Secondary Acute Myeloid Leukemia: Causes, Risks, and Treatments
Comprehensive guide on secondary acute myeloid leukemia, including causes, risk factors, symptoms, treatment, and prognosis.
Secondary Acute Myeloid Leukemia: Causes, Risks, Symptoms, and Treatments
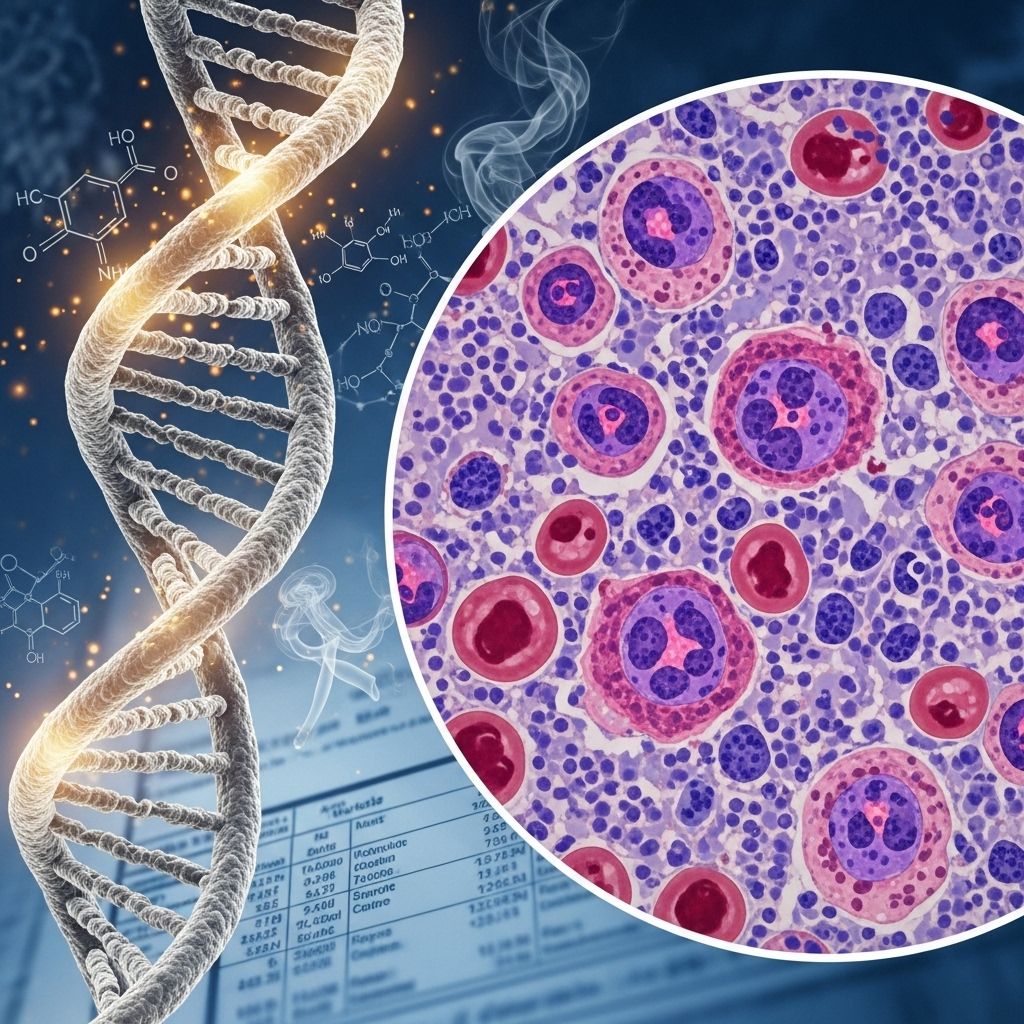
Secondary acute myeloid leukemia (AML) is a complex and aggressive form of blood cancer that often arises following previous cancer treatment or as a progression from existing blood or bone marrow disorders. This article provides a thorough overview of secondary AML, exploring its causes, risk factors, symptoms, diagnostic process, treatment options, prognosis, as well as frequently asked questions to help patients and caregivers better understand this challenging disease.
