Salivary Gland Infection (Sialadenitis): Symptoms, Causes, Diagnosis, and Treatment
Comprehensive overview of sialadenitis covering symptoms, causes, diagnosis, risk factors, prevention, and modern treatment strategies.
Salivary Gland Infection (Sialadenitis)
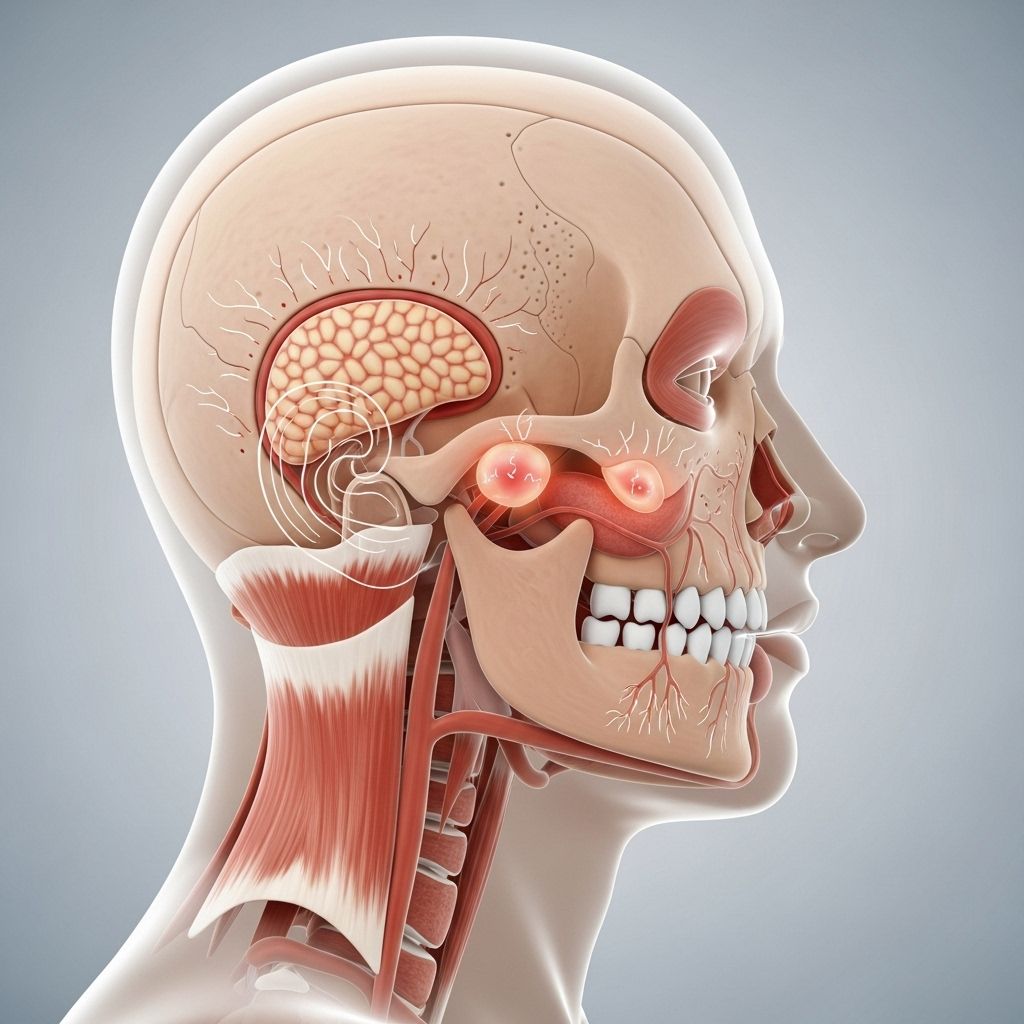
Sialadenitis, a term describing inflammation and infection of the salivary glands, is a common clinical condition that can lead to significant discomfort and, in rare cases, serious complications. The major salivary glands affected include the parotid, submandibular, and sublingual glands. Sialadenitis can occur in any age group but is most often seen in older adults and individuals with certain underlying medical conditions.
Overview
- Sialadenitis is an infection of one or more major salivary glands, most commonly the parotid and submandibular glands.
- The condition can be acute or chronic, bacterial or viral, and may result from an obstruction, diminished salivary flow, autoimmune disease, or post-radiation changes.
Types of Salivary Glands and Their Functions
The human body has three pairs of major salivary glands and several minor glands, all of which are essential for oral health:
- Parotid Glands: The largest salivary glands, located in front of the ears.
