Stomach and Duodenal Ulcers (Peptic Ulcers): Causes, Symptoms, and Treatment
Understand the causes, symptoms, complications, diagnosis, and effective treatments for stomach and duodenal (peptic) ulcers.
Stomach and Duodenal Ulcers (Peptic Ulcers)
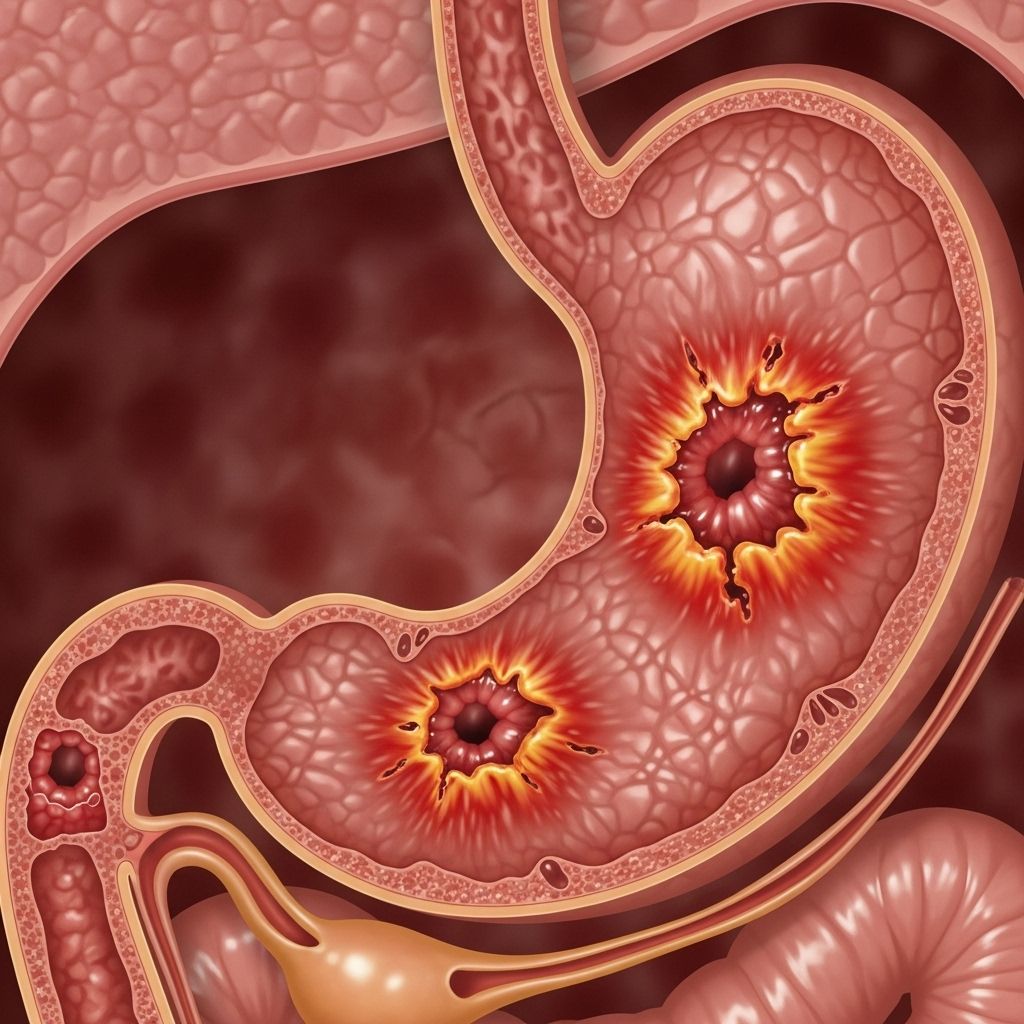
Peptic ulcers are open sores that develop on the inner lining of the stomach (known as gastric ulcers) or in the upper part of the small intestine called the duodenum (duodenal ulcers). These conditions can cause significant discomfort and, if left untreated, may lead to serious complications. This comprehensive guide explores the causes, symptoms, diagnosis, treatment options, potential complications, and prevention strategies related to stomach and duodenal ulcers.
What Are Stomach and Duodenal Ulcers?
