Right-Sided Heart Failure: Symptoms, Causes, and Modern Treatment Approaches
Understand the symptoms, causes, diagnosis, and evolving management of right-sided heart failure, including lifestyle, medical, and surgical options.
Right-sided heart failure is a complex cardiac condition affecting the right ventricle’s ability to effectively circulate blood to the lungs, resulting in systemic symptoms and a broad impact on patient well-being. This guide explores the hallmark signs, underlying causes, diagnostic strategies, treatment options, lifestyle adaptations, and answers to common questions for individuals facing or seeking to understand right-sided heart failure.
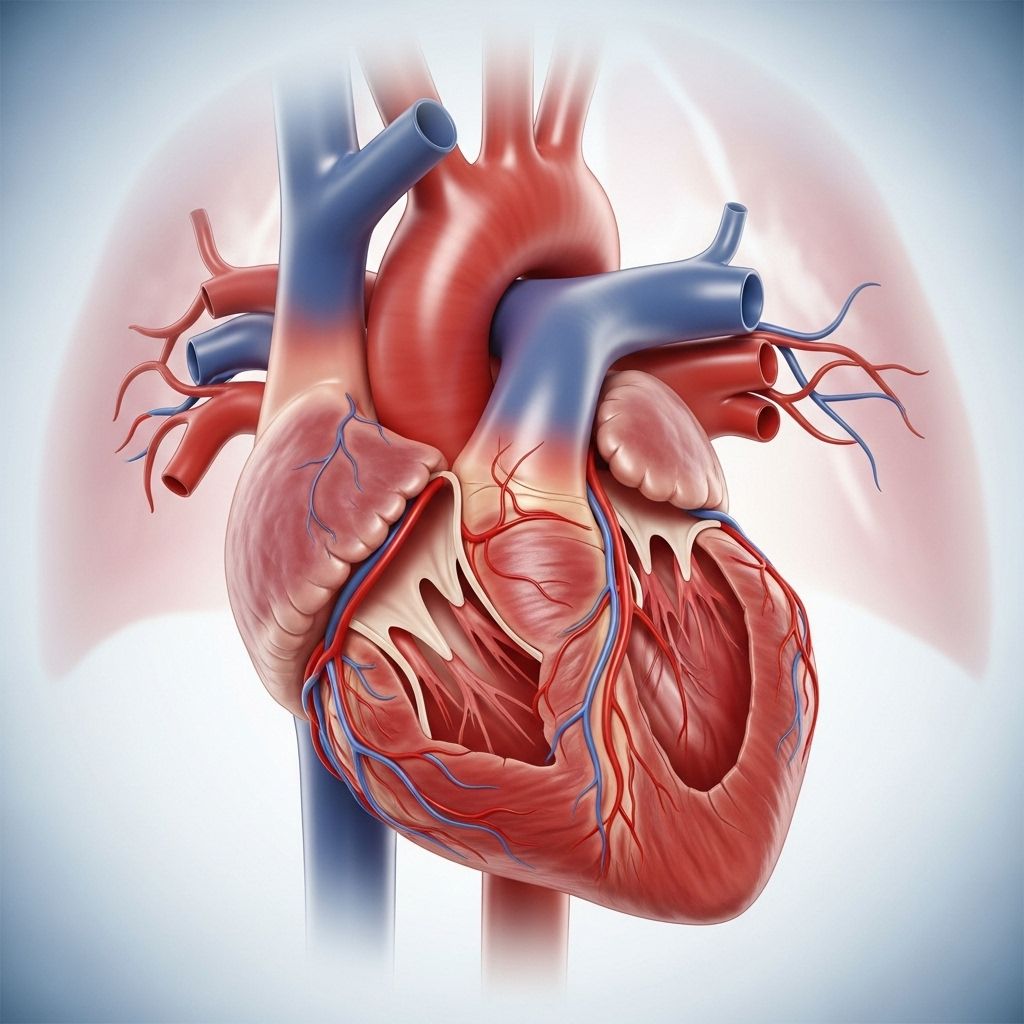
What Is Right-Sided Heart Failure?
