Understanding Secondary Cataracts: Causes, Symptoms, and Treatment
A comprehensive guide to secondary cataracts, their symptoms, risk factors, and the latest treatment options after cataract surgery.
Understanding Secondary Cataracts
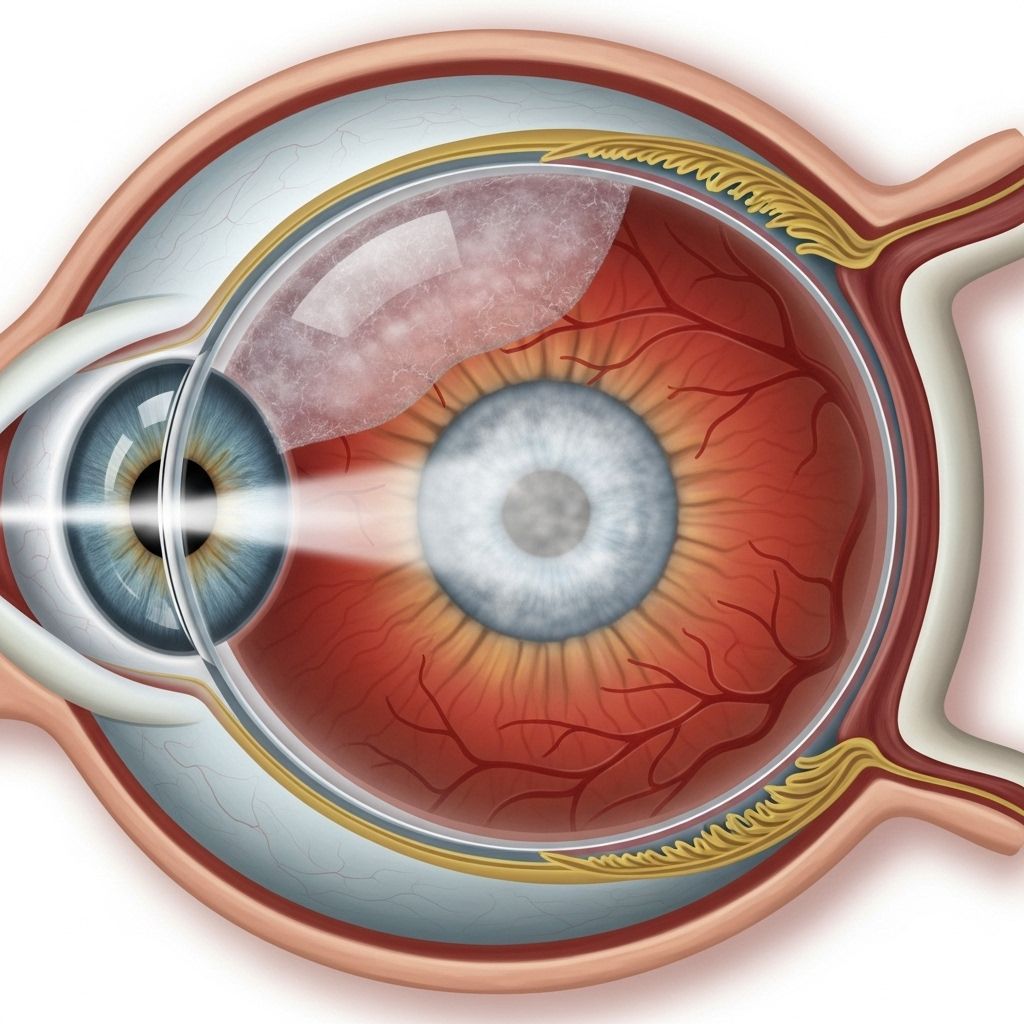
Secondary cataracts, also known as posterior capsule opacification (PCO), are a common complication following cataract surgery. While cataract surgery is a highly effective procedure to restore vision, some patients experience a recurrence of symptoms months or years after a successful operation. This article explains what secondary cataracts are, why they form, who is at risk, their typical symptoms, and how they are treated.
What Is a Secondary Cataract?
A secondary cataract is not a new cataract, nor does it mean the original cataract has “grown back.” Rather, it refers to the clouding of the posterior part of the lens capsule, which holds the artificial intraocular lens (IOL) implanted during cataract surgery. This clouding is the result of residual lens epithelial cells proliferating on the capsule after the removal of the eye’s natural lens.
