Staphylococcus (Staph) Infections: Causes, Symptoms, Prevention, and Treatment
Essential information on staph infections: learn about symptoms, risks, prevention, and advanced treatment options.
Staphylococcus infections, often referred to as staph infections, are a common clinical concern that can range from mild skin irritations to serious, potentially life-threatening conditions. Understanding the causes, risk factors, symptoms, and treatments is critical to preventing their spread and ensuring appropriate medical care. This guide offers a detailed overview of staph infections, including prevention strategies, treatment options, and important information on antibiotic resistance.
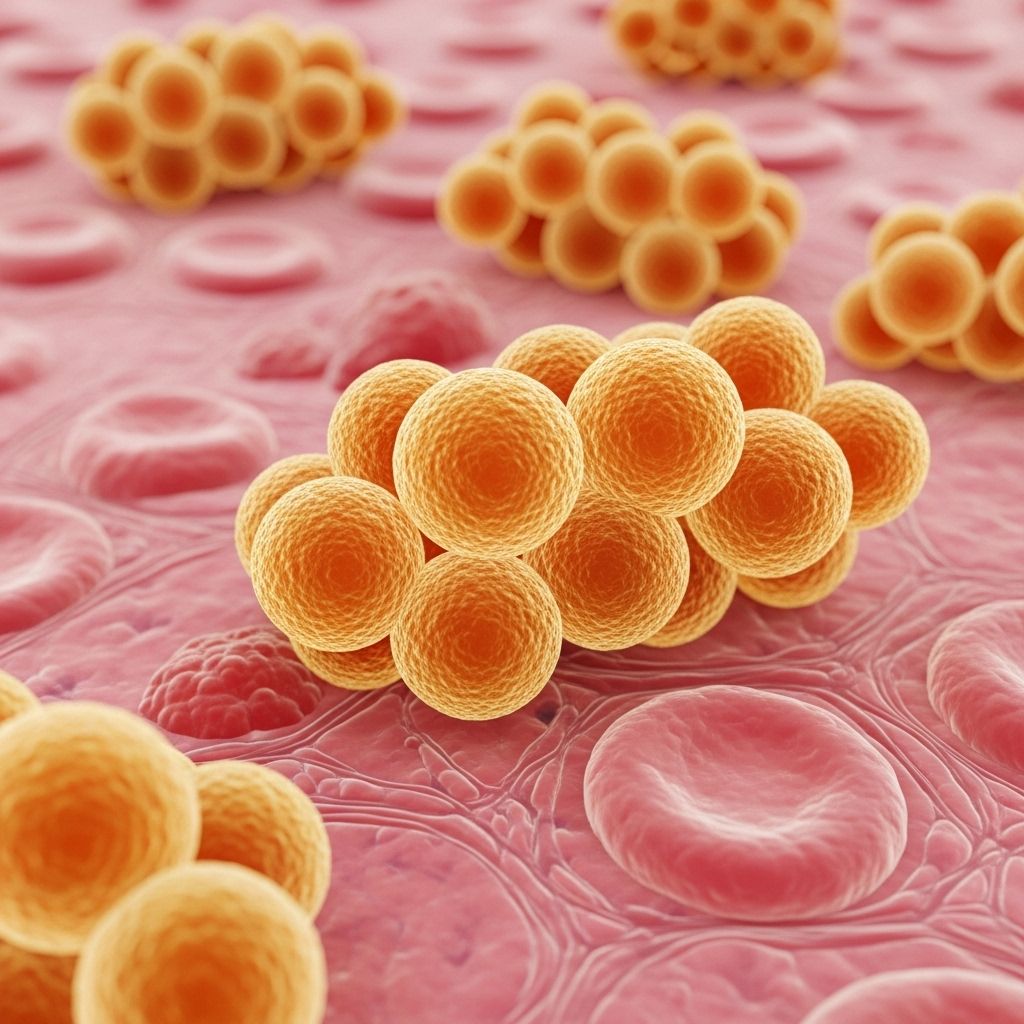
What Is a Staph Infection?
A staph infection is caused by Staphylococcus bacteria, a group of bacteria commonly found on the skin and in the nose of healthy people. While many carry these bacteria without harm, staph can cause infection when it enters the body through cuts, wounds, or medical devices.
- There are more than 30 types of Staphylococcus bacteria; the most significant for humans is Staphylococcus aureus (S. aureus).
- About 20–30% of people carry S. aureus on their skin or in their nasal passages without symptoms.
