Understanding Stargardt Macular Degeneration: Causes, Symptoms, Diagnosis, and Living With the Condition
A comprehensive guide to the genetic eye disease that leads to central vision loss, including causes, symptoms, management, and coping strategies.
Understanding Stargardt Macular Degeneration
Stargardt macular degeneration, also known as Stargardt disease or juvenile macular dystrophy, is the most common form of inherited macular degeneration that primarily affects children and young adults. It progressively leads to central vision loss, influencing the ability to read, recognize faces, and perform detailed visual tasks. This comprehensive guide presents an in-depth look at the causes, symptoms, diagnosis, progression, management, and living strategies associated with Stargardt disease.
What Is Stargardt Macular Degeneration?
Stargardt macular degeneration is a rare, inherited eye disorder that causes progressive loss of central (macular) vision due to the accumulation of fatty deposits on the macula, the small central region of the retina responsible for sharp, detailed vision. While predominantly affecting young people, its onset and progression can vary widely, with some individuals experiencing symptoms in adulthood. The disease typically spares peripheral (side) vision, though some forms may eventually impact it as well.
- Most common form of juvenile macular degeneration
- Affects 1 in 6,500 to 10,000 individuals globally
- Often detected between ages 10 and 20, but can begin later
- Progression speed and vision loss severity can differ person to person
Causes and Genetics
Stargardt macular degeneration is genetic in origin. It is usually inherited as an autosomal recessive trait, meaning both parents must carry a faulty gene for the condition to manifest in a child. The principal gene involved is ABCA4, although rare forms can involve the ELOVL4 gene.
Genetic Mechanism
- ABCA4 gene mutations: Lead to faulty production of a protein involved in clearing toxic byproducts from retinal cells. Failure to properly clear these substances results in lipofuscin build-up, damaging light-sensitive cells in the macula.
- ELOVL4 gene mutations: These are much less common and can result in formation of harmful protein aggregates that could disrupt retinal cell functions.
- Over 1,000 different mutations in ABCA4 have been identified, adding to the variability of disease onset and severity.
The inheritance pattern means siblings may also be at risk, particularly if both parents are carriers. Genetic counseling is advised for families with Stargardt disease history.
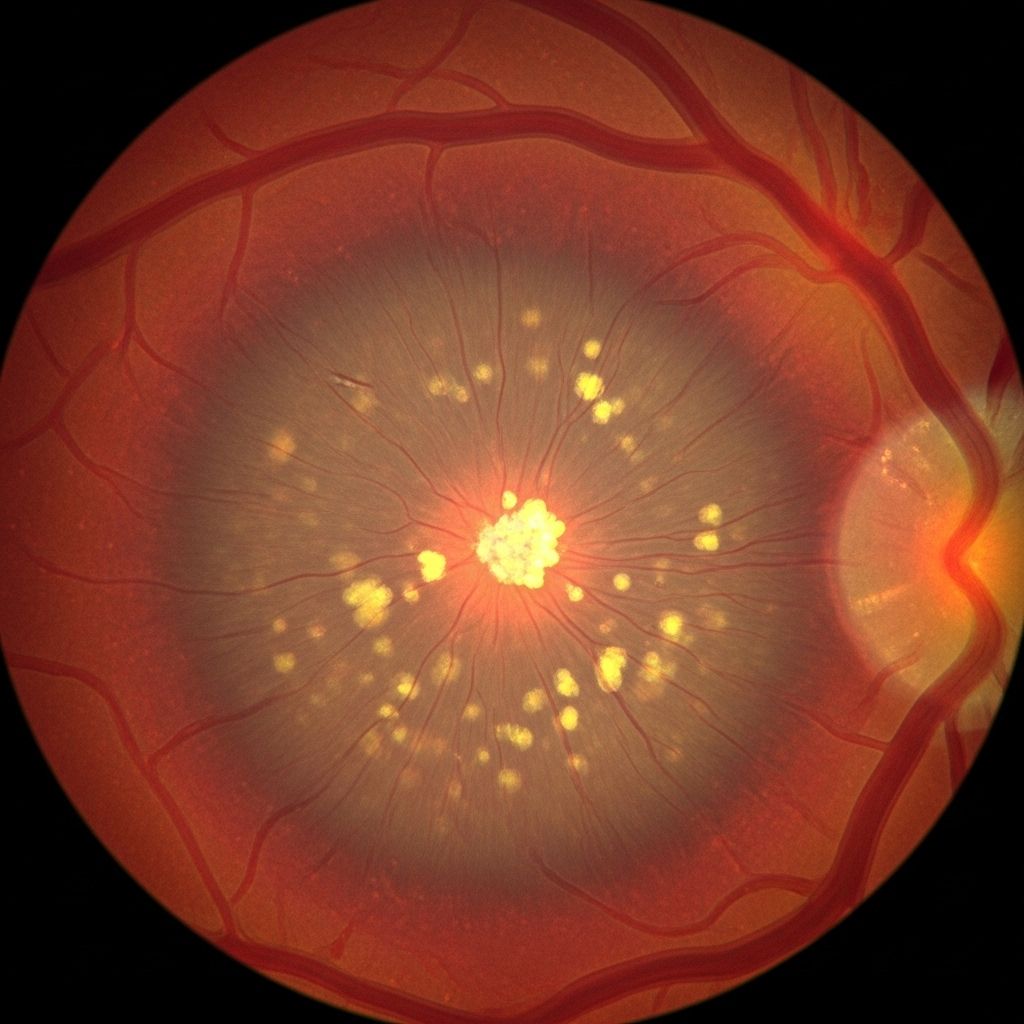
How Stargardt Disease Affects the Eye
The disease targets the central retina (macula), impairing high-resolution vision. Two notable changes are typically seen in the retina:
- Macular changes: The macula may take on an irregular or ‘beaten bronze’ appearance as it deteriorates over time, resulting in decreased visual acuity.
- Yellowish flecks (fundus flavimaculatus): These are accumulations of lipofuscin, a waste product. Some individuals exhibit these flecks even before macular degeneration becomes pronounced.
| Area Affected | Result of Damage | Impact on Vision |
|---|---|---|
| Macula (central retina) | Degeneration of photoreceptors | Loss of central vision, affects detail and color perception |