- Secondary cataracts are also called posterior capsule opacification (PCO).
- They typically develop months or years after cataract surgery, though they may appear earlier in some cases.
- Up to 20-33% of patients who have undergone cataract surgery may experience this condition, making it a relatively common postoperative occurrence.
How Do Secondary Cataracts Develop?
During cataract surgery, the cloudy natural lens is replaced with an artificial lens. The clear membrane, or capsular bag, which surrounds the natural lens, is usually left in place to support the new IOL. In most cases, some lens epithelial cells that remain on the capsular bag survive the procedure and continue growing. Over time, these cells can transform and migrate across the posterior capsule, forming a thin, opaque, scar-like layer that interferes with light passing through the eye.
This process leads to a gradual decline in vision, mimicking cataract symptoms.
Key Steps in Development
- The capsular bag is retained to anchor the artificial lens during cataract surgery.
- Residual lens epithelial cells can remain on the capsule, undetected during surgery.
- These cells multiply and change, creating a thin, cloudy film on the posterior capsule.
- This film scatters light, reducing the amount that reaches the retina, and causes visual symptoms.
Symptoms of Secondary Cataract
Symptoms of a secondary cataract are often similar to those of the original cataract removed during surgical treatment. They can emerge weeks, months, or even years after surgery, and may worsen over time. Common symptoms include:
- Blurry or cloudy vision
- Double vision in the affected eye
- Sensitivity to light, especially increased glare or halos around lights
- Reduced brightness or fading colors
- Difficulty seeing well in low-light or dark environments
- Frequent changes in eyeglass prescription, such as increased farsightedness
- Seeing halos or foggy patches in the field of vision
These symptoms may result in a noticeable decline in vision, and in severe cases, vision loss can resemble the impairment experienced before the original cataract surgery.
Who Is at Risk for Secondary Cataracts?
While secondary cataracts can affect anyone who has had cataract surgery, certain factors may increase the likelihood:
- Younger patients (under 60) tend to develop secondary cataracts more frequently than older adults.
- History of glaucoma or retinal surgery can increase risk.
- Uveitis, an inflammatory condition of the eye’s middle layer (uvea), may predispose individuals to secondary cataract.
- The type and material of the intraocular lens (IOL) implanted might affect the risk to some extent.
- In general, there is no definitive way to predict who will develop a secondary cataract after cataract surgery.
What Causes a Secondary Cataract?
The primary cause of a secondary cataract is the proliferation of lens epithelial cells left behind during cataract surgery. Over time, these cells produce scar-like tissue on the posterior capsule behind the artificial lens. The risk factors above may make this process more likely in some individuals, but the exact reasons why it occurs in certain patients and not others remain unclear to ophthalmologists.
Diagnosis of Secondary Cataracts
Diagnosis involves a thorough eye examination by an ophthalmologist. If a person develops new visual disturbances following cataract surgery, especially blurred vision, glare, or halos, it is important to seek prompt medical advice. The typical diagnostic process includes:
- Reviewing the patient’s surgical history and visual symptoms
- Conducting a slit-lamp examination to assess the clarity of the lens capsule and the position of the IOL
- Ruling out other potential causes of vision loss
The visual impact of secondary cataracts can be measured using standard visual acuity tests and imaging techniques.
Treatment: The YAG Laser Capsulotomy
The standard and most effective treatment for secondary cataracts is the YAG laser capsulotomy. This is a quick, outpatient laser procedure designed to remove the opaque portion of the posterior capsule, allowing light to pass freely to the retina and restoring clear vision.
What Happens During the Procedure?
- Eyedrops are used to numb and dilate the eye.
- The patient sits at a laser device, similar to the exam lamp used in routine eye exams.
- The ophthalmologist uses the Nd:YAG laser to painlessly create a small opening in the cloudy capsule behind the IOL.
- The procedure takes only a few minutes per eye, and rarely requires an injectable anesthetic.
Aftercare and Recovery
- Patients may experience immediate improvement in vision, often within a day or two.
- A short course of anti-inflammatory or pressure-lowering eyedrops is usually prescribed for several days.
