Understanding the Signs and Symptoms of Hypertrophic Cardiomyopathy
Recognize the symptoms, learn the risk factors, and discover treatment options for hypertrophic cardiomyopathy to manage your heart health.
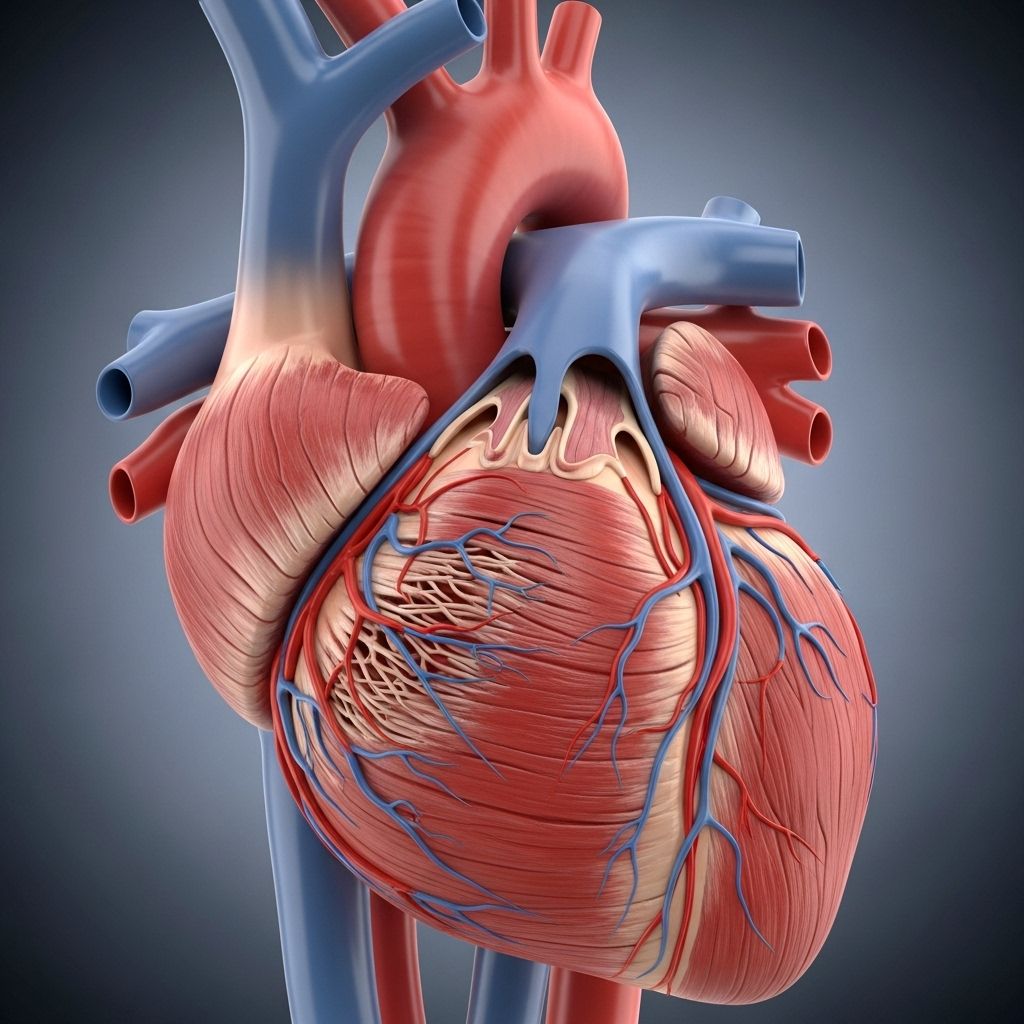
Hypertrophic cardiomyopathy (HCM) is a condition marked by the abnormal thickening of the heart muscle, especially the walls of the left ventricle. This inherited heart disease can affect people of any age but is often discovered during adolescence or early adulthood. While many people with HCM live normal lives without severe symptoms, awareness of its signs and indicators is essential for early detection, appropriate management, and prevention of potential complications such as heart failure or sudden cardiac death.
What Is Hypertrophic Cardiomyopathy?
Hypertrophic cardiomyopathy is a disease in which the heart muscle becomes thicker than usual. The thickening, known as hypertrophy, typically affects the septum — the wall that separates the left and right sides of the heart — making it more difficult for the heart to pump blood efficiently. The disease is commonly inherited and is most often caused by mutations in genes that code for heart muscle proteins. These changes lead to disorganized heart muscle fibers, thick muscle walls, and, in some cases, impaired function of the heart valves.
