiety, consult a healthcare professional. Early intervention not only helps manage digestive symptoms, but also addresses underlying mental health concerns. Key warning signs warranting medical attention include:
- Unintentional weight loss
- Rectal bleeding
- Persistent or severe abdominal pain
- Nighttime diarrhea
- Family history of GI disorders or cancer
Frequently Asked Questions (FAQs)
Q: How does anxiety physically affect my gut?
A: Anxiety triggers the sympathetic nervous system, releasing hormones like cortisol and adrenaline, which increase gut motility, sensitivity, and alter digestive secretions—leading to symptoms like pain, diarrhea, or constipation.
Q: Can treating mental health improve IBS symptoms?
A: Yes. Evidence shows that addressing anxiety and depression through therapy, medications, or lifestyle changes can significantly reduce IBS severity and improve quality of life.
Q: Are some types of IBS linked to higher anxiety?
A: While all IBS subtypes show elevated anxiety compared to the general population, studies do not find substantial differences in anxiety rates between IBS subtypes (IBS-D, IBS-C, IBS-M).
Q: What lifestyle changes can help manage IBS symptoms worsened by stress?
A: Regular exercise, a balanced diet, sleep hygiene, and practicing relaxation techniques can all lower stress levels and support gut health.
Q: Should I consider therapy for IBS?
A: Behavioral therapies such as cognitive behavioral therapy can be highly effective, helping manage both mental health challenges and IBS symptoms together.
Key Takeaways
- Stress and anxiety are deeply intertwined with IBS, both as causes and consequences.
- The gut-brain axis explains how mental health directly influences digestive function.
- Managing IBS often requires an integrated approach addressing both physical and psychological aspects.
- Therapy, medication, and lifestyle changes can each play a role in relief.
- Seeking support from healthcare professionals and support groups can make a significant difference.
References
- https://www.healthline.com/health-news/irritable-bowel-syndrome-how-psychological-stress-contributes-to-ibs-symptoms
- https://www.gastroenterologyadvisor.com/news/explaining-how-anxiety-affects-ibs-to-patients/
- https://medicine.missouri.edu/news/irritable-bowel-syndrome-patients-suffer-high-rates-anxiety-and-depression
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4202343/
- https://www.healthline.com/health/video/hidden-connection-between-stress-and-your-gut
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10237074/
- https://my.clevelandclinic.org/health/diseases/4342-irritable-bowel-syndrome-ibs
- https://www.goodrx.com/conditions/irritable-bowel-syndrome/anxiety-ibs-irritable-bowel-syndrome-how-are-they-related
Read full bio of medha deb












