Stents and Blood Clots: What You Need to Know
Understand the risks, symptoms, and prevention of blood clots after heart stent procedures for better recovery.
Stent placement is a key treatment for coronary artery disease, helping restore blood flow to heart tissue. While many people undergo this common procedure safely every year, placing a stent inside an artery can sometimes increase the risk of developing blood clots within the stent, causing serious complications like heart attack if not properly managed. This comprehensive guide explains how stents work, why blood clots sometimes form, the warning signs to watch for, and practical steps to keep your heart healthy after stent placement.
What Is a Stent?
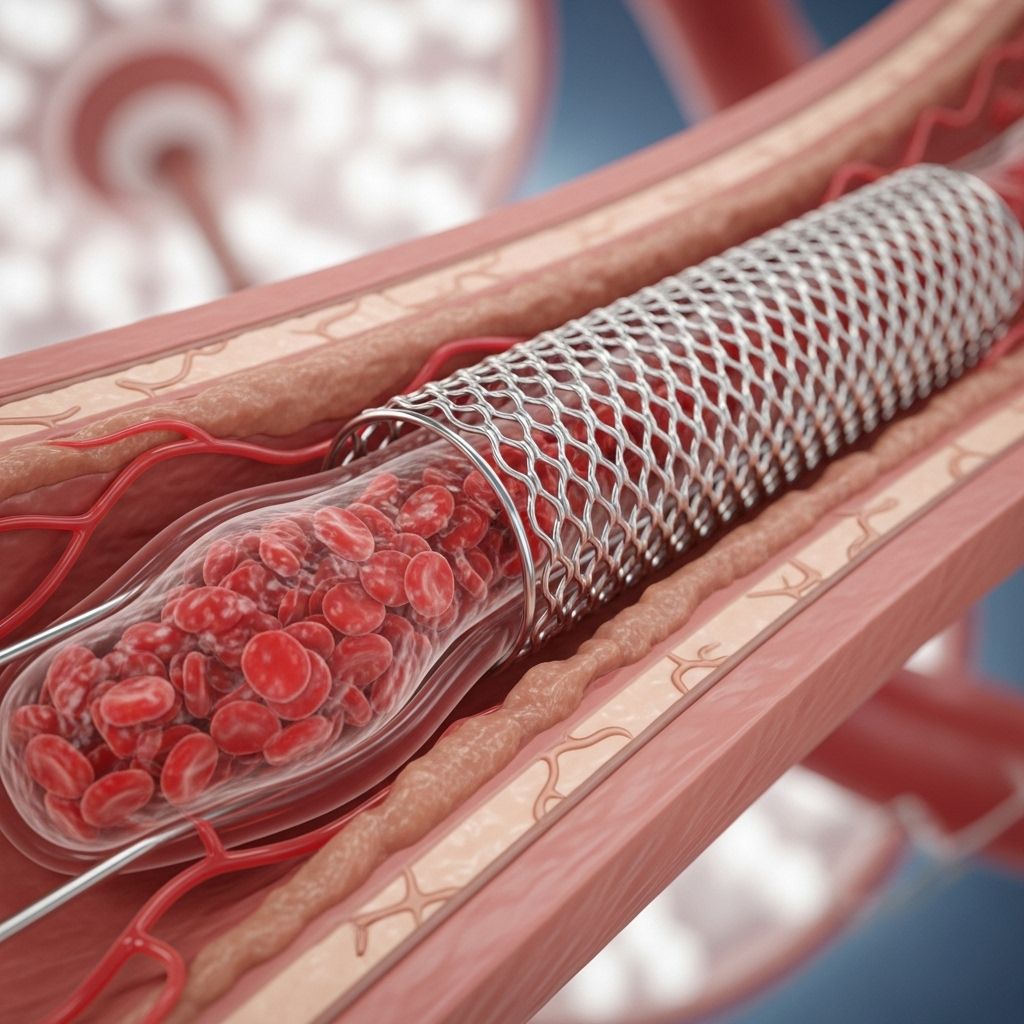
A stent is a tiny mesh tube made of metal or plastic that doctors use to prop open a narrowed or blocked blood vessel. Most commonly, stents are placed in the coronary arteries—the vessels that supply oxygen-rich blood to the heart—to relieve symptoms of coronary artery disease (CAD) and prevent heart attacks.
- Purpose: Prevent the recurrence of narrowing (restenosis) in an artery after angioplasty.
