Understanding the Stages of Diabetic Retinopathy: Progression, Symptoms, and Treatment
Get a comprehensive look at the stages of diabetic retinopathy, from early signs to advanced complications and modern treatment options.
Diabetic Retinopathy: An Overview
Diabetic retinopathy is a serious eye complication that can occur in people with any type of diabetes. It develops when elevated blood sugar damages blood vessels in the retina, the layer of tissue at the back of the eye responsible for detecting light and sending images to your brain. Over time, this damage can lead to vision impairment and, if untreated, blindness. Understanding the progression, symptoms, and treatments of diabetic retinopathy is crucial for people living with diabetes and their loved ones.
What Causes Diabetic Retinopathy?
Diabetic retinopathy is primarily caused by chronic high blood glucose levels, which gradually damage the tiny blood vessels in the retina. Key factors that contribute to its development include:
- Poorly controlled blood sugar
- High blood pressure (hypertension)
- High cholesterol
- Having diabetes for many years
- Smoking tobacco products
- Pregnancy in women with diabetes
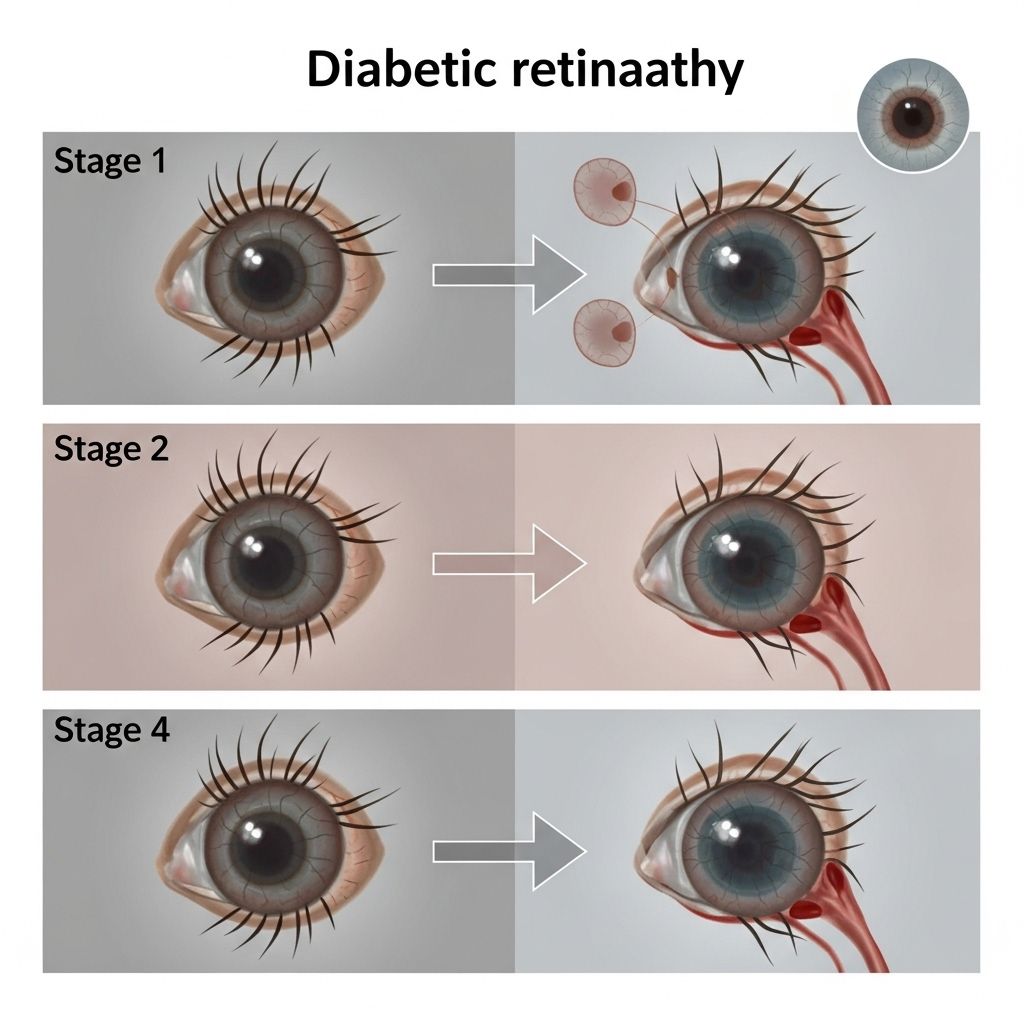
The Stages of Diabetic Retinopathy
Diabetic retinopathy progresses through four main stages, each with unique features and risks. Early stages may not cause noticeable symptoms, which is why regular eye exams are essential for all people with diabetes.