A peptic ulcer refers to an open sore in the lining of the stomach or duodenum. When the ulcer occurs in the stomach, it is called a gastric ulcer; if it occurs in the duodenum, it is a duodenal ulcer. Both types can cause abdominal pain and digestive disturbances, with duodenal ulcers being more common than gastric ulcers.
- Gastric ulcer: Located in the stomach lining
- Duodenal ulcer: Located in the first part of the small intestine (duodenum)
How Common Are Peptic Ulcers?
Peptic ulcers are a frequent condition worldwide, and millions of new cases are diagnosed annually. While anyone can develop an ulcer, some risk factors, such as certain infections and medication use, increase the likelihood.
Causes of Stomach and Duodenal Ulcers
The most common causes of peptic ulcers include:
- Helicobacter pylori (H. pylori) infection: This bacterium infects the lining of the stomach and duodenum, weakening the protective mucus layer and making it susceptible to damage from stomach acid.
H. pylori is estimated to be responsible for the majority of peptic ulcers worldwide. - Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Regular use of medications like ibuprofen, aspirin, and naproxen can erode the stomach’s protective lining, increasing the risk of ulcers.
Other risk factors and contributors include:
- Frequent smoking
- Excessive alcohol consumption
- High levels of stress (may not directly cause ulcers but can exacerbate symptoms)
- Family history of ulcers
Very rarely, cancers of the stomach or duodenum, or certain rare conditions like Zollinger-Ellison syndrome, can also cause peptic ulcers.
Symptoms of Peptic Ulcers
Symptoms of stomach and duodenal ulcers can range from mild discomfort to severe pain. Some individuals may remain asymptomatic, making regular medical check-ups essential if risk factors are present.
- Burning pain in the abdomen, often between meals or during the night; may be relieved by eating or antacids
- Bloating and feeling of fullness
- Frequent belching
- Heartburn or reflux
- Nausea or vomiting
- Unexplained weight loss
- Loss of appetite
Some symptoms call for immediate medical attention:
- Sharp or sudden severe abdominal pain
- Vomiting blood or material that looks like coffee grounds
- Black, tarry stools (a sign of bleeding)
Diagnosis of Stomach and Duodenal Ulcers
Diagnosis typically involves a combination of medical history, physical examination, and specific diagnostic tests:
- Upper Endoscopy (EGD): A flexible tube with a camera (endoscope) is inserted through the mouth to visually examine the stomach and duodenum. Tissue samples (biopsies) can be taken to check for H. pylori infection or rule out cancer.
- H. pylori Testing: Several tests are available, such as:
- Breath test
- Blood test
- Stool antigen test
- Biopsy during endoscopy
- Imaging Tests: In some cases, an upper gastrointestinal series (X-rays) may be ordered.
Complications of Peptic Ulcers
Without appropriate treatment, peptic ulcers can lead to serious, sometimes life-threatening, complications:
- Bleeding: Ulcers can erode blood vessels, causing slow oozing or massive hemorrhage. Signs include vomiting blood or black, tarry stools.
- Perforation: The ulcer can create a hole in the stomach or duodenal wall, leading to leakage of stomach contents and severe infection (peritonitis). This is a medical emergency.
- Obstruction: Swelling or scarring from an ulcer may block the passage of food, causing vomiting and weight loss.
- Peritonitis and Sepsis: Severe infections resulting from perforation that can spread rapidly and become life-threatening if untreated.
| Complication | Description and Signs |
|---|---|
| Bleeding Ulcer | Vomiting blood, black or tarry stools, weakness, shock in severe cases |
| Perforation | Sudden, severe abdominal pain; peritonitis; requires emergency surgery |
| Obstruction | Vomiting, persistent fullness, inability to keep food down |
Treatment Options for Stomach and Duodenal Ulcers
The goals of treatment include relieving pain, healing the ulcer, preventing complications, and reducing the risk of recurrence. Treatment plans vary depending on the underlying cause and any complications present.
Medications
- Proton Pump Inhibitors (PPIs): Reduce stomach acid production to promote healing (e.g., omeprazole, pantoprazole).
- H2-Receptor Blockers: Alternative acid-suppressing drugs (e.g., ranitidine, famotidine).