Right-sided heart failure, sometimes called right ventricular failure, refers to the inability of the heart’s right side to pump blood efficiently to the lungs. This leads to a build-up of blood in the veins, causing fluid to leak into surrounding tissues and resulting in swelling (edema), particularly in the legs, ankles, and abdomen. Right-sided heart failure may be acute (develops suddenly) or chronic (develops gradually over time) and frequently co-occurs with left-sided heart failure.
What Are the Symptoms of Right-Sided Heart Failure?
Right-sided heart failure causes a variety of symptoms primarily associated with fluid overload and impaired cardiac output. Early recognition of these symptoms can facilitate prompt diagnosis and management.
- Swelling (edema) in the lower extremities (feet, ankles, calves) and, in severe cases, the abdomen (ascites)
- Shortness of breath (particularly when lying flat or during exertion)
- Coughing
- Dizziness, confusion, or difficulty concentrating
- Fatigue and low energy
- Sudden, unexplained weight gain (from fluid retention)
- Reduced appetite or feeling unusually full; nausea or upset stomach
- Frequent urination at night
- Bloating or abdominal discomfort
Left-Sided Heart Failure Symptoms for Comparison
- Shortness of breath (dyspnea)
- Chronic cough
- Difficulty breathing during physical activity
- Episodes of breathlessness at night (paroxysmal nocturnal dyspnea)
What Causes Right-Sided Heart Failure?
Several medical conditions can precipitate right-sided heart failure either by direct damage to the right ventricle or by forcing it to work harder than normal. Understanding these causes is crucial for management.
- Left-sided heart failure: The most common cause; failure of the left side increases pressure in the lungs, overworking the right side.
- Pulmonary hypertension: High pressure in the arteries of the lungs increases workload on the right heart.
- Lung diseases (e.g., chronic obstructive pulmonary disease, pulmonary embolism): Obstructs blood flow, leading to right heart strain.
- Valve diseases: Malfunction of tricuspid or pulmonary valves can cause regurgitation or stenosis, both stressing the right ventricle.
- Congenital heart defects: Structural abnormalities can impair blood flow through the right side.
- Heart attack (myocardial infarction): Especially in the right coronary artery, can directly damage the right ventricle.
- Obstructive sleep apnea: Can contribute to increased pulmonary artery pressure.
- Other chronic conditions: Hypertension, obesity, some cancers (and their treatments), and certain infections can also play a role.
Key Risk Factors
- Advanced age (natural weakening of the heart)
- Family history of heart disease
- Unhealthy lifestyle: smoking, excessive alcohol consumption, poor diet
- Medical illnesses: hypertension, diabetes, obesity, chronic kidney disease
How Is Right-Sided Heart Failure Diagnosed?
Diagnosis is established through a combination of physical examination, patient history, laboratory tests, and imaging studies. Early and accurate diagnosis is vital for effective treatment.
- Physical exam: Noting swelling, jugular venous distention (bulging neck veins), and listening for abnormal heart and lung sounds.
- Blood tests: Checking for signs of kidney or liver dysfunction, and measuring natriuretic peptides (BNP or NT-proBNP) released by a strained heart.
- Electrocardiogram (ECG/EKG): Identifies rhythm disturbances or patterns of strain.
- Echocardiogram: Uses sound waves to visualize cardiac anatomy and function, essential for assessing the right ventricle and valves.
- Chest X-ray: Reveals heart enlargement or fluid in the lungs and pleural space.
- Cardiac MRI or CT: Advanced imaging for detailed anatomical information in complex cases.
- Right heart catheterization: Provides direct measurements of pressures in the right chambers and pulmonary arteries.
Current Treatment Options for Right-Sided Heart Failure
Treatment plans for right-sided heart failure are customized according to the underlying cause, severity, and the patient’s overall health. Treatment aims to reduce symptoms, correct or stabilize heart function, and prevent disease progression.