| Stage | Description |
|---|---|
| Mild Nonproliferative Retinopathy | Microaneurysms (tiny swellings) form in retinal blood vessels. Usually, there are no symptoms at this stage. |
| Moderate Nonproliferative Retinopathy | Some blood vessels are damaged, causing them to become blocked or leaky. Small amounts of blood or fluid may leak into the retina. |
| Severe Nonproliferative Retinopathy | More blood vessels are blocked, reducing blood supply to retinal tissue. This prompts the retina to signal for new, abnormal blood vessels to grow. |
| Proliferative Diabetic Retinopathy | The most advanced stage. New, fragile blood vessels grow on the retina and into the vitreous (the gel-like substance filling the eye). These vessels are prone to bleeding, leading to vision loss. |
Mild Nonproliferative Retinopathy
This initial stage is marked by microaneurysms, or small bulges, in the retinal blood vessels. These can leak a tiny amount of fluid into the retina, but there are generally no symptoms. Your ophthalmologist can spot these changes during a comprehensive eye exam.
Key features:
- No symptoms or minor vision changes
- Microaneurysms visible on retinal imaging
- Important to maintain good blood sugar control
Moderate Nonproliferative Retinopathy
As the disease progresses, more blood vessels become damaged. Some may leak blood or fluid into the retina, causing swelling. You may still not notice symptoms, but some people begin to experience blurred vision.
Key features:
- Leaky or blocked blood vessels
- Risk of fluid build-up (macular edema)
- Possible mild vision problems
- Stricter diabetes management advised
Severe Nonproliferative Retinopathy
This stage is characterized by widespread blood vessel blockage, resulting in poor blood supply (ischemia) to parts of the retina. The retina responds by releasing growth factors that stimulate the formation of new blood vessels, setting the stage for the most advanced type of retinopathy.
Key features:
- Large areas of blocked or damaged blood vessels
- Increased risk of developing abnormal new vessels
- Potential for worsening vision
- Frequent monitoring by an eye specialist is crucial
Proliferative Diabetic Retinopathy
This is the most serious and vision-threatening stage. The retina grows new, fragile blood vessels (neovascularization). These abnormal vessels can bleed easily, leading to:
- Hemorrhages into the vitreous, causing sudden vision loss
- Scar tissue buildup, which can pull the retina away from the back of the eye (retinal detachment)
- Severe and permanent vision loss if untreated
What Is Diabetic Maculopathy?
Diabetic maculopathy specifically affects the macula — the area of the retina that provides sharp, central vision used for reading, driving, and recognizing faces.
When fluid leaks into the macula and causes swelling, it is called diabetic macular edema (DME). DME can occur at any stage of retinopathy and is a leading cause of vision loss among people with diabetes.
- Symptoms may not appear immediately
- May result in blurred or wavy central vision
- Early detection is key to preventing permanent vision changes
Symptoms of Diabetic Retinopathy
Many people do not notice symptoms of diabetic retinopathy in its early stages. As it advances, symptoms may include:
- Blurred or fluctuating vision
- Difficulty seeing at night
- Spots, floaters, or dark strings in your vision
- Impaired color vision
- Empty or dark areas in your field of vision
- Sudden vision loss (if bleeding occurs in the eye)
If you notice sudden changes in your vision, seek medical attention promptly.
Risk Factors for Diabetic Retinopathy
Anyone with type 1 or type 2 diabetes is at risk, but some factors increase the likelihood or rate of progression:
- Longer duration of diabetes
- Poor blood sugar control
- High blood pressure
- High cholesterol levels
- Pregnancy in diabetic patients
- Smoking tobacco
- Kidney disease
Diagnosis: How Is Diabetic Retinopathy Detected?
Early detection is vital for preventing vision loss. Diabetic retinopathy is diagnosed through a comprehensive eye exam, which may include:
- Visual acuity test (to assess how clearly you see)
- Dilated eye examination using special drops
- Retinal imaging (such as fundus photography or optical coherence tomography)
- Fluorescein angiography (a dye study to observe blood flow in retinal vessels)
Treatments for Diabetic Retinopathy
The choice of treatment depends on the stage and severity of retinopathy. In the early stages, preserving blood sugar, blood pressure, and cholesterol levels can help slow or halt the disease’s progression. More advanced stages may require medical or surgical interventions.