Early Signs and Symptoms
Many individuals with HCM experience few or no symptoms in the early stages. However, when symptoms are present, they may be subtle and easy to misattribute to other conditions. Early symptoms may occur during physical exertion but can also happen at rest. Watch for the following early warning signs:
- Shortness of breath, especially when engaging in physical activities or sports
- Chest pain (angina), sometimes resembling that of coronary artery disease
- Palpitations or a fluttering, pounding heartbeat
- Fatigue or excessive tiredness, often after light exercise
- Dizziness or lightheadedness, especially when standing up or during activity
- Fainting (syncope), particularly during or immediately after exercise
It’s important to note that these symptoms can also be caused by other heart or lung conditions, so proper medical evaluation is critical.
Advanced Symptoms and Complications
As hypertrophic cardiomyopathy progresses, symptoms usually become more noticeable and may interrupt daily life. The advanced symptoms are generally due to increased obstruction of blood flow from the heart or due to arrhythmias (abnormal heart rhythms):
- Worsening shortness of breath, making regular activities difficult
- Swelling in the legs, ankles, or feet due to fluid buildup (edema)
- Irregular heartbeats (arrhythmias), such as atrial fibrillation, which may feel like a racing or skipped heartbeat
- Increased frequency or severity of chest pain
- Frequent fainting spells, sometimes without clear triggers
One of the most serious complications of HCM is sudden cardiac death, which is more common in young people, particularly athletes, and can occur even without previous symptoms. It is typically triggered by dangerous forms of arrhythmia.
Types of Hypertrophic Cardiomyopathy
HCM is broadly categorized into two types based on the location and extent of heart muscle thickening:
- Obstructive HCM (HOCM): The more common form, where the thickened septum blocks or reduces blood flow out of the left ventricle.
- Non-obstructive HCM: The heart muscle is thickened but does not significantly obstruct blood flow.
Both forms can cause symptoms, but the risk and nature of complications may differ.
Who Is at Risk?
Several factors can increase the risk of developing or experiencing complications from HCM:
- Family history: Having a close relative (parent or sibling) with HCM increases your risk, as the condition is often inherited in an autosomal dominant pattern.
- Genetic mutations: Mutations in specific genes, mainly those involved in the formation of heart muscle proteins.
- Age: While HCM can develop at any age, symptoms often appear during the teenage years or early adulthood.
- Sudden cardiac death in the family: If a close family member has died suddenly or unexpectedly at a young age, especially during exercise.
Genetic counseling and testing are often recommended for relatives of those diagnosed with HCM.
Causes and Risk Factors
The most common cause of hypertrophic cardiomyopathy is mutations in one or more genes that encode proteins of the heart muscle’s contractile apparatus. The condition has an autosomal dominant inheritance, meaning only one parent needs to pass on the gene mutation for the disease to occur.
There are additional risk factors and triggers that may exacerbate symptoms or bring complications to the forefront, including:
- High blood pressure (hypertension)
- Obesity
- Other existing heart diseases
- Use of certain medications that may worsen the obstruction or arrhythmias
When to See a Doctor
You should seek prompt medical attention if you have symptoms suggestive of HCM, particularly if you:
- Experience unexplained fainting or chest pain, especially during exercise
- Have a close family member diagnosed with HCM or who died suddenly and unexpectedly
- Develop new or worsening symptoms like shortness of breath, palpitations, or swelling
Early evaluation, especially through family screening, can help prevent severe complications.
How Hypertrophic Cardiomyopathy Is Diagnosed
The diagnosis of HCM is based on a combination of your symptoms, family history, physical examination, and several heart tests. These may include:
- Electrocardiogram (ECG): This test records electrical activity in the heart and can reveal abnormal rhythms or thickening patterns.
- Echocardiogram: An ultrasound-based test which visualizes heart structures and measures the thickness of heart muscle walls. It is the gold standard for diagnosing HCM.
- Cardiac MRI: Provides detailed images of heart muscle and helps assess the extent and location of muscle thickening.
- Exercise stress testing: Evaluates how the heart responds to physical exertion.
- Genetic testing: Especially important for those with a family history of the disease, as it can identify mutations associated with HCM.
| Test | Purpose |
|---|---|
| Echocardiogram | Visualizes heart muscle thickness and blood flow |
| ECG | Detects abnormal heart rhythms |
| Cardiac MRI | Confirms diagnosis; maps areas of thickening |
| Genetic Testing | Identifies causative mutations in family |
| Exercise Stress Test | Assesses functional impact under physical stress |
Potential Complications of HCM
Although HCM can be managed, there are certain serious complications that can arise, particularly if the condition goes unrecognized or untreated:
- Heart failure: Thickened muscle can reduce pumping efficiency, ultimately leading to fluid buildup and heart failure symptoms.
- Arrhythmias: Both atrial and ventricular arrhythmias can result from muscle disarray, some of which can be life-threatening.
- Sudden cardiac death: Triggered particularly by dangerous ventricular arrhythmias, even in people with few symptoms.
- Stroke: Arrhythmias such as atrial fibrillation increase the risk of blood clots and stroke.
- Mitral valve problems: The thickened heart muscle may interfere with mitral valve function, causing blood to leak backward (mitral regurgitation).
