Understanding Spontaneous Coronary Artery Dissection (SCAD): Causes, Symptoms, and Treatment
A detailed guide to the causes, symptoms, diagnosis, risks, and treatment of spontaneous coronary artery dissection (SCAD).
Spontaneous Coronary Artery Dissection (SCAD): Causes, Symptoms, Diagnosis, and Treatment
Spontaneous coronary artery dissection (SCAD) is a rare yet serious cardiovascular event that primarily affects healthy, younger women and can result in heart attacks and sudden cardiac death. This article explores the complexities of SCAD, providing you with thorough, up-to-date information on its causes, risk factors, symptoms, diagnosis, treatment, and recovery.
What is Spontaneous Coronary Artery Dissection (SCAD)?
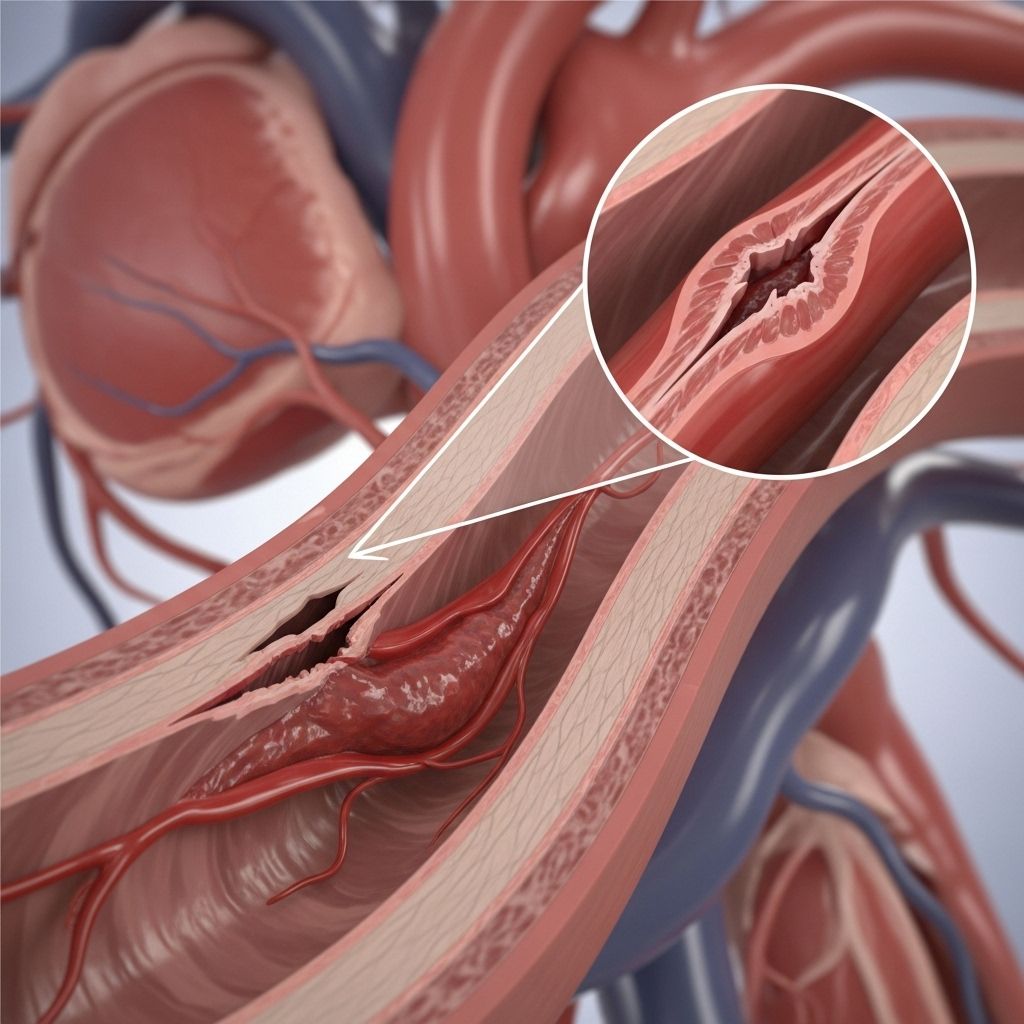
SCAD refers to a sudden tear in one of the arteries of the heart (coronary arteries). This tear allows blood to flow between the layers of the artery wall, causing these layers to separate (dissect). The dissection can slow or block blood flow to the heart muscle, resulting in chest pain, heart attacks, or even cardiac arrest.
- SCAD is different from heart attacks caused by atherosclerosis (plaque buildup).
- It often occurs in healthy individuals, including those without traditional cardiovascular risk factors.
- Most cases of SCAD occur spontaneously, without an obvious cause.
Who is Affected By SCAD?