Overview of Secondary Acute Myeloid Leukemia
Acute myeloid leukemia is a cancer affecting the myeloid line of blood cells, causing a rapid growth of abnormal cells in the bone marrow, which impairs the production of normal blood cells. Secondary AML specifically refers to cases that develop:
- After prior treatment for another cancer (chemotherapy or radiation), known as therapy-related AML (t-AML)
- As a progression of pre-existing blood or bone marrow disorders, primarily myelodysplastic syndromes and chronic myeloproliferative disorders
Secondary AML accounts for approximately 20% to 30% of all AML cases. It is generally associated with a more challenging outlook compared to primary or de novo AML, which occurs without such history.
Causes of Secondary AML
Secondary AML develops when genetic changes take place in immature myeloid blood cells as a result of:
- Chemotherapy or Radiation Therapy: Cancer treatment can induce DNA damage in healthy blood-forming cells, increasing the risk of developing secondary leukemia later.
- Preexisting Blood and Bone Marrow Disorders:
- Aplastic anemia — a rare disorder where the bone marrow fails to produce enough new blood cells.
- Myelodysplastic syndromes (MDS) — a group of disorders in which the bone marrow produces malformed or insufficient blood cells.
- Chronic myeloproliferative syndromes — characterized by the overproduction of one or more types of blood cells.
- Myelodysplastic/myeloproliferative overlap syndromes — exhibiting features of both myelodysplastic and myeloproliferative disorders.
Therapy-related AML (t-AML), specifically resulting from previous cancer therapy, makes up around 5% to 10% of all AML cases.
Who Is at Risk?
The following populations are at increased risk of developing secondary AML:
- Individuals with a history of blood disorders such as MDS, aplastic anemia, or myeloproliferative syndromes
- Cancer survivors previously treated with high-dose chemotherapy or radiation
- People with inherited genetic predispositions for hematologic malignancies
Examples of conditions that may progress to secondary AML include:
- Aplastic anemia: Reduced production of all types of blood cells, increasing risk through impaired marrow function.
- Myelodysplastic syndromes (MDS): Pre-leukemic disorders that can transform into AML, especially when characteristic chromosomal abnormalities are present.
- Chronic myeloproliferative disorders: Overproduction of blood cells leads to genetic instability over time.
Symptoms of Secondary AML
The clinical presentation of secondary AML is largely indistinguishable from primary AML. Symptoms typically result from anemia, leukopenia (low white blood cells), and thrombocytopenia (low platelets):
- Paleness and fatigue
- Shortness of breath
- Unexplained weight loss
- Frequent infections
- Fever and chills
- Night sweats
- Easy bruising and unusual bleeding (including frequent nosebleeds)
- Petechiae: Flat red or purple spots on the skin
- Bone or joint pain
- Abdominal discomfort
- Swollen lymph nodes (notably in the neck, armpits, or groin)
Potential Complications
Complications arising from secondary AML often mirror those seen in other types but can be aggravated by prior treatment or underlying blood disorders. Notable complications include:
- Life-threatening infections due to weakened immunity
- Severe bleeding episodes caused by low platelet counts
- Anemia-induced fatigue and organ stress
- Rapid disease progression and refractory disease to standard treatment
When to Seek Medical Help
It is crucial for individuals at increased risk or those experiencing symptoms of AML to seek immediate medical assessment if they notice:
- Persistent or unexplained fevers or infections
- Ongoing or severe bleeding/bruising
- Shortness of breath or chest pain
- Significant, unexplained fatigue
Early recognition and prompt diagnosis can be vital for optimizing treatment outcomes.
Diagnosing Secondary AML
Diagnosis is based on a combination of laboratory and clinical assessments to distinguish secondary AML from primary AML and underlying hematologic disorders. Common diagnostic steps include:
- Physical examination for signs such as pallor, petechiae, and lymphadenopathy
- Complete blood count (CBC): To check for anemia, leukopenia, and thrombocytopenia
- Bone marrow aspiration and biopsy: Confirms the diagnosis by identifying a high percentage of immature myeloid cells (myeloblasts) in the marrow or blood
- Cytogenetic and molecular testing: Identifies chromosomal abnormalities relevant to subtype and prognosis
Specific genetic markers and the presence of preceding blood disorders are crucial parts of the diagnostic workup.
Treatment Options for Secondary AML
Due to its aggressive biology and resistance to treatment, secondary AML often requires an intensive approach. Main treatment strategies include:
- Chemotherapy: Multi-agent regimens aimed at inducing remission. The chemotherapy protocol Vyxeos (daunorubicin and cytarabine in a fixed combination) is currently the standard for fit patients, approved for secondary AML since 2017. It is administered intravenously through 90-minute infusions.
