Ruptured Eye: Causes, Symptoms, Treatment, and Recovery
Learn about ruptured eye injuries—their causes, symptoms, treatment, and long-term outlook for eye health.
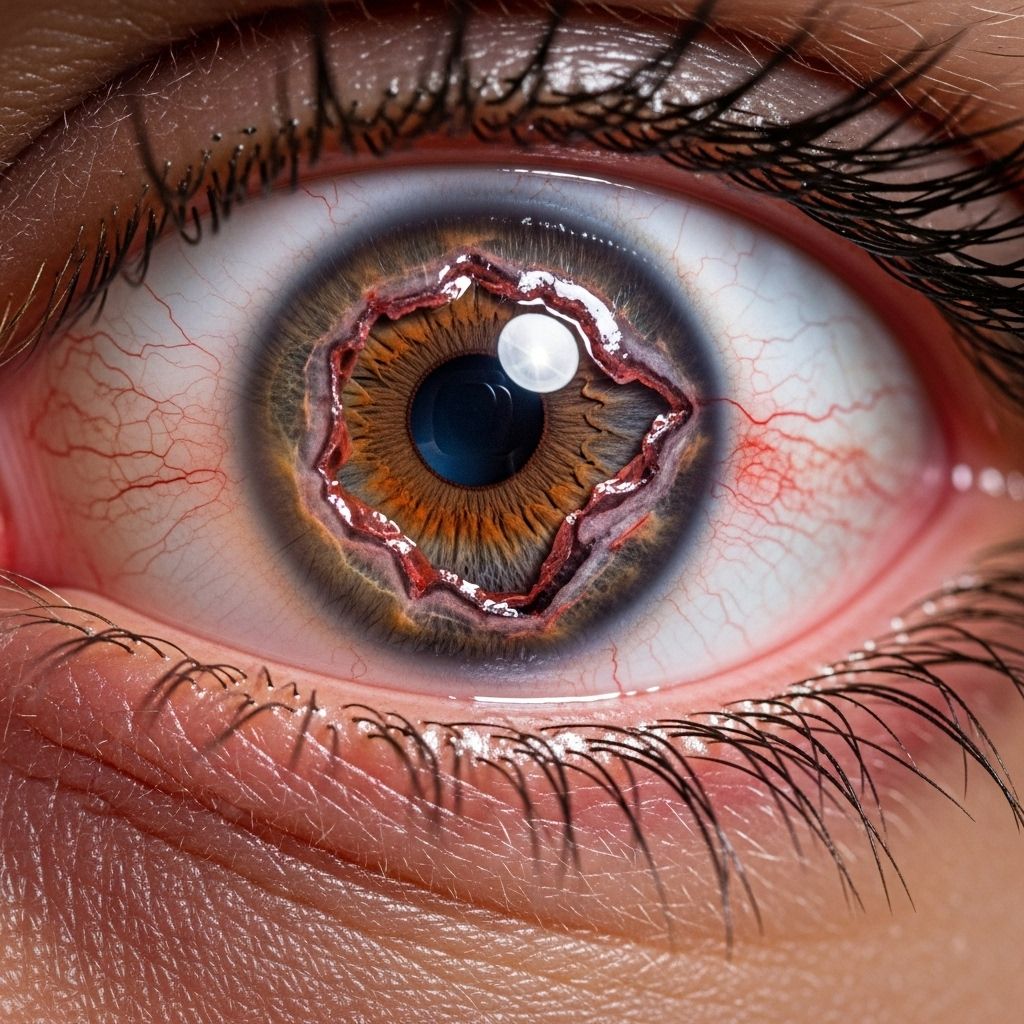
A ruptured eye or globe rupture is a severe eye injury that occurs when the outer membranes of the eyeball (the sclera and cornea) are disrupted, compromising the integrity of the eye. This is a medical emergency that requires immediate attention to prevent permanent vision loss and further complications.
Understanding a Ruptured Eye
The eye is filled with fluid, and its walls consist of tough tissue called the sclera (white part) and the transparent cornea. When a substantial force—often from trauma—hits the eye, the pressure inside can increase so much that the wall of the eye gives way, resulting in a rupture. This condition is different from superficial injuries such as corneal abrasions or eyelid cuts, as it involves a break in the actual globe housing the delicate internal structures responsible for vision.
Key Facts about Ruptured Eye Injuries
- Etiology: Typically caused by blunt or penetrating trauma.
- Urgency: Ruptured eyes require immediate emergency medical care to optimize outcomes and preserve vision.
- Prognosis: The degree of visual recovery depends on the site and extent of the injury, promptness of intervention, and other factors.
What Causes a Ruptured Eye?
Most cases of ruptured eyes are the result of significant trauma, either blunt or penetrating. Common causes include:
- Blunt trauma: Frequently due to sports injuries, falls, motor vehicle accidents, or assaults. A forceful blow increases internal pressure, rupturing the eyewall.