While anyone can experience SCAD, certain groups are more commonly affected:
- Women account for 80–90% of SCAD cases; younger women and those in the postpartum period are at particularly high risk.
- SCAD can also occur in men, but less frequently.
- It is often seen in people with few or no traditional risk factors for heart disease.
| Demographic | Relative Risk | Notes |
|---|---|---|
| Women (Overall) | High | Particularly ages 30–60 |
| Postpartum Women | Very High | Within weeks of giving birth |
| Men | Low | Less commonly affected, often with other risk factors |
| Those without traditional risk factors | Significant | Can affect healthy and physically active individuals |
Symptoms of SCAD
The symptoms of spontaneous coronary artery dissection are often similar to those of a heart attack. Recognizing them early and seeking immediate medical attention is crucial.
- Chest pain, pressure, or tightness
- Pain radiating to arms, neck, jaw, back, or stomach
- Shortness of breath
- Rapid heartbeat or fluttering sensation in the chest
- Cold sweats or clamminess
- Nausea or vomiting
- Dizziness or lightheadedness
- Extreme exhaustion
- Fainting or loss of consciousness (rare, but possible)
Some people may only experience mild symptoms, while others may have a sudden and severe health crisis (such as a heart attack or even cardiac arrest).
What Causes SCAD?
The exact cause of SCAD is not fully understood, but research has identified several potential triggers and associated risk factors:
- Hormonal changes: Pregnancy and postpartum hormonal shifts are strongly linked. Many cases occur in the weeks after childbirth.
- Underlying blood vessel conditions:
- Fibromuscular dysplasia (FMD): a disease that causes abnormal cell growth in artery walls.
- Other connective tissue disorders like Marfan or Ehlers-Danlos syndromes.
- Extreme physical or emotional stress: Intense exercise, significant emotional events, or severe strain (giving birth, heavy lifting) are sometimes linked to the onset of SCAD.
- Genetics: There may be a hereditary component in some families.
- Other factors: Spontaneous cases with no clear external trigger.
Key Points to Remember
- SCAD usually occurs spontaneously, but may be triggered by physical or emotional stressors.
- Plaque buildup in arteries (atherosclerosis), the most common cause of heart attacks, is not a cause of SCAD.
- The exact mechanisms behind SCAD are still being researched.
Complications Associated With SCAD
SCAD can cause multiple health risks. Complications include:
- Heart attack (myocardial infarction) due to restricted blood flow to the heart muscle
- Heart failure if a large portion of the heart muscle is damaged
- Abnormal heart rhythms (arrhythmias)
- Cardiac arrest in severe cases
- Damage to heart tissue, which may require long-term medications or interventions
Prompt diagnosis and management are critical to reduce these complications.
How is SCAD Diagnosed?
Diagnosing SCAD can be challenging, particularly because many patients are healthy and may not fit the typical profile of heart disease. However, early and accurate diagnosis is vital. Here’s how medical professionals diagnose SCAD:
- Medical history and physical exam: Attention to risk factors (such as recent pregnancy or FMD).
- Electrocardiogram (ECG): Detects irregularities in heart rhythm indicative of heart attack or reduced blood flow. Not all SCAD patients have abnormal ECGs.
- Blood tests: Measurement of troponin levels, a marker of heart muscle damage.
- Coronary angiogram: The gold standard for diagnosis. Uses dye and X-rays to visualize the coronary arteries and locate the tear.
- Advanced imaging:
- Optical coherence tomography (OCT): Provides detailed images of the vessel wall.
- Intravascular ultrasound (IVUS): Uses ultrasound within the artery to assess the extent and location of the dissection.
- CT Coronary Angiography: Noninvasive test that may be used in selected situations.
Current best practice recommends hospital monitoring for at least five days after diagnosis, as recurring dissections most often occur in this period.
SCAD vs. Other Heart Attacks: What’s Different?
Most heart attacks are caused by blockages due to atherosclerosis (plaque). key distinctions between SCAD and typical heart attacks include:
- SCAD happens in younger, healthy people with few or no risk factors.
- No evidence of plaque or cholesterol buildup in the affected arteries.
- More commonly affects women—especially those recently pregnant.
- Different treatment approach, often conservative rather than surgical or stent-based interventions.
How is SCAD Treated?
Treatment options depend on the severity of the dissection, location, number of vessels involved, and patient symptoms.
Conservative (Medical) Management
Most people with SCAD recover without the need for immediate interventions like stent placement or bypass surgery. Many cases of SCAD heal on their own with time and rest.
- Rest and observation: In-hospital monitoring, especially during the first week after SCAD diagnosis.
- Medications:
- Beta-blockers: help reduce the risk of recurrence by lowering heart rate/blood pressure
- Aspirin: reduces the risk of further clot formation
- Other blood thinners if needed (short-term or long-term use)
- Medications for chest pain or blood pressure as needed
Close follow-up with a cardiologist is essential for ongoing management.
