Understanding the Stages of Macular Degeneration
A comprehensive guide to the stages, symptoms, types, and treatments for macular degeneration.
Macular degeneration is a leading cause of vision loss for older adults. Its gradual effect on central vision, vital for reading, driving, and recognizing faces, can majorly impact daily life. This guide explains what macular degeneration is, its progression through key stages, differences that can occur in each eye, and what current treatments can offer to help preserve vision.
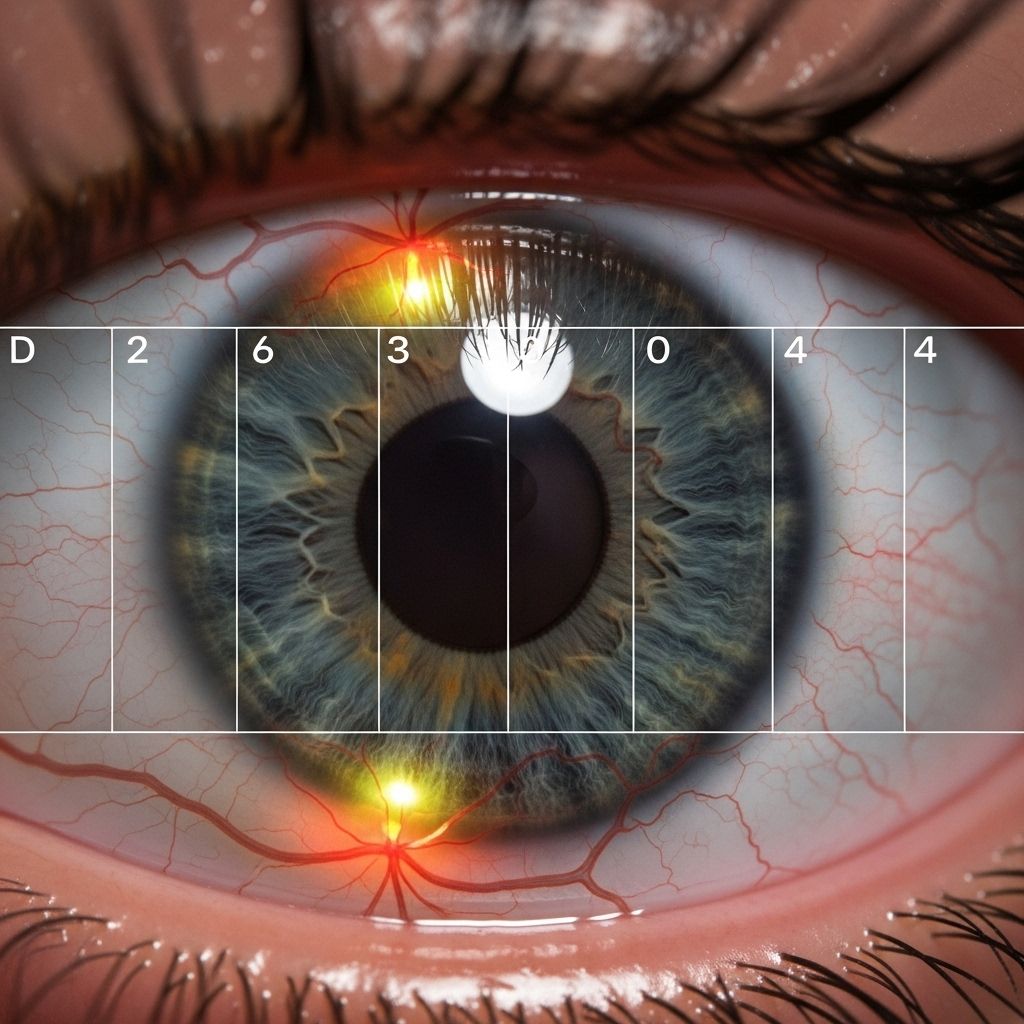
What Is Macular Degeneration?
Macular degeneration is an age-related eye disease affecting the macula—the central part of the retina responsible for sharp central vision. The condition is most common in adults over 50 years old and is also referred to as age-related macular degeneration (AMD). Damage to the macula gradually impairs the ability to see fine details, making everyday activities increasingly challenging. While AMD rarely leads to complete blindness, it can cause significant central vision loss.
