Understanding the Risk Factors of Diabetic Retinopathy
Explore how diabetes, lifestyle, and medical factors elevate your risk and learn proven ways to protect your vision.
Risk Factors of Diabetic Retinopathy
Diabetic retinopathy is a serious complication of diabetes that affects the eyes and, left unmanaged, can lead to vision loss or blindness. Understanding the risk factors for diabetic retinopathy can empower individuals with diabetes—and those who care for them—to make informed decisions to protect their eyesight.
What Is Diabetic Retinopathy?
Diabetic retinopathy is a progressive eye disease caused by damage to the blood vessels of the retina due to chronic high blood sugar associated with diabetes. Over time, this damage may lead to impaired vision or blindness, making early identification of risk factors and preventive care essential.
Core Risk Factors for Diabetic Retinopathy
Everyone with diabetes is at some risk of developing diabetic retinopathy, but the risk level is influenced by several key factors:
- Duration of Diabetes: The longer a person has diabetes, the higher their risk for diabetic retinopathy.
- Poor Blood Sugar Control: Consistently high blood glucose levels accelerate damage to the retina.
- High Blood Pressure: Hypertension increases pressure on retinal blood vessels, compounding damage.
- High Cholesterol and Triglycerides: Raised lipid levels can worsen blood vessel damage and increase the risk of retinopathy.
- Kidney Disease: Kidney complications from diabetes (nephropathy) are often linked to a greater eye disease risk.
- Pregnancy: Pregnancy can worsen diabetic retinopathy or trigger its onset, especially in women with preexisting diabetes.
- Tobacco Use: Smoking increases blood vessel damage and impairs healing.
- Ethnicity: Certain groups—including Black, Latino, and Native American populations—have higher risks of developing diabetic retinopathy.
- Obesity: Excess body weight is associated with poorer blood sugar and blood pressure control, raising risk.
How Diabetes Duration Affects Eye Health
One of the strongest predictors of diabetic retinopathy is the length of time a person has had diabetes. Even with careful management, the risk increases every year after diagnosis, especially after 10 to 20 years with the condition.
- People with type 1 diabetes often develop signs of retinopathy within five years of diagnosis and see increasing risk over decades.
- Those with type 2 diabetes may already have retinopathy at diagnosis because high blood sugar can go unnoticed for years.
Blood Sugar Control: The Central Factor
Maintaining stable and normal blood glucose levels is the most critical modifiable factor for lowering risk. Elevated blood glucose damages tiny blood vessels, including those supplying the retina. Persistent hyperglycemia makes the retina more susceptible to swelling, leakage, and abnormal new vessel growth.
- People who keep their HbA1c (three-month average blood glucose) below 7% generally have lower rates of retinopathy.
- Sudden large drops in blood sugar can also impact the retina, so gradual improvements are recommended.
Table: Impact of Risk Factors on Diabetic Retinopathy
| Risk Factor | Increased Relative Risk | Can Be Modified? |
|---|---|---|
| Duration of Diabetes | Significant over time | No |
| Poor Blood Sugar Control | Very High | Yes |
| High Blood Pressure | Moderate to High | Yes |
| High Cholesterol/Triglycerides | Moderate | Yes |
| Tobacco Use | Moderate | Yes |
| Pregnancy | Variable (especially if preexisting diabetes) | Partially |
The Role of Blood Pressure and Cholesterol
High blood pressure and cholesterol can both worsen the retinal damage inflicted by high blood glucose. These cardiovascular risk factors make blood vessels more fragile and likely to leak, which can speed the progression of retinopathy and lead to macular edema—a major cause of vision loss.
- Management of both hypertension and high cholesterol is a foundation of modern diabetes care.
- Lifestyle changes and, when necessary, medication are often required to control these factors.
Other Factors that Increase Risk
- Kidney Disease: Kidney impairment is associated with poor blood sugar control and the overall progression of microvascular complications like retinopathy.
- Pregnancy: Women with diabetes are carefully monitored during pregnancy, as hormonal changes can accelerate eye disease.
- Tobacco Use: Smoking worsens vascular damage and inflammation throughout the body, including the retina.
- Obesity: Obesity is linked to increased insulin resistance, higher blood pressure, and worse cholesterol numbers—all compounding risks for retinopathy.