- Penetrating injuries: Sharp objects (e.g., metal shards, knives, glass) directly puncture the eye.
- Occupational hazards: Industrial work involving high-speed tools, projectiles, or chemicals exposes workers to risk.
- Household accidents: Mishaps involving bungee cords, fireworks, or falling objects.
Vulnerable areas: The eye is most likely to rupture at points where the sclera is thinnest, such as near muscle attachments or previous surgical incisions.
Signs and Symptoms of a Ruptured Eye
Recognizing the symptoms early is crucial as prompt action can make the difference between saving and losing vision. Symptoms include:
- Severe eye pain or sudden onset of discomfort
- Decreased or blurred vision
- Change in the shape of the pupil, often teardrop-shaped or pointing towards the injury
- Visible wound or laceration of the eye
- Bleeding in or around the eye
- Loss of eye contents – jelly-like substance (vitreous), lens, or iris extrusion
- Subconjunctival hemorrhage that is extensive or bullous (blood pooling under the clear covering of the eye)
- Loss of red reflex (the light reflex seen in the pupil)
- Protrusion of eye tissue
- Complete or partial vision loss
- Hypotony (eye feels soft to the touch, but do not touch if rupture is suspected)
Some symptoms, especially in children or those with multiple injuries, can be subtle. Always assume an eye is ruptured after severe facial or eye trauma until proven otherwise by a medical professional.
When to Seek Emergency Care
A ruptured eye is a true ocular emergency. Get immediate medical attention if you experience:
- Any direct injury to the eye with possible penetration
- Sudden loss of vision
- Severe ocular pain after trauma
- Bleeding from the eye (not just eyelid)
- Visible globe deformity
Do not:
- Attempt to wash the eye or remove any object embedded in the eye
- Apply pressure to the eye
- Use eyedrops unless directed by a medical provider
- Try to open an eyelid that is tightly shut
Cover the eye gently with a shield or the bottom of a plastic cup and seek emergency care promptly.
How Is a Ruptured Eye Diagnosed?
Diagnosis of a ruptured globe requires careful evaluation by an ophthalmologist or emergency medicine doctor. The process includes:
- History: Inquiry about the mechanism of injury, symptoms, and any prior eye conditions or surgeries.
- Physical Examination: Inspection for external injuries, changes in globe shape, pupil deformity, visible lacerations, loss of ocular tissue, or bulging under conjunctiva. Careful checking without pressing on the globe.
- Visual Acuity Testing: Assessing the clarity of vision, if possible, helps guide treatment and prognosis.
- Slit Lamp Examination: A specialized microscope allows a detailed look at the anterior parts of the eye. Smaller wounds or occult ruptures are sometimes identified this way.
- Additional Observations: Look for chemosis (swelling), hypotony, vitreous loss, extensive hemorrhage, and change in anterior chamber depth.
Imaging studies (such as CT scans of the orbits) may be ordered to detect foreign bodies, bone fractures, or extent of internal injury—particularly if the view of the internal eye structures is obstructed.
Common Signs of Globe Rupture on Exam
- Thick subconjunctival hemorrhage (especially if extends 360° around the cornea)
- Scleral step-off or irregular contour (palpable notch or discontinuity)
- Peaked or irregularly shaped pupil pointing to injury site
- Loss of eye pressure (hypotony)
- Visible uveal or intraocular tissue prolapse
- Vitreous or lens visible in the wound
- Loss of red reflex, indicating intraocular hemorrhage
Note: Examination is often limited to avoid further damage or tissue extrusion.
Treatment: What Happens After a Ruptured Eye?
Immediate surgical intervention is required for any suspected or confirmed globe rupture. Treatment steps typically include:
- Immediate Protection: Shielding the eye with a rigid protective device to prevent further injury.
- Tetanus prophylaxis: Ensuring tetanus immunization status is up-to-date.
- Antibiotics: Intravenous broad-spectrum antibiotics are often given to reduce the risk of infection (endophthalmitis).
- Pain management: Analgesics and antiemetics to prevent straining (which could increase intraocular pressure).
- Surgical Repair: Performed by an ophthalmologist, repairing the outer eye wall under general anesthesia. The goals are to restore globe integrity, reposition any prolapsed tissue, and close the laceration. Intraocular foreign bodies may be removed if present.
- Observation and further surgery: Additional procedures may be needed for complications such as retinal detachment or cataract.
Hospitalization is common to monitor for infection and other complications.
Pre- and Post-Surgery Care
Before Surgery
- Do not eat, drink, or administer any drops unless instructed by a physician.
- Strictly avoid any pressure on the eye.
- Avoid coughing, sneezing, or vomiting (which increase intraocular pressure).