- Staph infections can be superficial (affecting the skin) or deeper and more severe (affecting blood, bones, or internal organs).
Types of Staph Infections
Staph infections manifest in various ways depending on the location, severity, and bacterial strain. Common types include:
- Skin and Soft Tissue Infections: The most frequent staph infections; presents as boils, impetigo, cellulitis, or abscesses.
- Food Poisoning: Caused by ingestion of food contaminated by staph toxins.
- Bacteremia (Bloodstream Infection): Staph in the blood can lead to serious complications, such as sepsis.
- Bone and Joint Infections: Osteomyelitis (bone infection) and septic arthritis (infection in joints).
- Pneumonia: Especially in individuals with underlying lung conditions or those on ventilators.
- Endocarditis: Infection of the heart valves, which can be life-threatening.
- Toxic Shock Syndrome (TSS): Rare but rapidly progressing illness caused by toxins produced by some strains.
Causes: How Do Staph Infections Occur?
Staph bacteria generally do not cause problems unless they enter the body. Infections typically occur when bacteria gain access through:
- Cuts, scrapes, or wounds
- Pierced skin, such as from surgery or medical devices (catheters, IV lines)
- Injections (injection drug use or medication)
Transmission can occur via:
- Direct person-to-person contact
- Contact with contaminated surfaces or objects, like towels, razors, or gym equipment
- Contact with pus or drainage from a staph lesion
- Eating contaminated food (for staph food poisoning)
Who Is at Risk?
Anyone can get a staph infection, but certain groups are at increased risk:
- People with weakened immune systems (due to conditions like diabetes, cancer, HIV/AIDS)
- Hospitalized patients, especially those in intensive care units (ICUs)
- Individuals with medical devices (catheters, joint prostheses, heart valves)
- People who inject drugs
- Those with chronic skin conditions (eczema, psoriasis)
- Contact sports participants who share equipment or sustain skin injuries
- Individuals living in crowded conditions (prisons, military barracks, shelters)
- People with recent surgery or invasive procedures
Symptoms of Staph Infections
The symptoms of a staph infection depend on the area of the body affected:
- Skin infections: Redness, swelling, warmth, pain or tenderness, pus-filled sores or blisters, crusting or abscesses.
- Bacteremia: Fever, chills, rapid heartbeat, low blood pressure, which may progress to sepsis (life-threatening).
- Bone/joint infections: Localized pain, swelling, warmth, impaired function.
- Pneumonia: Cough, chest pain, fever, shortness of breath.
- Food poisoning: Nausea, vomiting, diarrhea, stomach cramps (usually within hours of eating contaminated food).
- Toxic shock syndrome: Sudden high fever, low blood pressure, rash, confusion, muscle aches, vomiting, diarrhea.
- Endocarditis: Fever, heart murmur, fatigue, chest pain, signs of heart failure.
Complications of Staph Infections
Though many staph infections are mild and treatable, some can become serious or even fatal if not managed promptly. Major complications include:
- Sepsis: A systemic and potentially life-threatening immune response to infection.
- Spread of infection: To bones (osteomyelitis), joints, heart (endocarditis), or lungs (pneumonia).
- Organ failure: Due to widespread infection and sepsis.
- Toxic shock syndrome and necrotizing fasciitis: Rapidly progressing and severe outcomes.
Antibiotic Resistance: What Is MRSA?
An important concern with staph infections is the rise of antibiotic-resistant strains, especially:
- MRSA (Methicillin-Resistant Staphylococcus aureus): Resistant to many common antibiotics, making infections challenging to treat.
- MSSA (Methicillin-Sensitive Staphylococcus aureus): Staph strains still susceptible to methicillin and related antibiotics.
- VISA/VRSA (Vancomycin-Intermediate/Resistant Staphylococcus aureus): Rare, but pose significant treatment challenges.
MRSA infections can occur in healthcare settings (hospital-acquired) or in the community (community-acquired MRSA), affecting otherwise healthy people. Prompt diagnosis and appropriate therapy are vital for antibiotic-resistant staph infections.
How Staph Infections Are Diagnosed
Healthcare providers diagnose staph infections by:
- Obtaining a detailed history and conducting a physical examination.
- Collecting samples for laboratory analysis (such as pus, blood, urine, or sputum cultures).
- Testing for antibiotic sensitivity if bacteria are identified.
- Imaging studies (X-rays, CT scans, MRIs) if deeper infections (bones, joints, or organs) are suspected.