- Common Use: Treat blocked coronary arteries due to cholesterol, fats, and calcium deposits (plaques).
- Material: Often made of metal mesh; some newer types release medication to reduce future narrowing.
The procedure to insert a stent is called percutaneous coronary intervention (PCI) or angioplasty. During this, doctors may also use a tiny balloon to widen the blocked section of the artery before the stent is placed.
Stents and Blood Clots: Understanding the Connection
Stents are highly effective for restoring blood flow, but their presence in a blood vessel—particularly in the heart—can sometimes lead to thrombosis, the formation of a blood clot inside the stent (also called stent thrombosis).
Why do blood clots sometimes form around stents?
- Foreign Material: The stent itself is a foreign object, which can activate the body’s clotting system.
- Injury: Placing a stent can disrupt the artery lining, making it easier for clots to form.
- Plaque Disruption: Stents often go across the areas where plaque is most unstable and prone to clot formation.
While stents prevent future blockages, blood clots inside a stent can completely or partially block the blood vessel, limiting oxygen delivery to the heart muscle and leading to a heart attack.
How Is a Stent Placed? (The Procedure)
Stent placement usually happens in a minimally invasive, catheter-based procedure called angioplasty or PCI (percutaneous coronary intervention):
- A catheter is inserted into a blood vessel (usually in the wrist or groin) and advanced to the blocked coronary artery.
- A small balloon at the end of the catheter is inflated to widen the narrowed artery.
- The stent, pre-mounted on the balloon, is expanded and pressed against the artery wall.
- The balloon is deflated and removed, leaving the stent in place to hold the artery open.
Most patients are awake during this procedure, which typically takes approximately one to two hours. Afterward, the blood flow improves, reducing angina (chest pain) and the risk of heart attack.
Purpose: Why Are Stents Used?
| Condition | Role of Stent |
|---|---|
| Coronary Artery Disease (CAD) | Opens narrowing caused by plaques, restoring blood flow. |
| Acute Myocardial Infarction (Heart Attack) | Keeps artery open after emergency angioplasty post-heart attack. |
| Restenosis (Re-narrowing) | Prevents recurrent blockages after initial treatment. |
Risks: Why Can Stents Lead to Blood Clots?
Although stents help prevent dangerous artery blockages, they also come with some risks, chief among them is stent thrombosis—a blood clot forming inside or near the stent.
Key risk factors include:
- Early discontinuation of antiplatelet medication (like aspirin and clopidogrel)
- Underlying health conditions (diabetes, kidney disease)
- Extent and location of coronary artery disease
- Stent length and number (longer or multiple stents increase risk)
- Poor heart function
Drug-eluting stents (which release a medication to reduce artery narrowing) are generally safer for long-term openness but might slightly increase the risk of late clots compared to older bare-metal stents if antiplatelet therapy is stopped too soon.
Types and Timing of Stent Thrombosis
Medical professionals categorize stent thrombosis by when it occurs:
- Acute: Within 24 hours of stent placement
- Subacute: Between 24 hours and 1 month
- Early: Within 1 month
- Late: Between 1 and 12 months
- Very late: More than 12 months after stent placement
Most clots occur within the first month, but later events can happen, especially if antiplatelet medications are not taken as prescribed.
Symptoms: Recognizing Stent Thrombosis
Stent thrombosis can cause acute coronary syndrome, which can quickly progress to a heart attack. Watch for these urgent warning signs:
- Chest pain, pressure, or discomfort (angina)
- Pain radiating to arms, back, stomach, neck, or jaw
- Shortness of breath
- Weakness or faintness
- Lightheadedness or dizziness
- Nausea or vomiting
- Unexplained sweating
- Pain that lasts for several minutes or comes and goes
Important: Any of these symptoms after a stent procedure should trigger an emergency call to 911 or local emergency services, as immediate treatment can preserve heart muscle and save lives.
After a Stent: Recovery and Prevention
Most patients recover quickly from stent placement, often resuming regular activities within a week. However, follow-up care is crucial to prevent clot formation inside the stent.
Antiplatelet Medications
- Medications like aspirin and P2Y12 inhibitors (e.g., clopidogrel, prasugrel, ticagrelor) reduce the risk of dangerous clotting.
- This is called dual antiplatelet therapy (DAPT).
- Drug-eluting stents: Typically require DAPT for at least 12 months.