- Most individuals can resume normal activities quickly, although they may need to arrange transport home from the clinic.
Risks and Potential Complications
The YAG laser capsulotomy is considered very safe. However, as with any procedure, some risks exist:
- Transient eye pressure increases (usually short-lived)
- Potential for retinal detachment (rare)
- Possible inflammation or swelling
- Dislocation of the artificial lens (extremely rare)
Most patients experience little to no discomfort, and significant complications are rare when the procedure is performed by an experienced ophthalmologist.
Prevention and Outlook
There is currently no guaranteed way to prevent secondary cataracts after cataract surgery. While some newer IOL designs and materials may slightly reduce the incidence, individuals should remain vigilant for any returning visual symptoms after surgery, regardless of their IOL type.
- Secondary cataracts cannot be prevented by medication, lifestyle changes, or improved surgical technique alone.
- Regular follow-up appointments after cataract surgery are critical to detect and treat secondary cataracts early if they arise.
- Prognosis is excellent after YAG laser capsulotomy; most people regain clear vision quickly and with minimal risk of recurrence.
Secondary Cataract vs. Cataract Recurrence
| Feature | Secondary Cataract | True Cataract Recurrence |
|---|---|---|
| Location | Posterior capsule (behind the artificial lens) | Natural lens (already removed in surgery) |
| Cause | Scar-like tissue growth after cataract surgery | Original cataract cannot regrow |
| Treatment | YAG laser capsulotomy | N/A (does not occur) |
| Risk of Recurrence | Rare after laser treatment | N/A |
When to See a Doctor
It is important to contact an ophthalmologist promptly if you notice any of the following symptoms after cataract surgery:
- Blurring or clouding of vision that returns or worsens
- Problems with glare, halos, or fuzzy lights
- Sudden decrease in the ability to see or read clearly
- Any new or unexplained visual disturbances
Early intervention can restore vision quickly and help prevent complications.
Frequently Asked Questions (FAQs)
Can a cataract grow back after surgery?
No. The natural lens, which developed the original cataract, is completely removed during surgery. What some people call “cataract regrowth” is actually a secondary cataract or posterior capsule opacification. This is due to cell growth on the capsule behind the artificial lens.
How common are secondary cataracts?
Secondary cataracts are common, affecting up to one in three people who undergo cataract surgery. The risk is elevated in younger individuals and those with specific eye conditions like uveitis or who have had prior eye surgery.
Is YAG laser capsulotomy safe?
Yes. The YAG laser capsulotomy is a quick, highly effective, and safe outpatient procedure performed by ophthalmologists. Most patients benefit from significant vision improvement within days and experience minimal side effects.
Is there anything I can do to prevent a secondary cataract?
Currently, there is no proven method to prevent secondary cataracts. Regular follow-up with your eye doctor ensures early detection and prompt treatment should they occur.
How long does it take to recover vision after YAG laser capsulotomy?
Vision generally improves within a day or two after the procedure. A short course of anti-inflammatory eye drops is commonly used to optimize the healing process.
Key Takeaways
- Secondary cataracts (posterior capsule opacification) are a common, treatable complication after cataract surgery.
- Symptoms closely resemble the original cataract and can be distressing but are typically reversible.
- The YAG laser capsulotomy is an effective, quick, and safe solution, restoring clear vision for most patients.
- Regular eye check-ups after cataract surgery maximize your chances of early diagnosis and successful treatment if secondary cataracts develop.
References
- https://icrcat.com/en/eye-conditions/secondary-cataract/
- https://armadale-eye.com.au/can-you-have-cataract-surgery-twice/
- https://www.health.harvard.edu/diseases-and-conditions/are-you-at-risk-for-a-secondary-cataract
- https://resources.healthgrades.com/right-care/cataract-surgery/secondary-cataract
- https://my.clevelandclinic.org/health/diseases/24737-posterior-capsular-opacification
- https://www.healthline.com/health/eye-health/posterior-subcapsular-cataract
- https://www.medicalnewstoday.com/articles/can-cataracts-come-back-after-surgery
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3130924/
- https://www.bravenhealth.com/blog/detail/what-are-secondary-cataracts
Read full bio of Sneha Tete