Interventional and Surgical Approaches
- Percutaneous coronary intervention (stenting): May be considered if blood flow is critically reduced, or if symptoms persist or worsen. However, stenting can be technically challenging in SCAD patients, and often avoided unless absolutely necessary.
- Coronary artery bypass grafting (CABG): Rare, but might be required in the setting of multiple dissections or failed stenting.
Surgical interventions are reserved for severe cases or when conservative management is not possible.
Cardiac Rehabilitation
- After stabilization, most patients benefit from a structured cardiac rehabilitation program to restore physical function, build confidence, and help reduce anxiety.
Recovering From SCAD
Recovery can be both physically and emotionally challenging. Some key considerations include:
- Exercise restrictions and gradual return to activity as advised by your cardiologist
- Close monitoring for chest pain, fatigue, or other symptoms
- Emotional support and counseling, due to the unexpected and traumatic nature of SCAD events
- Participation in support groups or patient communities can aid in recovery
Most people with SCAD make a good recovery, but risk of recurrence exists. Ongoing care and communication with specialized SCAD clinicians are important for long-term health.
SCAD Recurrence: What Are the Chances?
While many people experience SCAD only once, recurrence is possible. Studies suggest a recurrence rate of around 10–30% over ten years. Risk factors for recurrence may include:
- Personal or family history of SCAD
- Underlying blood vessel conditions (e.g., FMD)
- Poor blood pressure control
Regular follow-up and healthy lifestyle practices are crucial to reduce risk of recurrence.
Prevention: Is SCAD Preventable?
Because SCAD usually occurs spontaneously, there is no definite way to prevent it. Some general strategies may help lower risk:
- Manage stress and avoid extreme physical strain
- Monitor and control blood pressure
- Discuss risks with your healthcare provider if you have a personal or family history of SCAD or connective tissue disease
Frequently Asked Questions (FAQs) About SCAD
Q: What should I do if I think I am having SCAD?
A: If you have sudden chest pain, shortness of breath, or other heart attack symptoms, call 911 or emergency services immediately—do not delay.
Q: Is SCAD the same as a heart attack?
A: SCAD can cause a heart attack if it restricts blood flow, but the underlying cause is different (artery wall tear versus plaque blockage).
Q: Can SCAD be misdiagnosed?
A: Yes. SCAD often affects healthy, young women and may not be suspected initially. Early, appropriate testing (ECG, troponin, angiogram) is essential.
Q: Is SCAD a lifelong condition?
A: For most, SCAD is a single event, but the risk of recurrence remains. Continued follow-up and lifestyle management are important.
Q: Can I exercise again after SCAD?
A: Most people can resume physical activity with guidance from their cardiac team. Cardiac rehabilitation is strongly recommended before returning to normal exercise.
Q: Are there support resources for SCAD patients?
A: Yes. Several national and international organizations (like Beat SCAD, SCAD Alliance, and the American Heart Association) offer resources, support groups, and educational materials.
Key Takeaways
- SCAD is a rare cause of heart attack, mainly affecting healthy women.
- Symptoms closely resemble classic heart attacks and require urgent attention.
- Diagnosis relies on specialized imaging and laboratory tests.
- Most cases are managed without surgery; long-term prognosis is generally positive with proper care.
- Recurrence is possible, making ongoing medical follow-up crucial.
Additional Support and Resources
- Beat SCAD (UK) – Patient stories, support, and event information
- SCAD Alliance (US) – Advocacy, education, and research
- American Heart Association – General heart health and SCAD information
- Local and online support groups
If you or someone you know is at risk, seek immediate care for symptoms and follow up regularly with a healthcare provider experienced in SCAD management.
References
- https://www.heartandstroke.ca/heart-disease/conditions/spontaneous-coronary-artery-dissection
- https://beatscad.org.uk/SCAD-for-Patients/Symptoms-and-Diagnosis
- https://www.rwjbh.org/treatment-care/heart-and-vascular-care/diseases-conditions/spontaneous-coronary-artery-dissection/
- https://stanfordhealthcare.org/medical-conditions/blood-heart-circulation/spontaneous-coronary-artery-dissection/symptoms.html
- https://my.clevelandclinic.org/health/diseases/17503-spontaneous-coronary-artery-dissection-scad
- https://www.heart.org/en/health-topics/heart-attack/about-heart-attacks/coronary-artery-dissection-not-just-a-heart-attack
- https://www.svhhearthealth.com.au/conditions/spontanous-coronary-artery-dissection
- https://www.bhf.org.uk/informationsupport/conditions/spontaneous-coronary-artery-dissection
Read full bio of medha deb