Early-Stage Management
- Optimal blood sugar control
- Managing high blood pressure and cholesterol
- Regular exercise and a healthy diet
- Smoking cessation
- Routine eye exams every 6–12 months
Advanced-Stage Treatments
- Anti-VEGF injections: These medications block signals that cause abnormal blood vessel growth. Delivered directly into the eye, anti-VEGF injections can reduce swelling and slow vision loss.
- Steroid eye injections or implants: Used to decrease inflammation and swelling in the retina, especially with diabetic macular edema.
- Laser photocoagulation: A focused laser seals or destroys leaking blood vessels, reducing further vision damage. Often performed as an outpatient procedure.
- Vitrectomy: In cases of vitreous hemorrhage or retinal detachment, surgery to remove the blood-filled gel (vitreous) from the eye and repair retinal tissue may be necessary.
| Treatment | Description | Common Use |
|---|---|---|
| Anti-VEGF Injections | Medications injected into the eye to stop abnormal blood vessel growth | Proliferative retinopathy, diabetic macular edema |
| Steroid Injections | Anti-inflammatory steroids injected into the eye | Diabetic macular edema |
| Laser Surgery | Laser seals leaky vessels or inhibits abnormal vessel growth | All advanced stages |
| Vitrectomy | Removal of blood-filled gel and scar tissue from the eye | Severe proliferative retinopathy |
Effectiveness and Goals of Treatment
Treatments primarily aim to prevent further vision loss rather than restore vision already lost. Early intervention and regular monitoring yield the best outcomes, so it’s vital to follow your eye doctor’s recommendations even if you don’t notice symptoms.
Preventing Diabetic Retinopathy and Its Progression
Prevention and early intervention are key. Adopt these strategies:
- Monitor and control your blood sugar carefully
- Keep blood pressure and cholesterol in check
- Have regular comprehensive eye exams
- Maintain a healthy diet and weight
- Don’t smoke
- Report any new vision problems immediately to your doctor
When to See a Doctor
Schedule annual eye exams if you have diabetes, even if your eyesight seems normal. See your eye doctor right away if you:
- Notice sudden changes or blurring in your vision
- See flashes of light, floaters, or dark spots
- Experience loss of vision in one or both eyes
Frequently Asked Questions (FAQs)
What is the difference between diabetic retinopathy and diabetic macular edema?
Diabetic retinopathy refers to all types of diabetes-related damage to the retina. Diabetic macular edema (DME) is a complication of retinopathy where fluid accumulates in the macula, leading to blurred or distorted central vision.
Can diabetic retinopathy be reversed?
Early-stage retinopathy may be halted and even improved with optimal diabetes control, but established damage—especially in advanced stages—usually cannot be reversed. Treatment aims to stop progression and prevent further vision loss.
How often should people with diabetes get eye exams?
An annual comprehensive dilated eye exam is recommended for all people with diabetes. Those with existing retinopathy may need exams more frequently, such as every 3–6 months, depending on severity and doctor recommendations.
Are there any symptoms in early diabetic retinopathy?
Most people have no symptoms in the early stages. This is why regular screening is crucial for detecting changes before they threaten vision.
What lifestyle changes help prevent progression?
Maintaining strict blood sugar control, following a healthy diet, engaging in regular physical activity, managing blood pressure and cholesterol, not smoking, and having regular checkups all help lower the risk of progression or complications.
Summary
Diabetic retinopathy is a gradual, progressive complication of diabetes that threatens eyesight. While not everyone with diabetes will experience vision impairment, risk increases over time without proper management. Early detection, routine eye exams, and prompt treatment remain the best defenses. Every person with diabetes should work closely with medical professionals to protect and preserve their vision throughout life.
References
- https://www.nhs.uk/conditions/diabetic-retinopathy/
- https://www.uchicagomedicine.org/conditions-services/ophthalmology/diabetic-retinopathy
- https://www.californiaretina.com/blog/understanding-the-different-stages-of-diabetic-retinopathy
- https://www.goodrx.com/health-topic/eye/diabetic-retinopathy-causes-stages-symptoms-treatment
- https://my.clevelandclinic.org/health/diseases/8591-diabetic-retinopathy
- https://www.mayoclinic.org/diseases-conditions/diabetic-retinopathy/symptoms-causes/syc-20371611
- https://www.cvpdaytoneyedoctors.com/macular-retinal-diseases/diabetic-eye/
Read full bio of medha deb