- Most prevalent in adults over 50
- Impacts central vision, crucial for activities like reading and driving
- Does not typically result in total blindness, but greatly impairs visual detail
- Two main types: Dry (atrophic) and Wet (neovascular) AMD
How Macular Degeneration Progresses
Macular degeneration is often a progressive disease. The pace and severity of vision loss can vary based on the AMD type and individual health factors. While most people experience a gradual decline, some might maintain stable symptoms for years, or have one eye progress more quickly than the other. Regular eye exams are essential for early detection and management, even when symptoms are not apparent.
- The progression is generally slow, particularly in dry AMD
- Symptoms are often absent in early stages, making regular screening vital
- Some individuals have asymmetrical progression (one eye advances faster)
- Wet AMD can cause sudden, severe loss of vision compared to dry AMD
The Three Stages of Macular Degeneration
Macular degeneration is typically characterized by three main stages: early, intermediate, and late. Each stage is marked by changes in the retina and worsening symptoms. Understanding these stages is critical for recognizing the threats to central vision and taking appropriate action.
Early Stage
The early stage of dry macular degeneration is usually asymptomatic. Individuals do not notice any change in their vision, and the disease is most often discovered during routine eye exams. The key sign is the presence of small to medium-sized yellow deposits called drusen beneath the retina. Eye care professionals recommend periodic eye examinations in at-risk populations to catch this stage as early as possible.
- No noticeable symptoms for most people
- Detected during comprehensive eye exams with the identification of drusen
- Guidelines often advise annual or biennial eye exams for adults over 50 or with risk factors
Intermediate Stage
The intermediate stage may still be silent for some, but for others, mild symptoms start to emerge. The drusen become larger, and the retinal pigment epithelium—the layer that nourishes the retina—may show distinct thinning and damage. Vision changes can include mild central blurriness, reduced contrast sensitivity, or more significant issues seeing in low-light or at night.
- Possible symptoms include slight central vision blurriness or trouble with night vision
- Difficulty seeing in dim light or picking up fine details
- Onset of mild visual distortion (e.g., straight lines appearing wavy)
- Changes may be more pronounced when reading or recognizing faces
Late Stage
Late-stage macular degeneration involves significant functional vision loss. Known as geographic atrophy (GA) in the dry form or as the onset of wet AMD, this stage is when central vision becomes noticeably and often irreversibly degraded. Wet AMD, characterized by the growth of abnormal blood vessels under the retina, can emerge during any stage but always signals an advanced disease state. Sudden or severe vision changes in one or both eyes may occur.
- Pronounced central vision loss, including blind spots (scotomas)
- Straight lines may appear distorted, crooked, or warped
- Increasing trouble with color contrast and adaptation to light
- Possible rapid decline if wet AMD develops due to bleeding or fluid leakage
- Late-stage dry AMD is termed “geographic atrophy” due to atrophic (wasted) areas in the retina
Types of Macular Degeneration: Dry vs. Wet
| Feature | Dry (Atrophic) AMD | Wet (Neovascular) AMD |
|---|---|---|
| Prevalence | 90% of AMD cases | 10% of AMD cases |
| Progression | Slower, gradual | Faster, sometimes sudden |
| Main Pathology | Accumulation of drusen, thinning of retina | Abnormal blood vessels, bleeding, fluid leakage |
| Symptoms | Mild to moderate central vision loss | Rapid, severe central vision loss |
| Stage Structure | Early, intermediate, late | Always represents late/advanced stage |
All cases of AMD begin as the dry form, which may progress slowly through early and intermediate stages. About 10% of cases transform into the wet form, which can cause much more rapid and extensive vision loss.
Symptoms of Macular Degeneration by Stage
- Early Stage: Typically no symptoms. Detected via drusen in eye exams.
- Intermediate Stage:
- Mild blurriness in central vision
- Difficulty seeing at night
- Reduced ability to discern colors or contrast
- Late Stage:
- Significant central vision loss and blind spots
- Distorted or wavy vision (straight lines appear warped)
- Difficulty with reading, driving, or recognizing faces
- Trouble adapting between light and dark environments
- Colors appear faded or less vibrant
- Wet AMD: Symptoms can progress rapidly and may include perceiving straight lines as blurred or wavy, sudden central vision loss, or seeing dark patches in the center of vision.
Can Macular Degeneration Progress Differently in Each Eye?
Macular degeneration commonly affects both eyes, but it does not necessarily do so at the same pace. About 64.5% of people have AMD at the same stage in both eyes, while approximately 35.5% may experience different stages between their eyes. Early AMD in one eye is a strong risk factor for the progression to AMD in the other.