After Surgery
- Follow all post-operative instructions regarding medications, eye shields, and activity level.
- Avoid heavy lifting or activities that might strain the eye.
- Attend all follow-up appointments for monitoring healing, intraocular pressure, and vision.
- Promptly report any sudden vision change, pain, or discharge to your ophthalmologist.
Recovery and Prognosis
The outlook after a ruptured eye depends on several factors:
- Extent and location of the injury: Posterior (back of eye) ruptures, involvement of the optic nerve, or severe retinal injury have poorer outcomes.
- Time to intervention: Earlier surgical repair within hours generally gives the best chances.
- Presence of infection: Endophthalmitis (intraocular infection) significantly worsens visual outcomes.
- Other complications: Retinal detachment, traumatic cataract, and persistent hypotony can occur.
Visual recovery varies widely: some individuals regain useful vision, while others sustain permanent vision loss or, in rare cases, require removal of the eye. Long-term complications such as glaucoma, cataracts, or retinal detachment may need additional management.
Complications: What Can Go Wrong?
Potential complications following a ruptured globe include:
- Endophthalmitis: A sight-threatening infection inside the eye
- Sympathetic ophthalmia: Immune reaction causing inflammation in both eyes
- Retinal detachment: Separation of the retina from its underlying support tissue
- Cataract formation: Clouding of the lens, sometimes after trauma or surgery
- Persistent vision loss or blindness
- Chronic pain or disfigurement
- Secondary glaucoma: Elevated intraocular pressure causing optic nerve damage
Close and regular follow-up with an ophthalmology specialist is vital for detecting and managing complications.
How Can You Prevent Eye Rupture and Related Injuries?
- Wear safety goggles or face shields during sports, construction, or work with hazardous materials.
- Store sharp or projective objects safely away from children.
- Take precautions when using tools, chemicals, or fireworks.
- Implement home safety measures to prevent falls or accidents.
Public education and adherence to safety protocols can significantly reduce the incidence of vision-threatening eye injuries.
Frequently Asked Questions (FAQs)
What is a ruptured eye or globe rupture?
A ruptured eye (globe rupture) is an emergency injury where the eyeball’s tough outer coating is disrupted, causing its internal fluids and tissues to potentially leak out, threatening vision.
How is a ruptured eye different from a scratched eye?
A scratched eye (corneal abrasion) affects only the outermost layer (cornea). A ruptured eye involves a deeper, full-thickness wound that breaches the wall of the eyeball, requiring urgent surgery.
What should I do if I suspect an eye is ruptured?
- Do not touch, press, or rinse the eye.
- Cover the eye with a rigid shield (not cloth or gauze).
- Seek emergency medical care—go directly to the ER or call emergency services.
How is vision affected after a ruptured eye?
Visual outcomes range greatly. Some regain partial vision after prompt care; others may face permanent visual impairment or blindness, depending on injury severity and complications.
What are long-term risks after a ruptured globe injury?
- Cataract formation
- Secondary glaucoma
- Retinal detachment
- Chronic pain or cosmetic issues
- Recurrent infections
Summary Table: Ruptured Eye (Globe Rupture) Overview
| Aspect | Details |
|---|---|
| Primary Causes | Blunt trauma, penetrating injury, falls, sports injuries, accidents with tools/objects |
| Key Symptoms | Eye pain, sudden vision loss, open wound, peaked pupil, subconjunctival hemorrhage, visible tissue extrusion |
| Immediate Actions | Do not touch or press the eye; shield and seek emergency care |
| Diagnosis | History, exam, slit lamp, imaging (CT) |
| Treatment | Surgical repair, antibiotics, tetanus prophylaxis, hospitalization |
| Prognosis | Varies by injury severity, location, complications, and timeliness of treatment |
| Prevention | Eye protection, safety education, workplace/household hazard controls |
Conclusion
A ruptured eye (globe rupture) is a sight-threatening emergency that demands immediate medical attention. Understanding the signs, taking quick and proper action, and getting expert care can improve your chances of preserving vision and preventing devastating complications. Early recognition, safety awareness, and prevention are key to reducing the impact of these serious eye injuries.
References
- https://psnet.ahrq.gov/web-mm/missing-point-eye-injury
- https://eyewiki.org/Ruptured_Globe
- https://www.ncbi.nlm.nih.gov/books/NBK470379/
- https://www.healthline.com/health/eye-health/popped-blood-vessel-in-eye
- https://www.ncbi.nlm.nih.gov/books/NBK551637/
- https://24hrer.com/eye-injuries-when-to-go-to-the-er/
- https://www.nhs.uk/conditions/
- https://www.uc.edu/news/articles/legacy/healthnews/2005/11/uc-health-line–brain-aneurysm-can-masquerade-as-flu.html
Read full bio of Sneha Tete