- Submandibular Glands: Situated beneath the jaw.
- Sublingual Glands: Located under the tongue.
These glands produce saliva, which aids in digestion, maintains oral hygiene, and keeps the mouth moist.
Causes of Sialadenitis
Sialadenitis is most frequently caused by bacterial infection, but other factors also play a role:
- Bacterial Infection: Most commonly Staphylococcus aureus. Other bacteria include streptococci, coliforms, anaerobic bacteria, and, rarely, actinomyces.
- Viral Causes: Mumps, cytomegalovirus, and human immunodeficiency virus (HIV) can infect salivary glands.
- Obstruction: Blockage by a salivary stone (sialolithiasis), ductal stricture, or external compression (e.g., poorly fitted dentures).
- Autoimmune Disorders: Sjögren syndrome and IgG4-related disease.
- Post-Radiation Changes: Radiation treatment for head, neck, or thyroid cancer may damage salivary tissue, leading to inflammation.
- Drug-Induced: Certain medications are associated with reduced saliva flow and increased risk of infection (e.g., anticholinergics, clozapine).
- Idiopathic and Chronic Conditions: Sometimes, the cause remains unknown; chronic sclerosing sialadenitis may mimic tumors.
Risk Factors for Sialadenitis
Several factors increase the risk of developing salivary gland infections:
- Older age and chronic illnesses, especially those resulting in dry mouth (xerostomia).
- Dehydration and reduced oral intake.
- Poor oral hygiene, including dental infections.
- Recent surgery, especially of the head and neck.
- Use of medications that reduce saliva (e.g., antihistamines, antidepressants).
- Autoimmune disease history.
- History of radiation therapy to the oral cavity, neck, or thyroid gland.
- Sialolithiasis (presence of salivary duct stones).
- Children: Juvenile recurrent parotitis (usually ages 4 to 6); often resolves by puberty.
Symptoms of Salivary Gland Infection
The clinical presentation varies depending on the severity and duration of the infection:
- Pain and swelling over the affected gland; it may be unilateral or bilateral.
- Tenderness and firmness of the gland.
- Redness and edema of the overlying skin.
- Fever and chills may be present in acute cases.
- Pus may drain into the mouth, especially when the gland is compressed; this should be cultured for diagnosis.
- Difficulty opening the mouth (trismus), chewing, or swallowing.
- Dry mouth or altered taste.
- Malaise or general feeling of illness.
- Abscess formation may occur—focal enlargement and increased pain.
- Chronic cases may have intermittent, painless swelling, often associated with autoimmune disease.
Complications of Sialadenitis
If not properly treated, sialadenitis can lead to:
- Abscess formation requiring surgical intervention.
- Spread of infection to surrounding tissues or bloodstream (sepsis).
- Airway compromise from glandular swelling.
- Chronic pain and gland dysfunction.
- Rarely, fistula formation (an abnormal passageway from the gland to the skin).
Diagnosis of Sialadenitis
Clinical evaluation is essential, but imaging and laboratory studies may be required to confirm the diagnosis and guide management.
- Physical Examination: Examination for swelling, tenderness, firmness, skin changes, pus expression.
- Imaging:
- CT Scan: Detects inflammation, abscesses, and obstructing stones.
- Ultrasound: Visualizes gland structure, stones, and fluid collections.
- MRI: May identify abscesses but may miss small stones.
- Pus Culture and Gram Stain: If pus is expressed, laboratory testing helps identify causative organisms and guides antibiotic therapy.
- Blood Tests: May show elevated white blood cell count (WBC) if infection is severe.
- Biopsy: Used to rule out tumors or to confirm chronic sclerosing sialadenitis in ambiguous cases.
Treatment Options for Sialadenitis
Management depends on the underlying cause, severity, and whether the condition is acute or chronic.
- Antibiotics: Mainstay of treatment for acute bacterial sialadenitis; empiric therapy targets Staphylococcus aureus (e.g., dicloxacillin, cephalosporin, or clindamycin), but may be adjusted based on culture results. Methicillin-resistant S. aureus (MRSA) may require vancomycin.
- Pain Management: Analgesics (e.g., acetaminophen or nonsteroidal anti-inflammatory drugs) relieve pain and inflammation.
- Local Measures:
- Hydration: Maintains salivary flow and promotes gland function.
- Sialogogues: Substances that stimulate saliva production, e.g., lemon drops, sour candy.
