Septicemia: Causes, Symptoms, Risks, and Treatment
Understand septicemia: its causes, symptoms, life-threatening risks, treatments, and preventative strategies.
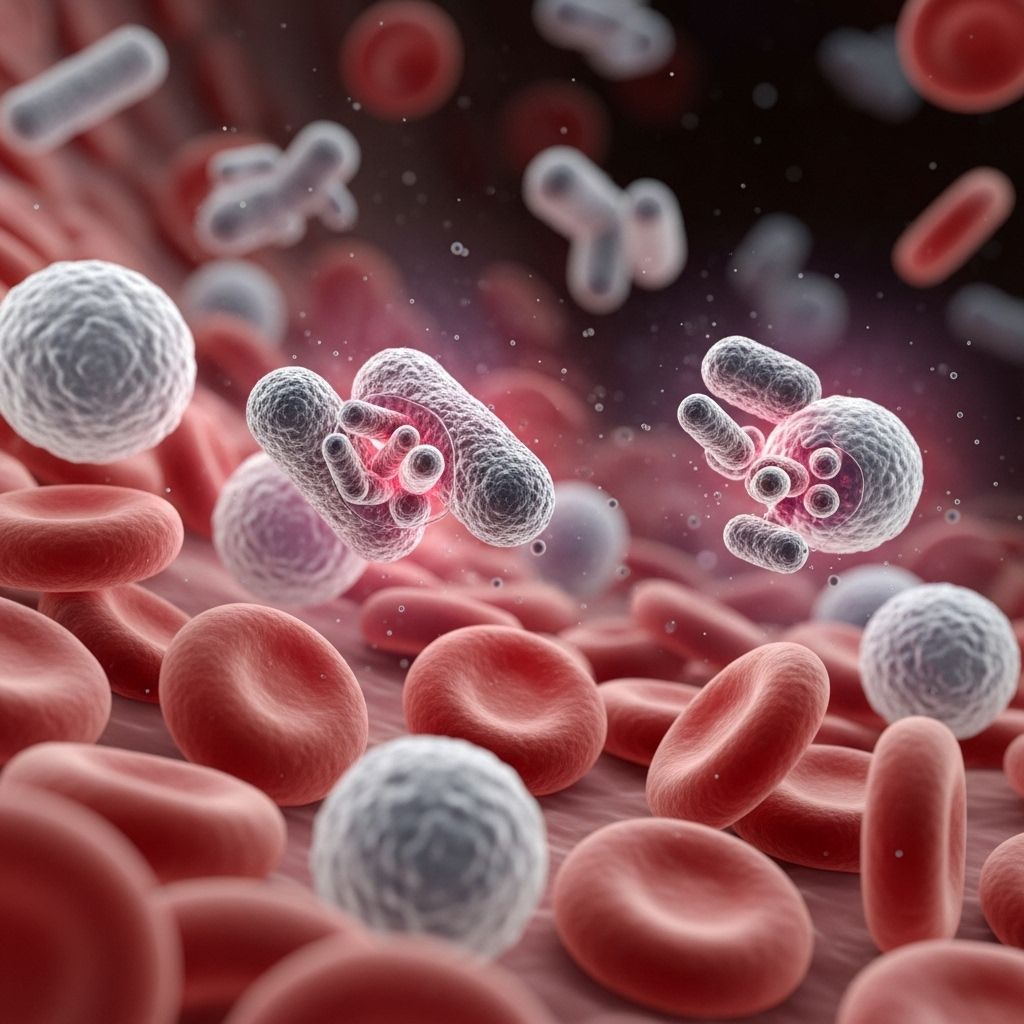
What Is Septicemia?
Septicemia, also commonly called blood poisoning, is a serious bloodstream infection that arises when disease-causing microorganisms such as bacteria, viruses, or fungi enter the bloodstream and multiply rapidly. This condition can quickly escalate to sepsis—a life-threatening inflammatory response that may lead to severe tissue damage, organ failure, and sometimes death if not treated promptly.
How Does Septicemia Occur?