Treatment Options for Staph Infections
Treatment varies according to the type and severity of infection:
- Antibiotics: Most mild infections respond to oral or topical antibiotics. Severe infections may require intravenous antibiotics or prolonged treatment. The choice depends on the strain’s sensitivity.
- Drainage: Abscesses or boils require draining the pus to promote healing and reduce bacteria.
- Surgery: In cases of deep-seated infection (such as endocarditis, osteomyelitis, or infected medical devices), surgical removal or repair may be necessary.
- Supportive Care: This includes fluids, pain relief, and management of complications, such as sepsis.
Some infections, like staph food poisoning, are usually self-limiting and resolve within 24–48 hours. Severe or deep infections require longer recovery and, sometimes, long-term antibiotic therapy or multiple interventions.
Prevention: How to Reduce Your Risk
Good hygiene and preventive measures significantly decrease the risk of staph infection:
- Regular and thorough hand washing with soap and water.
- Cleaning and covering cuts, scrapes, and wounds with sterile, dry bandages until healed.
- Washing clothes, bedding, and towels in hot water and drying them thoroughly.
- Sanitizing shared surfaces and frequently touched items in gyms, community centers, and schools.
- Avoiding sharing personal items such as towels, razors, cosmetics, and sports equipment.
- Maintaining a healthy immune system through balanced nutrition, adequate sleep, and chronic disease management.
Staph Infection Prognosis and Recovery
The outlook varies depending on the type and severity of infection and the individual’s overall health:
- Mild skin infections typically improve within days of starting treatment.
- More serious or deeper infections can take several weeks or months to resolve and may require longer medical follow-up.
- Food poisoning from staph usually resolves in 1–2 days, but full recovery can take a few days longer.
- Severe infections (sepsis, endocarditis, pneumonia) have a more guarded prognosis, especially in vulnerable populations.
When to Seek Medical Attention
Immediate medical care is essential if you experience:
- Rapid swelling, redness, or pain
- Pus-filled sores or abscesses
- High fever, chills, confusion, or rapid heartbeat
- Signs of spreading infection (red streaks, expanding rash)
- Difficulty breathing, chest pain, or severe joint pain
Early diagnosis and treatment are key to preventing complications.
Frequently Asked Questions (FAQs) About Staph Infections
What is the difference between MRSA and regular staph?
MRSA is a strain of Staphylococcus aureus that is resistant to methicillin and many other common antibiotics, making it harder to treat compared to non-resistant (MSSA) strains.
Can staph infections spread between people?
Yes, staph infections are contagious and can be spread by direct contact or by touching contaminated objects and surfaces.
What is the fastest way to cure a staph infection?
Prompt treatment with the appropriate antibiotics and proper wound care can speed recovery. Minor skin infections may heal faster with both antibiotics and drainage, while more severe infections require medical supervision.
How do I know if my staph infection is serious?
Signs of seriousness include rapidly spreading redness, severe pain, swelling, fever, confusion, and any signs of systemic involvement (difficulty breathing, dizziness). Seek medical attention promptly.
Is it possible to prevent staph infections entirely?
Prevention is not always possible, but practicing excellent hygiene and avoiding sharing personal items can dramatically reduce your risk. People at increased risk should take extra precautions in healthcare settings and when using shared facilities.
Summary Table: Key Facts About Staph Infections
| Aspect | Key Points |
|---|---|
| Common Locations | Skin, nose, wounds, blood, joints, heart, lungs |
| Main Bacteria | Staphylococcus aureus |
| Contagious? | Yes, via direct and indirect contact |
| Risk Groups | Immunocompromised, hospitalized, device users, athletes, crowded-living |
| Treatments | Antibiotics, drainage, surgery if severe |
| Complications | Sepsis, organ failure, abscess, chronic infection |
Key Points to Remember
- Staph infections are common, usually mild, but can be serious if untreated or involving antibiotic resistance.
- MRSA is a major concern due to limited treatment options.
- Good hygiene, wound care, and avoiding sharing personal items are vital preventive strategies.
- Medical attention should be sought early for suspicious or worsening symptoms.
References
- https://www.medicalnewstoday.com/articles/staph-infection
- https://www.cdc.gov/staphylococcus-aureus/about/index.html
- https://www.healthdirect.gov.au/staph-infections
- https://www.healthline.com/health/mrsa
- https://www.ncbi.nlm.nih.gov/books/NBK441868/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7244392/
- https://www.aafp.org/pubs/afp/issues/2005/1215/p2474.html
Read full bio of medha deb