- One eye may remain stable while the other progresses
- Vision loss in one eye can be masked by compensatory visual ability in the other eye
- Both eyes usually progress with age, but at variable rates
- Regular, comprehensive monitoring of both eyes is advised
Treatment Options at Each Stage of Macular Degeneration
While there is no cure to restore lost vision from macular degeneration, there are preventive steps, lifestyle adjustments, and, at advanced stages, medical interventions to help manage the disease and slow its progression:
Early Stage
- Routine monitoring—no specific medical treatment
- Lifestyle changes: Healthy diet (leafy greens, fish, nuts), smoking cessation, blood pressure control, and UV protection
- Scheduled eye exams to detect progression or emergence of symptoms
Intermediate Stage
- Nutritional supplements, specifically the AREDS2 formula (vitamins C & E, copper, zinc, lutein, zeaxanthin), may slow progression
- Continuation of healthy lifestyle habits
- Close follow-up with an ophthalmologist
Late Stage: Geographic Atrophy and Wet AMD
- Dry (Geographic Atrophy): Supportive care, magnifying devices, low-vision therapy, and continued monitoring
- Wet AMD: Anti-VEGF injections to stop abnormal blood vessel growth and reduce fluid leakage
- Options may also include laser therapy in select cases
Assistive technologies like magnifiers, electronic reading devices, and vision rehabilitation programs can further improve quality of life for those with significant visual impairment.
Risk Factors for Developing Macular Degeneration
- Age (most important risk factor, especially over 50)
- Family history and genetics
- Smoking (increases AMD risk two- to four-fold)
- Cardiovascular disease and high blood pressure
- Poor diet or obesity
- Excessive sunlight exposure without eye protection
- Presence of drusen as detected on eye examination
Prevention Tips for Macular Degeneration
- Do not smoke, or quit if you do
- Eat a balanced diet high in dark leafy greens, fruits, and fish
- Maintain a healthy body weight and exercise regularly
- Manage chronic conditions such as hypertension and cholesterol
- Wear sunglasses to limit UV exposure
- Get regular, comprehensive dilated eye exams after age 50 or earlier if at increased risk
How Quickly Does Macular Degeneration Progress?
The timeline for progression varies depending on several factors, including the type and individual risk factors. Dry AMD progression from initial diagnosis to significant vision loss typically spans several years—often up to a decade. Wet AMD, by contrast, can develop rapidly, with vision changes sometimes occurring within days or weeks. Prompt recognition and treatment of wet AMD are critical for preserving as much sight as possible.
Frequently Asked Questions (FAQs)
Can macular degeneration cause complete blindness?
No, macular degeneration does not usually lead to total blindness. Peripheral vision generally remains, but central vision loss can have a substantial impact on daily living.
Is macular degeneration hereditary?
Yes, genetics play a significant role. Having a parent or sibling with AMD increases your risk, though lifestyle factors also influence its development.
Can both eyes be affected differently?
Yes, it is common for one eye to progress faster than the other, and stages can differ. Regular exams are important to monitor both eyes.
What can I do to prevent or slow progression?
Adopt a healthy lifestyle, don’t smoke, protect your eyes from UV, manage chronic medical issues, and follow your ophthalmologist’s recommendations for supplements or monitoring.
How is AMD diagnosed?
An ophthalmologist will conduct a comprehensive eye exam, often using dilation, visual acuity tests, retinal imaging, and an Amsler grid to detect visual distortion.
Is there a cure for macular degeneration?
Currently, there is no cure, but advancements in drug therapy and low-vision aids provide improving options for managing vision loss and maintaining independence.
Conclusion
Awareness of the stages and progression of macular degeneration empowers individuals to seek early care, monitor changes, and adopt lifestyle habits that may help preserve vision. If you are at risk, schedule regular comprehensive eye exams and consult your ophthalmologist about the best preventive and therapeutic measures for you.
References
- https://www.healthline.com/health/eye-health/stages-of-macular-degeneration
- https://www.wandmeyes.com/how-long-does-it-take-for-macular-degeneration-to-progress/
- https://www.macular.org/about-macular-degeneration/what-is-macular-degeneration/types
- https://www.medicalnewstoday.com/articles/stages-of-macular-degeneration
- https://www.medicalnewstoday.com/articles/symptoms-of-wet-amd-progression
- https://www.britannica.com/science/age-related-macular-degeneration
- https://www.visionpointeye.com/eye-diseases-bloomington/macular-degeneration/
- https://www.kivlineyeclinic.com/services/macular-degeneration/
Read full bio of Sneha Tete