Septicemia starts when germs gain direct access to the blood, possibly through infections elsewhere in the body, open wounds, medical devices such as catheters, or post-surgical sites. The immune system typically fights off a small number of invading germs, but when pathogens multiply faster than the immune defenses, widespread infection results.
- Bacterial infection is the most frequent cause, often from pneumonia, urinary tract infections (UTIs), abdominal infections, or skin infections.
- Viruses or fungi can also sometimes be responsible.
- Entry points: Lungs, urinary tract, abdomen, skin, or open wounds.
Without rapid intervention, septicemia can quickly worsen, overwhelming the body and potentially triggering sepsis, septic shock, and multi-organ failure.
Septicemia vs. Sepsis vs. Septic Shock
| Condition | Description |
|---|---|
| Septicemia | Presence of pathogenic organisms in the blood causing systemic infection. May or may not trigger full-body inflammation. |
| Sepsis | Body’s extreme, overwhelming response to infection, leading to widespread inflammation and tissue damage. Sepsis can result from septicemia or other severe infections. Medical emergency. |
| Septic shock | Advanced stage of sepsis with severe circulatory, metabolic, and cellular disturbances. Often includes dangerously low blood pressure that does not respond to fluids. |
Causes and Risk Factors
Septicemia can be caused by a wide range of pathogens that invade the bloodstream:
- Bacteria: The leading cause, particularly from infections in the lungs (pneumonia), urinary tract, digestive tract, or skin.
- Viruses: Such as influenza, certain coronaviruses.
- Fungi: Such as Candida, especially in immunocompromised patients.
Some key risk factors include:
- Weakened immune system (due to chronic illness, cancer therapy, HIV/AIDS, organ transplantation, etc.)
- Older adults and infants
- Indwelling medical devices such as catheters, IV lines
- Recent surgery or hospitalization
- Open wounds or burns
- Untreated or severe infections
Symptoms of Septicemia
Early detection is critical for effective treatment. Symptoms of septicemia can develop quickly and often include:
- High fever, sometimes with chills or shivering
- Rapid heart rate (tachycardia)
- Rapid breathing (tachypnea)
- Low blood pressure
- Confusion or disorientation
- Extreme weakness or lethargy
- Lightheadedness or dizziness
Other possible signs include clammy or sweaty skin, decreased urination, or mottled/discolored skin. As the infection progresses, vital organs may begin to fail, leading to further complications.
Complications of Septicemia
- Sepsis: Septicemia can rapidly progress to sepsis, an extreme life-threatening immune response causing widespread tissue damage and organ failure.
- Septic shock: A severe drop in blood pressure leading to poor organ perfusion and a high risk of coma or death.
- Organ dysfunction or failure: Including the kidneys, liver, lungs, and heart. Acute respiratory distress syndrome (ARDS) is a risk.
- Amputation: In cases of severe circulation loss to limbs.
- Death: Septicemia and sepsis are medical emergencies with significant mortality rates.
Diagnosis
Septicemia diagnosis requires prompt recognition, as early intervention is key to survival. Diagnosis involves:
- Clinical assessment: Evaluation of symptoms, vital signs, and risk factors
- Laboratory tests:
- Blood cultures: To identify the causative organism
- Complete blood count (CBC): To assess white cell counts
- Blood chemistry tests: To detect organ dysfunction
- Lactate levels: Elevated with sepsis/septic shock
- Other cultures: Such as urine, sputum, wound swabs if an infection source is suspected
- Imaging: X-rays, CT scans, or ultrasounds may be used to locate infection sources
Treatment of Septicemia
Immediate treatment is essential. Septicemia is a life-threatening emergency; prompt intervention increases survival rates significantly.
Medications
- Antibiotics: Broad-spectrum antibiotics are started intravenously, targeting a wide range of bacteria, and later refined once the precise organism is identified.
- Antivirals or antifungals: If the infection arises from viruses or fungi, specific medications are prescribed.
- Vasopressors: Medications such as norepinephrine may be given to raise and maintain blood pressure if fluids alone are insufficient.