- Ethnic background: Black, Latino, and Native American individuals with diabetes are more susceptible, which may reflect a mix of genetic, socioeconomic, and healthcare access factors.
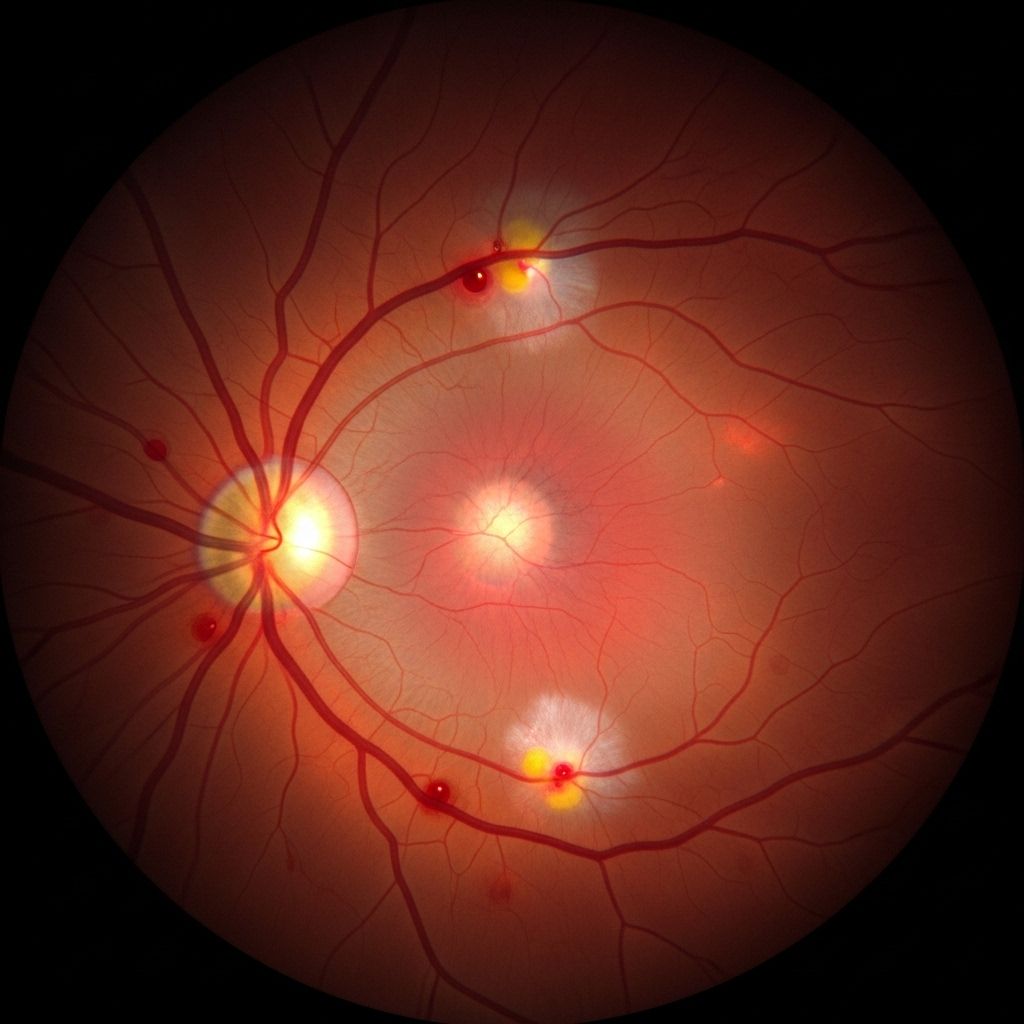
Types of Diabetic Retinopathy
Understanding the types and stages of diabetic retinopathy helps in assessing how risk factors influence disease progression:
- Nonproliferative Diabetic Retinopathy (NPDR): Early stage in which blood vessels in the retina weaken, bulge (microaneurysms), and may leak fluid or blood. NPDR can range from mild to severe, depending on the amount of leakage and swelling.
- Proliferative Diabetic Retinopathy (PDR): Advanced stage where new, abnormal blood vessels proliferate on the retina or into the vitreous. These vessels are fragile and prone to bleeding. Scar tissue from new vessel growth can cause retinal detachment or severe vision loss.
