Serotonin and Irritable Bowel Syndrome: Understanding the Gut-Brain Connection
Explore how serotonin shapes IBS—impacting gut motility, symptoms, and treatment, in both constipation and diarrhea forms.
Serotonin and IBS: An Overview
Irritable bowel syndrome (IBS) is a frequently diagnosed gastrointestinal disorder characterized by unpredictable symptoms such as abdominal pain, bloating, and altered bowel habits. Recent research has illuminated the central role of serotonin—a neurotransmitter not only vital in the brain but also abundantly present in the gut—in the development, persistence, and treatment of IBS symptoms. Understanding serotonin’s impact on gut physiology is key to offering effective management strategies for both constipation-predominant (IBS-C) and diarrhea-predominant (IBS-D) IBS forms.
What Is Serotonin?
Serotonin, or 5-hydroxytryptamine (5-HT), is a chemical messenger found throughout the body. While it’s well-known for its effects on mood and sleep in the brain, around 95% of the body’s serotonin is produced in the gastrointestinal tract, mainly in specialized cells called enterochromaffin cells.
- Regulates gut motility (how the intestines move contents)
- Impacts intestinal secretion and absorption
- Influences pain perception in the gut (visceral sensitivity)
- Is involved in inflammatory processes within the intestine
Serotonin’s multifaceted role in the gut makes it a pivotal player in the emergence and manifestation of IBS symptoms.
How Serotonin Is Produced and Managed in the Gut
The production and regulation of serotonin in the gut is a complex process:
- Serotonin synthesis starts with the amino acid L-tryptophan.
- L-tryptophan is converted to 5-hydroxytryptophan (5-HTP) via the enzyme tryptophan hydroxylase (TPH).
- 5-HTP is then converted to serotonin (5-HT) by aromatic amino acid decarboxylase.
- There are two variants of TPH:
- TPH1: Found in enterochromaffin (EC) cells of the gut—responsible for about 90% of gut serotonin production.
- TPH2: Present in neurons of the enteric and central nervous systems.
Serotonin is released by EC cells in response to food and other stimuli, and its effects are largely determined by how quickly it is reabsorbed or broken down. This is where the serotonin reuptake transporter (SERT) is critical—it recycles serotonin out of the gut lining so it doesn’t accumulate excessively or become depleted.
The Role of Serotonin in Gut Function
Serotonin acts as a crucial messenger in the enteric nervous system (ENS), the network of nerves governing the digestive tract. Its presence shapes several digestive functions:
- Gut motility: Facilitates the contractions helping food, liquid, and waste move through the gut.
- Secretory activity: Regulates fluid secretion and absorption in the intestines.
- Pain and sensitivity: Increases the sensitivity of gut nerves, potentially leading to symptoms such as abdominal pain or discomfort.
- Inflammation: Can modulate immune cell activity within the intestinal lining.
Disturbances in serotonin signaling can trigger or aggravate IBS symptoms—each subtype (IBS-C and IBS-D) relates to a specific serotonin imbalance.
IBS Subtypes and Serotonin Imbalance
| IBS Subtype | Serotonin Activity | Effect on the Gut |
|---|---|---|
| IBS-C (Constipation) | Low serotonin due to increased SERT activity | Reduced gut motility, leading to constipation |
| IBS-D (Diarrhea) | High serotonin due to decreased SERT activity | Increased gut motility, leading to diarrhea |
Alterations in SERT transcription (how much SERT is made) can result from factors like inflammation, gut microbes, growth factors, and certain peptides. By influencing SERT, these factors control serotonin availability and thus determine IBS symptom patterns.
Serotonin Receptors: The Therapeutic Targets
Serotonin operates on multiple receptor subtypes in the gut. The most notable in IBS are:
- 5HT3 receptors: These increase electrical activity and contraction in the gut, amplifying motility and gut sensitivity. Overactivation is linked to diarrhea.
- 5HT4 receptors: These support gut movement. Agonists (activators) of these can help counteract constipation.
Different medications work by targeting these receptors, thus offering symptom relief tailored to IBS subtypes.