- Pain relievers, corticosteroids, or insulin: To manage pain, inflammation, and blood sugar as needed.
Supportive Care
- IV fluids: Large volumes are administered early to treat or prevent shock.
- Oxygen therapy: Supplemental oxygen or mechanical ventilation if breathing is impaired.
- Dialysis: For kidney support if acute kidney injury occurs.
- Nutritional support: Enteral or parenteral nutrition as needed during prolonged illness.
Surgery
- Sometimes needed to drain pus-filled abscesses, remove dead or infected tissue, or control the source of infection.
Hospitalization and Monitoring
Patients with septicemia require:
- Intensive monitoring in a hospital, often in the Intensive Care Unit (ICU)
- Frequent reassessment of vital signs, organ function, and laboratory values
- Ongoing evaluation for complications or the need for advanced supportive therapies
Outlook and Recovery
The prognosis for septicemia depends on how quickly treatment begins, the patient’s overall health, age, the infectious organism, and the severity of organ involvement. Most people who survive septicemia begin to recover within weeks, although those with severe illness may take months, and some experience post-sepsis syndrome, with lingering physical and psychological symptoms such as:
- Fatigue and muscle weakness
- Difficulty concentrating, memory problems, or “brain fog”
- Insomnia, nightmares, or mood changes
- Persistent pain or discomfort
- Anxiety or depression
Patients recovering from severe septicemia may also endure long-term organ damage or disabilities including limb amputation in extreme cases.
Prevention
- Timely treatment of infections: Seek prompt medical care for any signs of infection, especially if you have a weakened immune system, chronic disease, or have recently undergone surgery.
- Good hygiene practices:
- Wash hands regularly
- Clean and cover all wounds
- Follow sterile techniques during medical procedures
- Vaccination: Routine immunizations, especially against pneumonia and influenza, help lower the risk of serious infections that can lead to septicemia.
- Manage chronic conditions: Keep diseases like diabetes or kidney conditions under control to reduce infection risk.
Frequently Asked Questions (FAQs)
Q: What is the difference between septicemia and sepsis?
A: Septicemia refers to the invasion and multiplication of disease-causing microbes in the bloodstream. Sepsis is a potentially life-threatening reaction by the body to that infection, often causing widespread inflammation, organ dysfunction, or failure.
Q: How quickly does septicemia become dangerous?
A: Septicemia can progress extremely rapidly, sometimes within hours, to severe sepsis or septic shock, making immediate medical attention critical.
Q: Can septicemia be cured?
A: With prompt diagnosis and aggressive treatment, including antibiotics and supportive care, many people fully recover. Delays in treatment increase the risk of death or lasting damage.
Q: Who is most at risk for developing septicemia?
A: Those at highest risk include infants, older adults, people with weakened immune systems, chronic health problems, recent surgical patients, and individuals with untreated or severe infections.
Q: Is septicemia contagious?
A: Septicemia itself is not contagious, but the underlying bacteria or viruses can be spread by direct or indirect contact, depending on the microbe involved. Standard infection control measures minimize this risk.
Key Points to Remember
- Septicemia is a medical emergency demanding fast diagnosis and treatment.
- Increasing awareness of early symptoms (fever, rapid heartbeat, confusion) is crucial for early intervention.
- Survivors may face long-term health effects; prevention strategies focus on infection control and prompt treatment.
- Regular follow-up and rehabilitation may be necessary for those recovering from severe septicemia or sepsis.
References
- https://my.clevelandclinic.org/health/diseases/21539-septicemia
- https://www.healthline.com/health/sepsis
- https://en.wikipedia.org/wiki/Sepsis
- https://www.mayoclinic.org/diseases-conditions/sepsis/diagnosis-treatment/drc-20351219
- https://www.medicalnewstoday.com/articles/305782
- https://my.clevelandclinic.org/health/diseases/12361-sepsis
- https://www.mayoclinic.org/diseases-conditions/sepsis/symptoms-causes/syc-20351214
- https://www.webmd.com/a-to-z-guides/sepsis-septicemia-blood-infection
Read full bio of medha deb