- Antibiotics: Required if H. pylori infection is detected. Combination therapy with two antibiotics and a PPI is standard (triple therapy).
- Antacids: Over-the-counter medicines that neutralize stomach acid, providing quick symptomatic relief.
- Protective agents: Medications like sucralfate can coat the ulcer, shielding it from acid during healing.
Lifestyle Changes
- Stop using NSAIDs whenever possible and only use them under medical supervision
- Reduce or eliminate tobacco and alcohol use
- Adopt a balanced diet and avoid foods that trigger symptoms (spicy, fatty, acidic foods, caffeine)
- Eat smaller, more frequent meals instead of large meals
- Manage stress with techniques like meditation, counseling, or physical activity
- Maintain a healthy weight
If the ulcer is associated with medicine use, switching to alternative pain relief strategies may be necessary in consultation with a healthcare provider.
Surgical and Endoscopic Interventions
Surgery is rarely needed today, thanks to effective medications. However, surgery or endoscopic management may be necessary for complications such as massive bleeding, perforation, or obstruction.
Prevention of Peptic Ulcers
While not all ulcers can be prevented, healthy habits can significantly reduce your risk:
- Practice good handwashing and food hygiene to avoid H. pylori infection
- Avoid the unnecessary use of NSAID medications
- Do not smoke
- Drink alcohol only in moderation or not at all
- Seek prompt treatment for conditions causing chronic inflammation
Living with Peptic Ulcers
With proper treatment, most people with peptic ulcers can expect excellent outcomes. It is vital to:
- Take all medications as prescribed
- Attend follow-up appointments and repeat testing if advised
- Adopt healthy lifestyle practices to support healing and prevent recurrence
- Contact your doctor if you develop new or severe symptoms
Frequently Asked Questions (FAQs)
Q: What is the difference between a stomach (gastric) ulcer and a duodenal ulcer?
A: A gastric ulcer forms in the stomach lining, while a duodenal ulcer occurs in the duodenum—the first section of the small intestine. Both are types of peptic ulcers, with similar causes and symptoms but may differ slightly in presentation.
Q: How do I know if I have an ulcer or just indigestion?
A: Both ulcers and indigestion can cause upper abdominal discomfort, but ulcer-related pain is often a persistent burning or gnawing pain, sometimes accompanied by nausea or vomiting. Only diagnostic tests can confirm the presence of an ulcer, so persistent or severe symptoms should be evaluated by a healthcare provider.
Q: Do foods cause ulcers?
A: Foods themselves do not cause ulcers. However, certain foods and beverages (like spicy foods, coffee, or alcohol) may trigger or worsen symptoms if you already have an ulcer or sensitive stomach lining.
Q: Are ulcers curable?
A: Yes, most ulcers heal completely with appropriate treatment, which includes medications to reduce stomach acid and antibiotics if H. pylori infection is present. Recurrence is possible if risk factors are not managed.
Q: When should I seek emergency care?
A: Seek immediate medical attention if you experience severe, sudden abdominal pain, vomiting blood, black or tarry stools, or symptoms of shock (fainting, rapid heartbeat). These may signal a bleeding or perforated ulcer, which is a medical emergency.
Resources
- Consult your healthcare provider for personal medical guidance
- National Institutes of Health – Peptic Ulcer Disease Information
- American College of Gastroenterology – Patient Resources
References
- https://www.gastromedclinic.com/duodenal-ulcers-causes-symptoms-and-treatment-strategies/
- https://www.healthdirect.gov.au/duodenal-ulcer
- https://my.clevelandclinic.org/health/diseases/22314-stomach-ulcer
- https://www.niddk.nih.gov/health-information/digestive-diseases/peptic-ulcers-stomach-ulcers/symptoms-causes
- https://www.nhs.uk/conditions/stomach-ulcer/
- https://www.mayoclinic.org/diseases-conditions/peptic-ulcer/diagnosis-treatment/drc-20354229
- https://www.childrenshospital.org/conditions/stomach-and-duodenal-ulcers
- https://www.mayoclinic.org/diseases-conditions/peptic-ulcer/symptoms-causes/syc-20354223
Read full bio of medha deb