Medications That Target Serotonin in IBS
Modern IBS treatments focus on modulating serotonin activity to restore gut balance. Major approaches include:
- 5HT3 receptor antagonists (for IBS-D): Block excess serotonin signaling at the 5HT3 receptor; reduce diarrhea and visceral pain.
- 5HT4 receptor agonists (for IBS-C): Stimulate the 5HT4 receptor to promote intestinal contraction; address constipation.
- Serotonin modulators:
- Selective serotonin reuptake inhibitors (SSRIs): Enhance serotonin’s availability by blocking its reabsorption; may benefit IBS-C.
- Tricyclic antidepressants (TCAs): Alter serotonin and norepinephrine signaling, especially helpful for pain and IBS-D symptoms.
- Serotonin-norepinephrine reuptake inhibitors (SNRIs): Affect both serotonin and norepinephrine, potentially improving abdominal pain and motility.
Antidepressants (e.g., amitriptyline, duloxetine) do not only lift mood—they interact with serotonin in the gut, modifying pain perception and transit times. Their use in IBS is supported by studies showing improved quality of life and symptom relief, though they may bring adverse effects (e.g., drowsiness, dry mouth).
Other Factors Affecting Serotonin in IBS
Several elements can further influence serotonin production and activity, shaping the IBS experience:
- Gut microbiota: Certain bacteria can alter SERT activity, impacting serotonin levels and gut movement.
- Inflammation: Inflammatory mediators might disrupt SERT regulation, leading to excess or deficient serotonin.
- Hormones and peptides: Growth factors and hormones like glucagon-like peptide-1 can change how SERT works, further affecting serotonin’s influence on the gut.
- Diet and food intake: Nutrient composition can modulate serotonin release from EC cells.
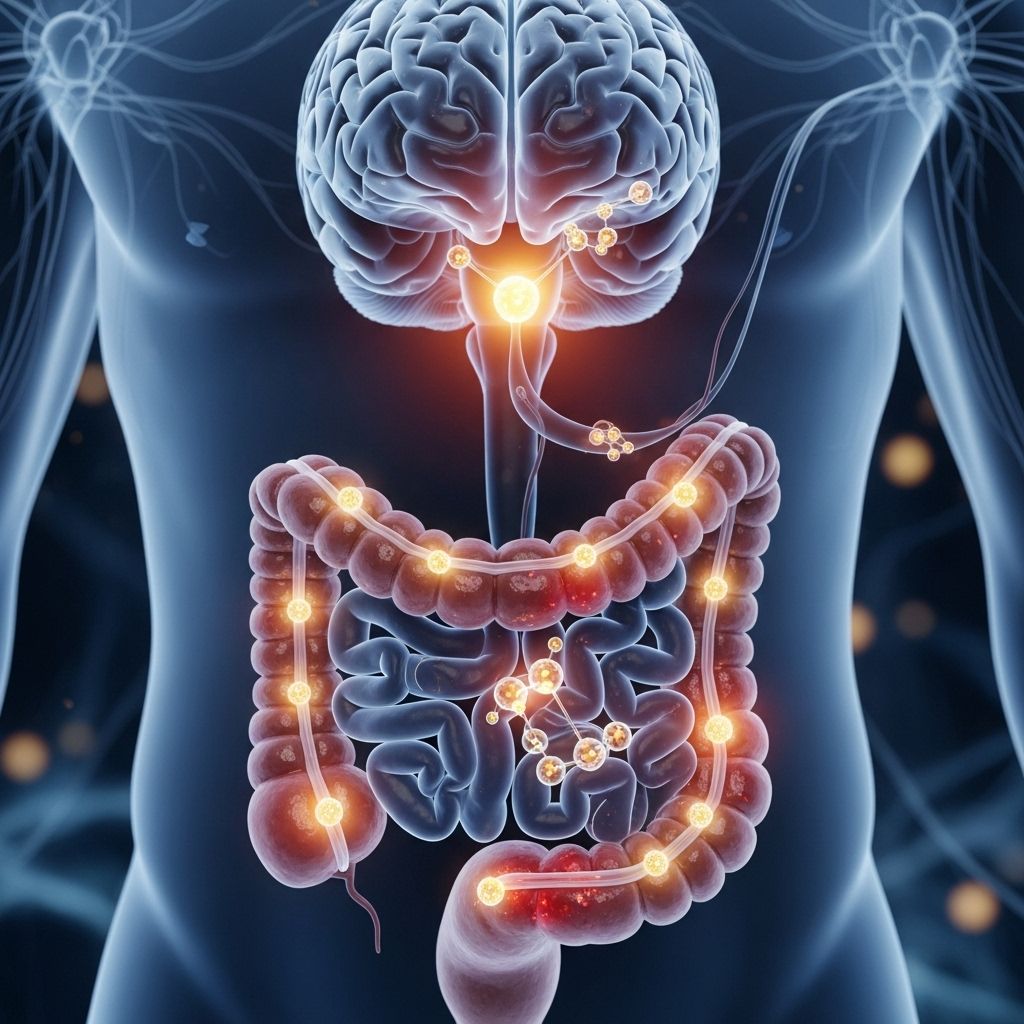
The Gut-Brain Axis: Psychological Stress and Serotonin
The gut and brain are intimately connected via the gut-brain axis, with serotonin serving as a main messenger. Evidence shows that psychological stress can exacerbate IBS symptoms by interfering with serotonin signaling.