Treatment for Hypertrophic Cardiomyopathy
The primary goals for treating HCM are to alleviate symptoms, improve quality of life, and prevent complications such as sudden cardiac death. The approach depends on the presence and severity of symptoms as well as risk factors for complications.
Medications
Medications are usually the first step in treatment, especially for those with mild or moderate symptoms:
- Beta-blockers: Slow down the heart rate and decrease the strength of contractions, helping the heart fill more effectively.
- Calcium channel blockers: Relax the heart muscle and promote better blood flow.
- Disopyramide: Used specifically to reduce obstruction in those with severe symptoms or who don’t respond to first-line medications.
- Blood thinners (anticoagulants): Important in patients with atrial fibrillation to reduce the risk of stroke.
- Mavacamten: A newer drug option for adults with obstructive HCM who do not respond to standard medications.
Procedures and Surgeries
When medications do not adequately relieve symptoms, or if there is significant obstruction to blood flow, additional interventions may be considered:
- Septal myectomy: An open-heart surgery in which a portion of the thickened septal wall is removed. This is the gold-standard surgical treatment for patients with severe obstruction and symptoms not relieved by medication.
- Alcohol septal ablation: A catheter-based procedure in which alcohol is injected into a small artery supplying the thickened heart muscle, intentionally creating a controlled myocardial infarction to thin the septum and improve blood flow. It can be a preferable option for patients at higher surgical risk.
- Implantable cardioverter-defibrillator (ICD): Recommended for those with a high risk of ventricular arrhythmias and sudden cardiac death. The ICD can detect dangerous arrhythmias and deliver a shock to restore normal rhythm.
- Heart transplantation: Reserved for rare cases of end-stage heart failure that do not respond to other treatments.
Lifestyle Adjustments and Management
While treatment can be effective, lifestyle adjustments play a key role in living well with HCM. Management recommendations include:
- Following medical advice for exercise; some may be restricted from high-intensity athletics or contact sports
- Maintaining a healthy diet and managing other medical conditions such as high blood pressure or high cholesterol
- Regular follow-ups with a cardiologist for ongoing evaluation and management
- Screening of first-degree relatives, as HCM is often inherited
- Avoiding medications that may worsen obstruction, such as certain stimulants and decongestants
Prognosis and Outlook
With proper treatment and monitoring, many people with HCM can lead full and active lives. Advances in medication, device therapy, and surgical interventions have significantly reduced the risk of complications. Family members should be aware of their own risk, and individuals living with HCM should remain vigilant about symptom changes and adhere to their personalized care plans.
Frequently Asked Questions (FAQs)
Is hypertrophic cardiomyopathy always inherited?
Most cases are caused by inherited gene mutations, but in rare cases, it can occur due to spontaneous mutations without a family history.
Can HCM be cured?
There is no cure, but the condition can be managed effectively in most people with a combination of medications, procedures, and lifestyle adjustments.
How is HCM different from other types of cardiomyopathy?
HCM specifically refers to thickening of the heart muscle not due to other causes (like high blood pressure or valve disease) and is frequently inherited. Other types, such as dilated cardiomyopathy, involve enlargement and weakening rather than thickening.
Can I exercise if I have HCM?
Some people can safely participate in low to moderate intensity exercise, but competitive or high-intensity sports may be restricted. Always consult your cardiologist to develop a safe activity plan.
Should my family members get tested?
Yes. First-degree relatives should consider genetic evaluation and regular heart screenings, as timely identification can reduce risks and optimize care.
Takeaway
Hypertrophic cardiomyopathy is a serious, often inherited heart condition marked by thickened heart muscle. Many people remain symptom-free for years, but the condition can progress without notice and pose significant risks. Understanding the early warning signs, undergoing regular cardiac assessment, and working with a specialized healthcare team are crucial in managing HCM and minimizing its impact on your life and those of your loved ones.
References
- https://healthcare.utah.edu/cardiovascular/programs/hypertrophic-cardiomyopathy-program/treatment
- https://www.mayoclinic.org/diseases-conditions/hypertrophic-cardiomyopathy/diagnosis-treatment/drc-20350204
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3078548/
- https://my.clevelandclinic.org/health/diseases/17116-hypertrophic-cardiomyopathy
- https://www.mayoclinic.org/diseases-conditions/hypertrophic-cardiomyopathy/symptoms-causes/syc-20350198
- https://www.heart.org/en/health-topics/cardiomyopathy/what-is-cardiomyopathy-in-adults/hypertrophic-cardiomyopathy
- https://www.pennmedicine.org/conditions/hypertrophic-cardiomyopathy
- https://my.clevelandclinic.org/health/diseases/16841-cardiomyopathy
- https://rarediseases.org/rare-diseases/obstructive-hypertrophic-cardiomyopathy/
Read full bio of Sneha Tete