- Bare-metal stents: DAPT might be shorter, about 1 month, depending on circumstance.
- Never stop antiplatelet medications without consulting your cardiologist.
Healthy Lifestyle Steps
- Adopt a heart-healthy diet low in saturated fat and rich in fruits, vegetables, and whole grains.
- Engage in regular physical activity after your doctor’s approval.
- Control blood pressure, cholesterol, and blood sugar.
- Quit smoking.
- Maintain a healthy weight.
Stent Thrombosis Outlook
Stent thrombosis is a rare but serious complication. Immediate diagnosis and treatment are vital to preserve heart function and survival. Many patients live full, healthy lives after their procedure, especially with strict adherence to medication and lifestyle recommendations.
Diagnosis and Treatment of Blood Clots in Stents
If your doctor suspects a stent blood clot (stent thrombosis), they may perform the following tests:
- Electrocardiogram (ECG): To detect changes indicating heart muscle damage.
- Blood tests: To assess for markers of heart attack.
- Coronary angiography: To directly visualize blood flow and blockages.
Treatment options may include:
- Repeat angioplasty to reopen the blocked stent and restore flow.
- Thrombolytic therapy (clot-busting medications).
- Intensified antiplatelet or anticoagulant therapy.
- Emergency bypass surgery (rarely, if other approaches fail).
Complications and Prevention Tips
| Potential Complications | Prevention Strategies |
|---|---|
| Heart attack (myocardial infarction) | Adhere strictly to antiplatelet therapy. |
| Sudden cardiac death | Monitor symptoms; respond rapidly to chest pain or shortness of breath. |
| In-stent restenosis (re-narrowing) | Maintain follow-up appointments and healthy lifestyle. |
| Bleeding complications | Discuss medication management with your healthcare provider. |
Frequently Asked Questions (FAQs)
Q: What is the risk of clotting after a stent?
A: The risk is low, especially with modern stents and adherence to prescribed medications. Early discontinuation of antiplatelet therapies significantly increases risk.
Q: How long do I need to take blood thinners after my stent?
A: Most people require dual antiplatelet therapy for at least 12 months after drug-eluting stent placement. Always follow your cardiologist’s instructions and do not stop medication early.
Q: Can you prevent blood clots after a stent?
A: Yes. Take antiplatelet drugs exactly as prescribed, maintain a heart-healthy lifestyle, and keep regular medical appointments.
Q: What happens if a blood clot forms in a stent?
A: A blood clot in a stent can block blood flow and trigger a heart attack. This is a medical emergency requiring immediate treatment.
Q: Are drug-eluting stents safer than bare-metal stents?
A: Drug-eluting stents lower the chance of restenosis but may increase the risk of very late clot formation. Adherence to long-term dual antiplatelet therapy reduces this risk.
When to Seek Medical Attention
Seek emergency care immediately if you experience:
- Chest pain that does not go away with rest
- Shortness of breath
- Fainting or severe lightheadedness
- Pain radiating to your arm, neck, back, or jaw
Quick medical intervention can save heart muscle and lives.
Key Takeaways
- Stents save lives by reopening blocked arteries but carry a small risk of blood clot formation called stent thrombosis.
- Recognize symptoms: Chest pain, shortness of breath, weakness, and sweating after a stent may signal a clot—call for emergency help.
- Prevention is key: Take antiplatelet medication exactly as prescribed and maintain a heart-healthy lifestyle.
- Regular follow-up and communication with your cardiologist help ensure the long-term success of your stent procedure.
References
- https://www.healthline.com/health/heart-disease/stent-blood-clot
- https://www.healthline.com/health/what-is-stent-thrombosis
- https://www.medicalnewstoday.com/articles/stent-thrombosis
- https://www.youtube.com/watch?v=TBdREEzwy7E
- https://www.healthline.com/health/video/how-to-tell-if-you-have-a-blood-clot
- https://www.medicalnewstoday.com/articles/184130
- https://www.heartbeats.org.nz/educate/after-a-heart-attack-all-clogged-arteries-should-be-repaired-researchers-say/
- https://www.dxnimble.com/how-long-do-coronary-stents-last-and-factors-that-influence-their-lifespan/
- https://pacificmedicaltraining.com/life-beyond-heart-disease
- https://prodiadigital.com/en/articles/heart-attack-causes-symptoms-and-first-aid
Read full bio of Sneha Tete