- Macular Edema: Fluid leaking into the macula (the central portion of the retina critical for detailed vision) can cause the macula to swell, leading to central vision loss. Macular edema can occur at any stage but is a crucial cause of vision problems in diabetes.
Complications of Diabetic Retinopathy
Unmanaged diabetic retinopathy, especially when multiple risk factors are present, may lead to severe complications:
- Vitreous hemorrhage: Bleeding into the clear gel (vitreous) inside the eye, causing sudden vision loss or floaters.
- Retinal detachment: Scar tissue pulls the retina away from the back of the eye, leading to partial or total vision loss.
- Glaucoma: New blood vessels block the fluid drainage system of the eye, raising pressure and damaging the optic nerve.
- Blindness: When retinopathy, macular edema, and glaucoma are left unchecked, complete and irreversible blindness can occur.
Reducing Your Risk: Prevention and Management
Many risks for diabetic retinopathy can be modified with careful lifestyle choices and medical management. Here are proven strategies to reduce your risk:
- Monitor and Control Blood Sugar: The single most important step—use medications, diet, and exercise to keep glucose levels as close to target as possible.
- Manage Blood Pressure and Cholesterol: Take blood pressure and lipid-lowering medication if prescribed, and adopt a heart-healthy lifestyle.
- Schedule Regular Eye Exams: Annual comprehensive dilated eye exams can detect early signs of retinopathy, allowing for timely treatment.
- Quit Smoking: Avoiding tobacco is essential for vascular health and can slow or prevent progression of retinopathy.
- Maintain a Healthy Weight: Weight loss improves insulin sensitivity, blood sugar, blood pressure, and lipids.
- Exercise Regularly: Physical activity helps control blood sugar, blood pressure, and cholesterol.
- Follow Medical Advice During Pregnancy: Women with diabetes should work closely with their healthcare providers during pregnancy, as additional monitoring may be necessary.
Why Screening Is Essential
Regular eye exams are the cornerstone of diabetic retinopathy prevention. Because the earliest changes in the retina rarely cause symptoms, only a dilated retinal examination can detect retinopathy before it threatens vision.
- Early detection and treatment through laser therapy, medications, or surgery can prevent or minimize vision loss.
- Experts recommend at least annual eye exams for everyone with diabetes, and more frequent visits if retinopathy or risk factors are present.
Frequently Asked Questions (FAQs)
What are the first symptoms of diabetic retinopathy?
Most people do not notice symptoms during the early stages. Blurred vision, dark spots, or sudden vision changes may appear as the disease progresses. Regular eye exams are crucial because retinal damage often develops silently.
Can lifestyle changes really reduce my risk?
Yes, managing blood sugar, blood pressure, cholesterol, controlling body weight, and quitting smoking can all meaningfully reduce your risk and the rate of progression of diabetic retinopathy.
Is diabetic retinopathy reversible?
In the earliest stages, some changes can be halted or slowed with rigorous blood sugar management, but established structural damage to the retina is not reversible. Ongoing care can prevent further deterioration.
Does everyone with diabetes develop retinopathy?
Not everyone, but the risk increases with duration of diabetes. Proactive management can delay or prevent development of retinopathy for many individuals.
How often should I have eye exams if I have diabetes?
Most experts advise annual comprehensive eye exams for all people with diabetes. Those with signs of retinopathy or high-risk features may be asked to visit more frequently for monitoring.
Takeaway
Diabetic retinopathy is a common and serious complication of diabetes, but many of its risk factors are controllable. Understanding your risks and taking active steps—especially with regular eye monitoring—offers the best chance to preserve your vision and overall health.
References
- https://www.mayoclinic.org/diseases-conditions/diabetic-retinopathy/symptoms-causes/syc-20371611
- http://www.kadrmaseyecare.com/eye-health–care-blog/who-is-at-risk-of-diabetic-eye-disease-and-diabetic-retinopathy
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/diabetic-retinopathy
- https://my.clevelandclinic.org/health/diseases/8591-diabetic-retinopathy
- https://www.healthline.com/health/type-2-diabetes/retinopathy
- https://www.news-medical.net/health/Diabetic-Retinopathy-Risk-Factors.aspx
Read full bio of Sneha Tete












