Septal Myectomy: Surgery, Recovery, Risks, and Alternatives for HCM
Detailed guide on septal myectomy surgery for hypertrophic cardiomyopathy, covering procedure, recovery, risks, and treatment options.
Septal Myectomy: Surgery for Hypertrophic Cardiomyopathy (HCM)
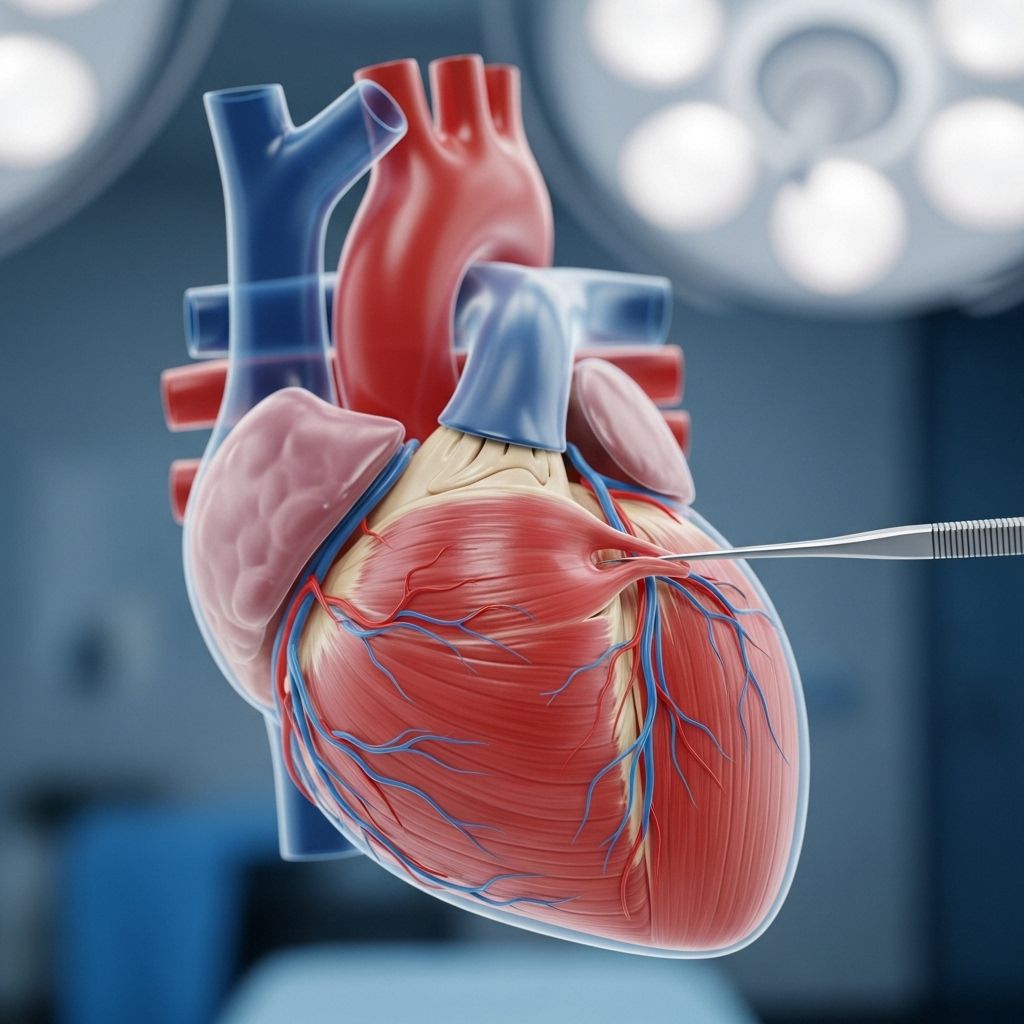
Septal myectomy is an open-heart surgical procedure used to treat severe forms of hypertrophic cardiomyopathy (HCM), an inherited condition resulting in abnormal thickening of heart muscle, particularly the septum (inner wall) of the left ventricle. By removing a portion of the thickened septal wall, septal myectomy can relieve left ventricular outflow tract (LVOT) obstruction and improve heart function for eligible patients, often leading to significant improvement in symptoms and quality of life.