- Hematopoietic Stem Cell Transplant: Also called allogeneic stem cell transplant, this involves the infusion of healthy donor stem cells to restore normal blood production. It is generally pursued in patients who respond to initial chemotherapy and can tolerate the procedure.
- Targeted Therapy: Certain drugs target specific genetic mutations or pathways in AML cells. Examples include Janus kinase (JAK) inhibitors and venetoclax.
- Supportive Care: Includes blood transfusions, infection management, and medications to control symptoms and complications.
Therapies are tailored to each patient based on age, overall health, previous treatments, genetic findings, and comorbidities.
Key Treatment Approaches: Comparative Table
| Treatment Type | Purpose | Main Characteristics |
|---|---|---|
| Vyxeos Chemotherapy | Induce remission | Daunorubicin & Cytarabine; IV regimen; standard in secondary AML |
| Stem Cell Transplant | Curative potential | Donor stem cells administered to repopulate blood system |
| Targeted Therapy | Target mutations | e.g., JAK inhibitors, venetoclax; used based on genetic findings |
| Supportive Care | Manage complications | Blood transfusions, infection treatment, symptom relief |
Prognosis and Outlook
The overall prognosis for individuals with secondary AML is generally less favorable compared to those with primary AML. The five-year overall survival rate is under 30%. Key prognostic factors include:
- Genetic mutations: Simultaneous mutations such as the inversion of chromosome 16 or the translocation of chromosomes 15 and 17 are associated with better outcomes.
- Health status at diagnosis: Presence of additional health issues or ongoing complications from prior treatments can impact survival prospects.
- Response to initial therapies: Achieving remission with first-line therapy is a critical determinant.
Is Secondary AML Preventable?
While it may not be possible to completely prevent the onset of secondary AML, especially in patients who require life-saving cancer chemotherapy or who have a primary blood disorder, certain steps may lower risk:
- Close monitoring of patients with myelodysplastic syndromes and other pre-leukemic conditions
- Judicious use of chemotherapy and radiation therapy, weighing long-term risks
- Prompt reporting and evaluation of concerning blood count abnormalities or new symptoms
For cancer survivors and patients with blood disorders, regular medical follow-up and communication with healthcare providers remain essential.
Frequently Asked Questions (FAQs)
What is the difference between secondary and primary AML?
Primary AML develops without a prior history of blood disorders or cancer treatment. Secondary AML arises either after previous cancer therapy or due to the transformation of preexisting blood or bone marrow disorders.
How is secondary AML diagnosed?
Diagnosis involves clinical evaluation, complete blood counts, examination of bone marrow samples, and genetic/cytogenetic testing to confirm the presence of AML and distinguish it as secondary or therapy-related.
Are outcomes worse for secondary AML?
Yes. Secondary AML typically has a lower response rate to standard treatment and a lower five-year survival rate, emphasizing the need for improved and tailored therapeutic strategies.
Can secondary AML be cured?
Cure is difficult but not impossible, especially for those who achieve remission and undergo stem cell transplant. Prognosis depends on several individual factors, including underlying genetic markers.
Is there a way to screen for secondary AML?
No standard screening exists, but regular monitoring for blood abnormalities in at-risk individuals (such as cancer survivors or those with MDS) allows for early detection and prompt intervention.
What is the most effective treatment for secondary AML?
The combination chemotherapy regimen Vyxeos, often followed by a stem cell transplant for eligible patients, currently represents the standard of care for fit individuals.
Summary
Secondary acute myeloid leukemia is a rare but serious cancer with a strong association to prior cancer treatments or underlying blood disorders. It is typically characterized by aggressive disease progression and a more challenging outlook than primary AML. Early recognition, comprehensive diagnostic evaluation, and timely intervention are essential. Research continues to seek better treatment algorithms and improved outcomes for those affected by this condition.
References
- https://www.healthline.com/health/leukemia/secondary-acute-myeloid-leukemia
- https://www.medicalnewstoday.com/articles/secondary-aml
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11317385/
- https://ascopubs.org/doi/10.1200/EDBK_199519
- https://www.healthline.com/health/aml/acute-myeloid-leukemia-diet
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9820930/
- https://www.healthline.com/health/video/break-it-down-anemia-in-mds-bt
- https://www.medicalnewstoday.com/articles/215538
Read full bio of Sneha Tete