- Warm Compresses: Reduce pain and swelling.
- Gland Massage: Encourages drainage and relieves ductal obstruction.
- Oral Hygiene: Antimicrobial mouth rinses (e.g., chlorhexidine) to reduce bacterial burden and promote oral health.
- Surgical Intervention: Indicated for abscess drainage, persistent stones (sialolithiasis), or in cases of chronic, relapsing infection; may involve sialendoscopy or gland excision.
- Management of Underlying Conditions: Treatment of autoimmune disease, radiation side effects, or medication review may be necessary in chronic cases.
- Corticosteroid Therapy: Rarely, used for severe soft tissue swelling when infection is controlled.
Prevention Strategies
- Maintain good oral hygiene and regular dental checkups.
- Avoid dehydration by drinking adequate fluids.
- Identify and address medications that may decrease saliva production.
- Treat or manage underlying conditions such as autoimmune disease or chronic illnesses.
- Regularly massage the gland if prone to recurrent episodes, as recommended by healthcare professionals.
Prognosis
Most cases of acute sialadenitis resolve completely with appropriate treatment. Chronic or recurrent infection may require surgical intervention, and autoimmune-mediated or post-radiation cases may have a variable course. Complications such as abscess or airway compromise require urgent medical evaluation.
Frequently Asked Questions (FAQs)
Q: What are the common signs of sialadenitis?
A: Common signs include pain, swelling, redness, and sometimes pus draining from the duct. Fever and difficulty swallowing may also occur.
Q: Is sialadenitis contagious?
A: Bacterial sialadenitis is not generally contagious, but viral causes like mumps can be transmitted, especially among unvaccinated individuals.
Q: Which antibiotics are used to treat sialadenitis?
A: Empiric antibiotics cover Staphylococcus aureus (e.g., dicloxacillin, cephalosporins, clindamycin). For MRSA, vancomycin may be needed. Therapy is tailored to culture results.
Q: Can sialadenitis become a chronic condition?
A: Yes, chronic sialadenitis can occur with repeated infection, obstruction, or underlying autoimmune disorders. It may require surgical intervention or specialized medical therapy.
Q: How can I prevent salivary gland infection?
A: Prevention includes hydration, good oral hygiene, regular dental visits, avoiding medications that cause dry mouth when possible, and prompt management of underlying health conditions.
Table: Comparison of Major Salivary Gland Infections
| Feature | Parotid Gland | Submandibular Gland | Sublingual Gland |
|---|---|---|---|
| Prevalence | Most common in adults | Common with duct obstruction | Rare |
| Typical Symptoms | Painful swelling, fever, pus | Pain, swelling, stone formation | Pain, swelling |
| Main Causes | Bacterial, viral, autoimmune, post-radiation | Stone obstruction, infection | Infection |
| Treatment Approach | Antibiotics, drainage, surgery if needed | Antibiotics, removal of stones | Antibiotics |
When to Contact a Healthcare Provider
- If you notice persistent pain and swelling in the jaw, neck, or mouth.
- When you develop fever, chills, or pus drainage from the mouth.
- If symptoms worsen, fail to improve with self-care, or interfere with eating and drinking.
- Whenever you experience difficulty breathing or swallowing.
Key Takeaways
- Sialadenitis is a multifactorial inflammation and infection of the salivary glands that requires early recognition and appropriate management.
- Acute bacterial episodes are usually rapidly progressive and visible; chronic cases might be harder to diagnose and need specialist evaluation.
- Prevention and timely medical intervention are essential for optimal outcomes and to avoid complications.
Related Topics
- Sialolithiasis (Salivary stone disease)
- Autoimmune salivary gland disorders (e.g., Sjögren syndrome)
- Oral health and dental hygiene
- Head and neck infections
- Post-radiation complications
References
- https://www.merckmanuals.com/professional/ear-nose-and-throat-disorders/oral-and-pharyngeal-disorders/sialadenitis
- https://www.ncbi.nlm.nih.gov/books/NBK562211/
- https://bestpractice.bmj.com/topics/en-us/1038
- https://my.clevelandclinic.org/health/diseases/15749-sialadenitis-swollen-salivary-gland
- https://rarediseases.org/rare-diseases/sialadenitis/
- https://www.enthealth.org/conditions/sialadenitis/
- https://my.clevelandclinic.org/health/diseases/24344-sialolithiasis
Read full bio of medha deb