Who is Septal Myectomy For?
Septal myectomy is generally recommended for individuals diagnosed with HCM who experience:
- Severe, drug-resistant symptoms (such as chest pain, shortness of breath, significant exercise intolerance)
- Documented left ventricular outflow tract obstruction affecting blood flow from the heart to the body
- Ongoing heart failure risk due to obstruction despite optimal medical therapy
While most candidates are adults, myectomy may also be performed in children and infants in rare cases of severe congenital HCM, such as those linked to genetic syndromes like Noonan syndrome. Proper patient selection, based on thorough imaging and assessment of symptoms, is critical for ensuring good outcomes.
Preparation for Septal Myectomy
Preparation for the surgery typically includes:
- Comprehensive physical examination and review of symptoms
- Imaging studies (echocardiogram, cardiac MRI, sometimes cardiac catheterization) to map septal thickening and LVOT obstruction
- Discussion of risks, benefits, and alternative treatments with the patient and family
- Arrangements for hospital stay and postoperative support
Some patients may be instructed to adjust medications or dietary habits, and all will be advised to fast prior to surgery.
Septal Myectomy Procedure: Steps and Techniques
Septal myectomy is an open-heart procedure performed under general anesthesia. There are several approaches, but the general steps include:
- Incision and Access: The surgeon makes a large incision down the center of the chest and splits the breastbone (sternotomy) to access the heart.
- Heart-Lung Machine: Catheters are placed to connect the patient to a cardiac bypass (heart-lung) machine, which temporarily takes over heart and lung function during the operation.
- Septal Muscle Removal: The surgeon identifies and carefully removes the thickened septal tissue causing the obstruction. If HCM has affected the mitral valve, the surgeon will repair this valve at the same time if needed.
- Restoring Function: Blood flow is restored from the cardiac bypass machine, and the heart is restarted.
- Closure: The breastbone is wired back together, and the incision is closed with sutures.
Advanced techniques and careful planning are essential to avoid complications such as incomplete resection, heart block, or injury to the valves. Concomitant mitral valve surgery (repair is preferred over replacement) may be performed in cases with severe mitral valve disease.
| Step | Description |
|---|---|
| 1. Anesthesia | General anesthesia is administered to ensure patient is fully asleep. |
| 2. Sternotomy | Chest incision and breastbone split to access the heart. |
| 3. Cardiac Bypass | Heart-lung machine takes over circulation. |
| 4. Septal Resection | Diseased septal muscle tissue is carefully excised. |
| 5. Valve Repair | If indicated, mitral valve is repaired. |
| 6. Restoration | Blood flow and heart rhythm are restored. |
| 7. Closure | Breastbone is rewired, incision closed. |
Recovery After Septal Myectomy
It is an invasive operation, so patients should expect to stay in the hospital for several days:
- Initial recovery in an intensive care unit (ICU) for close monitoring
- Average total hospital stay is about 4.9 days, according to recent clinical studies at high-volume referral centers
- Hospital stay may be longer (average 5.8 days) for patients developing complications such as atrial fibrillation
- Gradual transition to an inpatient unit, with monitoring of heart rhythms and wound healing
After discharge, recovery at home typically spans 6 to 8 weeks, during which patients need to restrict physical activities and follow up regularly with their doctor to monitor healing and symptom improvement. It is crucial to watch for signs of infection, arrhythmias, or worsening symptoms.
Complications and Risks
Septal myectomy is regarded as one of the safest open-heart surgeries when performed at experienced, high-volume HCM centers, with a mortality risk as low as 0.4% in dedicated centers. Complications are rare, but can include:
- Bleeding or infection at the incision site
- Abnormal heart rhythm (especially atrial fibrillation, heart block)
- Injury to the aortic or mitral valves, possibly requiring additional surgery
- Incomplete muscle resection leading to persistent obstruction
- Stroke or other major operative risks (extremely rare in expert centers)
Risks are notably higher in low-volume community hospitals, which lack specialized teams and experience with HCM surgeries. In expert centers, operative risks are even lower than coronary bypass or valve replacement surgeries.