Key points from recent studies:
- Chronic psychological stress increases cortisol—a stress hormone—which stimulates colon spasms and abdominal cramps.
- Individuals with IBS display higher baseline cortisol, making them prone to intensified gut discomfort and motility changes.
- Medicines and interventions that modulate serotonin (and dopamine) have observable effects on gut function during periods of stress.
- The gut microbiome produces serotonin; disruption from stress or illness can shift serotonin levels and alter symptoms.
This connection suggests that mental health interventions may complement serotonin-based pharmacological treatments for IBS.
Comparing Serotonin’s Effects in IBS-C and IBS-D
| Feature | IBS-C | IBS-D |
|---|---|---|
| Serotonin Level | Low | High |
| SERT Expression | High | Low |
| Gut Motility | Slow | Accelerated |
| Main Symptom | Constipation | Diarrhea |
| Therapeutic Target | 5HT4 agonists, SSRIs | 5HT3 antagonists, TCAs |
Frequently Asked Questions (FAQs)
What is the main role of serotonin in the gut?
Serotonin controls motility, secretion, and sensitivity in the intestines, impacting how the gut moves contents, responds to pain, and absorbs nutrients.
How does serotonin imbalance lead to different IBS types?
In IBS-C, too little serotonin results in slow transit and constipation. In IBS-D, excess serotonin causes rapid transit and diarrhea.
Can psychological stress affect serotonin levels and IBS symptoms?
Yes—stress increases cortisol, which can trigger gut spasms and alter serotonin signaling, worsening IBS symptoms.
Are antidepressants effective for treating IBS?
Antidepressants such as TCAs and SSRIs can help modulate serotonin in the gut, providing relief from pain and bowel dysfunction, though benefits and side effects may vary between individuals.
Does diet influence serotonin in the gut?
Dietary components—especially those affecting gut microbiota and EC cell activity—can influence serotonin production and thus affect IBS symptoms.
Key Takeaways: Managing IBS through Serotonin Modulation
- Serotonin is central to gut function, with its balance determining whether IBS presents as constipation or diarrhea.
- The serotonin transporter SERT controls available serotonin; disturbances in SERT can trigger IBS symptoms.
- Medications are tailored to correct serotonin imbalances specific to IBS-C (using SSRIs or 5HT4 agonists) and IBS-D (using TCAs or 5HT3 antagonists).
- Stress management is crucial, as psychological factors can exacerbate serotonin-driven gut symptoms.
Further Reading and Resources
- Review articles on serotonin and IBS pathophysiology
- Clinical guidelines for IBS management
- Patient support organizations for IBS and gastrointestinal health
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7505258/
- https://pubmed.ncbi.nlm.nih.gov/18627647/
- https://www.healthline.com/health-news/irritable-bowel-syndrome-how-psychological-stress-contributes-to-ibs-symptoms
- https://my.clevelandclinic.org/health/diseases/4342-irritable-bowel-syndrome-ibs
- https://www.nature.com/articles/s41380-023-01972-w
Read full bio of Sneha Tete