| Retinal pigment epithelium (RPE) | Build-up of lipofuscin | Progressive visual impairment, potential effect on night vision |
| Peripheral retina (in rare severe cases) | Further cell loss | Possible loss of peripheral vision |
Symptoms of Stargardt Disease
Stargardt disease characteristically causes a gradual decline in central vision, though symptoms and their rate of progression can differ widely.
- Slow, progressive loss of central vision in both eyes
- Difficulty reading, recognizing faces, or performing tasks requiring sharp vision
- Gray, black, or hazy spots (scotomas) in central field of view
- Images appearing wavy or distorted
- Reduced or altered color perception (color blindness possible)
- Increased sensitivity to light (photophobia), presence of glare
- Trouble adjusting between light and dark environments
- Night vision difficulties in some individuals
- Peripheral vision is usually preserved, but may be affected in atypical or advanced cases
Symptoms may first appear as mild visual difficulties before worsening over time. Severity doesn’t always correlate with age of onset.
Who Is At Risk?
Anyone with inherited mutations in the ABCA4 gene is at risk for developing Stargardt disease. Because it is a recessive condition, both parents must carry at least one copy of the faulty gene to pass it on.
- Family history increases risk
- Equal prevalence across genders
- Most common onset: children, teenagers, and young adults, but late onset is possible
Genetic testing is recommended for relatives of affected individuals to clarify risk and support family planning.
Diagnosis: How Is Stargardt Disease Identified?
Diagnosing Stargardt macular degeneration involves both clinical examination and specialized retinal imaging. Early-stage disease may be subtle, making expert evaluation essential.
Diagnostic Steps:
- Ophthalmological exam: Eye doctor checks for macular changes and characteristic flecks using ophthalmoscopy.
- Visual acuity test: To determine central vision clarity loss.
- Retinal imaging:
- Fundus autofluorescence highlights lipofuscin build-up
- Optical coherence tomography (OCT) visualizes cross-sections of retinal layers
- Fluorescein angiography assesses blood flow in the retina to rule out other causes
- Electroretinography (ERG): Measures the retina’s response to light, which can reveal the extent of functional loss
- Genetic testing: Confirms the presence of ABCA4 or ELOVL4 mutations and guides counseling
Early diagnosis is important for maximizing use of remaining vision and accessing management resources.
Progression: What to Expect Over Time
Stargardt disease progression is highly variable. Some individuals experience slow, gradual vision decline over many years, while others lose vision more rapidly. Typically:
- Central vision progressively worsens, with blind spots in the central field enlarging over time
- Peripheral vision generally remains intact, allowing continued independent mobility
- Most people retain some usable vision throughout life
- Color vision and night vision can also decline as the disease advances
- Emotional challenges, such as anxiety and adaptation difficulties, may accompany progression
Managing Stargardt Disease: Treatment and Support
Currently, there is no cure or approved medical treatment to reverse or halt the progression of Stargardt disease, but strategies are available to help affected individuals optimize their remaining vision and maintain independence.