Long-Term Outlook
The prognosis following septal myectomy is generally excellent for well-selected patients:
- Marked reduction or elimination of LVOT obstruction
- Sustained improvement in exercise tolerance and heart failure symptoms
- Low risk of major complications when performed by experienced surgical teams
- Quality of life improvements similar to normal population, particularly in adult patients
Long-term follow-up is essential to monitor for late complications, recurrence of obstruction, arrhythmias, or progression of valve disease. In pediatric cases, outcomes can also be favorable despite higher baseline risks linked to genetic syndromes such as Noonan syndrome.
Alternative Treatments to Septal Myectomy
Treatment for hypertrophic cardiomyopathy centers on symptom control and prevention of complications. Alternatives to septal myectomy include:
- Medication therapy: Beta-blockers, calcium-channel blockers, and antiarrhythmics may help control symptoms in many patients.
- Alcohol septal ablation: A less invasive approach where a catheter delivers alcohol to the area of thickened septum, causing it to shrink through a controlled heart attack. Suitable for some patients not candidates for surgery, but risk of complications is higher and may cause heart block, requiring pacemaker.
- Implantable cardioverter defibrillator (ICD): Used for individuals at risk of sudden cardiac death due to arrhythmias.
- Pacing treatments: May help reduce outflow obstruction in some cases.
- Mitral valve surgery: Repair or replacement may be required in some cases with significant mitral regurgitation or structural abnormalities.
The choice among these treatments depends on the patient’s age, symptom severity, coexisting medical conditions, and the presence of anatomical variants within the heart.
Cost of Septal Myectomy
The cost of septal myectomy can vary widely based on factors such as geography, hospital setting, physician expertise, insurance coverage, and whether additional procedures (e.g., mitral valve repair) are performed.
- Costs can range from tens of thousands to over a hundred thousand USD.
- Insurance coverage varies; many policies cover the procedure when deemed medically necessary.
- Costs may include hospital stay, surgeon and anesthesiologist fees, imaging, and post-operative rehabilitation.
Patients should work with hospital billing departments and their health insurer for detailed cost estimates and coverage verification before surgery.
Frequently Asked Questions (FAQs)
What are the benefits of septal myectomy for HCM?
Septal myectomy can alleviate severe heart failure symptoms, restore normal blood flow from the heart, and greatly improve quality of life in people with obstructive HCM.
How long is the hospital stay after surgery?
Most patients spend about 4-5 days in the hospital, starting in ICU and moving to a regular cardiac care room as they recover.
What risks should I consider before surgery?
Risks include bleeding, infection, arrhythmias, and rare chance of stroke or death. These risks are minimized when surgery is performed at high-volume HCM centers by experienced teams.
Is mitral valve surgery always needed during myectomy?
Not always. Most mitral regurgitation related to HCM is resolved by removing the thickened septum. Mitral repair is performed only if there is intrinsic valve disease.
Are there less invasive alternatives to myectomy?
Alcohol septal ablation is less invasive but carries distinct risks such as heart block requiring a pacemaker. Medical management may be possible in mild or moderate cases.
Will my symptoms ever return?
In most carefully selected patients, septal myectomy produces long-lasting relief from symptoms. Ongoing follow-up is important to address any recurrence or new heart problems.
Key Takeaway
Septal myectomy is a highly effective and safe surgical option for individuals with severe, drug-resistant hypertrophic cardiomyopathy and significant LVOT obstruction, especially when performed in specialized centers. The recovery period involves both hospital and home-based phases, with most patients achieving symptom resolution and improved quality of life. Alternative treatments exist, but myectomy remains the gold standard for those with severe obstruction. Discuss options thoroughly with your cardiologist to determine the best strategy based on your individual health needs and circumstances.
References
- https://www.healthline.com/health/heart/septal-myectomy
- https://www.ahajournals.org/doi/10.1161/circ.132.suppl_3.13977
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5973224/
- https://academic.oup.com/ejcts/article/53/3/538/4568989
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9569270/
- https://www.healthline.com/program/the-facts-you-need-to-manage-hypertrophic-cardiomyopathy
Read full bio of medha deb