Vision Rehabilitation
- Work with low-vision specialists to assess needs
- Utilize assistive devices such as magnifiers, strong lighting, high-contrast tools, and talking books
- Adapt work and school environments for accessibility and comfort
Protecting Eye Health
- Avoid excessive light exposure by wearing UV-protective sunglasses and hats outdoors
- Do not smoke, as smoking can accelerate retinal damage
- Maintain overall eye health by managing coexisting eye conditions
- Follow a diet rich in healthy nutrients (though no diet can cure or prevent progression)
Potential Research and Emerging Therapies
- Gene therapy: research is ongoing to correct or replace the faulty ABCA4 gene
- Stem cell therapy trials aim to restore retinal function
- Clinical studies are testing drugs to slow lipofuscin accumulation
Participation in clinical trials and staying connected with patient advocacy groups may offer access to new treatments as they become available.
Living With Stargardt Disease
Central vision loss from Stargardt disease can impact daily life, but most individuals are able to lead full and independent lives by utilizing support and adaptive tools. It is essential to address physical, emotional, and practical aspects of adjustment.
Emotional and Social Support
- Connect with support groups for shared experiences
- Access counseling or mental health services if adapting proves challenging
- Educate family, teachers, and employers about the condition for stronger support systems
Strategies for Independence
- Use tactile and auditory cues for navigation
- Learn to read using adaptive techniques such as large print or Braille
- Take advantage of smartphone and computer accessibility features
- Plan environments to enhance contrast and reduce trip hazards
Children and young adults with Stargardt disease can thrive academically with accommodations, and adults can often continue employment with workplace adjustments.
Frequently Asked Questions (FAQs)
What is the primary cause of Stargardt macular degeneration?
The primary cause is mutations in the ABCA4 gene, leading to harmful build-up of fatty deposits in the retina that damage the macula and impair central vision.
Is Stargardt disease contagious or preventable?
No, Stargardt disease is a genetic, inherited disorder and is not contagious or currently preventable.
Can Stargardt disease lead to total blindness?
Complete blindness is rare. Peripheral (side) vision usually remains functional, allowing continued mobility and independence even as central vision declines.
Are there any treatments or cures available?
No cure currently exists. Management focuses on making the most of remaining vision with low vision aids and adapting to changes over time. Research into gene and stem cell therapies is ongoing.
Does avoiding sunlight help slow disease progression?
There is no evidence that avoiding sunlight slows progression, but protecting eyes from excessive UV light is recommended to support overall retinal health.
Can diet or supplements help manage Stargardt disease?
No diet or supplement has proven to alter the course of Stargardt disease. A healthy diet is beneficial for general eye health, but cannot prevent or cure the disorder.
Should people with Stargardt disease drive?
Many people with Stargardt disease are not able to meet the vision requirements for a driver’s license because of central vision loss. Alternatives such as public transportation and accessible travel aids are typically needed.
Where can families find support and resources?
Support is available through low vision rehabilitation services, national and international vision associations, genetic counselors, and patient advocacy groups specializing in retinal diseases.
Key Takeaways
- Stargardt macular degeneration is the leading cause of inherited juvenile macular degeneration and central vision loss in children and young adults.
- It is caused by mutations in the ABCA4 (and rarely ELOVL4) genes, leading to toxic build-up in the retina.
- Symptoms commonly include progressive central vision loss, color vision changes, sensitivity to light, and adaptation difficulties.
- No cure exists yet, but vision rehabilitation and adaptive strategies enable most individuals to maintain full and independent lives.
- Active research promises hope for future gene, drug, and cell-based therapies.
References
- https://medlineplus.gov/genetics/condition/stargardt-macular-degeneration/
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/stargardt-disease
- https://www.mdfoundation.com.au/about-macular-disease/other-macular-conditions/stargardt-disease/
- https://www.rnib.org.uk/your-eyes/eye-conditions-az/stargardt-disease/
- https://www.fightingblindness.org/diseases/stargardt-disease
- https://www.macularsociety.org/macular-disease/macular-conditions/stargardt-disease/
- https://eyewiki.org/Stargardt_Disease/Fundus_Flavimaculatus
- https://www.lowvisionmich.com/low-vision-optometrist/low-vision-eye-diseases/how-stargardt-disease-cause-low-vision/
Read full bio of Sneha Tete