Medications
- Diuretics: Promote removal of excess fluid and sodium, reducing swelling and congestion. Potassium-sparing types (e.g., spironolactone) are sometimes used to prevent low potassium.
- Vasodilators: Relax blood vessels, reducing the heart’s workload. Examples include ACE inhibitors and angiotensin receptor blockers (ARBs).
- Beta-blockers: Slow the heart rate and reduce its workload.
- Digoxin: Increases the force of the heart’s contraction, valuable in advanced cases.
- Pulmonary vasodilators: Target high blood pressure in the lungs (for pulmonary hypertension), lessening strain on the right ventricle.
- Other supportive medications: Anticoagulants (if clot risk is present), statins (to manage cholesterol), and others as needed.
Lifestyle Measures
- Smoking cessation: Avoid all tobacco products.
- Healthy weight maintenance: Use a home scale to monitor for sudden weight gain (possible fluid overload).
- Low-sodium, balanced diet: Minimizes fluid retention.
- Fluid restriction: Under physician guidance, especially in severe cases.
- Physical activity: Engage in regular, doctor-approved exercise or cardiac rehabilitation.
- Alcohol moderation: Reduce or eliminate intake to avoid further cardiac stress.
Devices and Surgical Interventions
- Implanted cardiac devices: For severe heart failure, technologies like ventricular assist devices (VADs) can help the heart pump blood.
- Total artificial heart: Rarely, replaces both ventricles in end-stage heart disease.
- Valve repair or replacement: Surgery to correct defective heart valves may be necessary if valvular disease is the primary problem.
- Correction of congenital heart defects: Where present, surgical procedures may restore better blood flow.
- Heart transplantation: In end-stage cases unresponsive to other therapies.
Self-Care and Home Management
Empowering patients with education and practical strategies is vital for controlling right-sided heart failure and maintaining quality of life.
- Daily monitoring: Weigh yourself each morning before eating or drinking. Rapid weight gain may signal fluid retention.
- Symptom diary: Record swelling, breathing changes, appetite, and energy levels.
- Adherence: Take medications exactly as prescribed and attend all follow-up appointments.
- Nutrition: Avoid excess salt and highly processed foods. Eat smaller, frequent meals if you experience bloating.
- Support: Join patient groups, cardiac rehabilitation programs, or seek counseling for emotional challenges.
- Emergency action plan: Know when and how to seek urgent help (see warning signs below).
Potential Complications of Right-Sided Heart Failure
- Progressive edema leading to skin breakdown or infections
- Impaired kidney and liver function
- Malnutrition or unintentional weight loss (cardiac cachexia)
- Arrhythmias (irregular heartbeats)
- Severe breathlessness and activity limitations
- Hospitalizations for decompensated heart failure
When to Seek Emergency Medical Care
- Sudden, severe shortness of breath or chest pain
- Fainting or severe dizziness
- New or rapidly worsening swelling in the face, hands, abdomen, or legs
- Coughing up pink or frothy sputum
- Rapid or irregular heartbeat not relieved by usual measures
Frequently Asked Questions (FAQs) About Right-Sided Heart Failure
What is the difference between right-sided and left-sided heart failure?
Right-sided heart failure primarily affects the blood returning from the body to the heart, often resulting in swelling in the legs and abdomen. Left-sided heart failure involves the ventricle that pumps blood out to the body and most often leads to fluid buildup in the lungs (pulmonary congestion).
Can right-sided heart failure be reversed?
Depending on its underlying cause and how advanced it is, right-sided heart failure may be stabilized or, in some cases, improved. For instance, managing a leaky heart valve or treating pulmonary hypertension can relieve right heart strain. However, in chronic or severe cases, ongoing management is the primary goal.
How can I reduce my risk of right-sided heart failure?
- Treat and manage high blood pressure, diabetes, and other chronic conditions.
- Avoid tobacco and excess alcohol.
- Maintain a healthy weight and exercise regularly.
- Seek timely treatment for lung diseases or valve problems.
Is exercise safe for people with right-sided heart failure?
Regular physical activity, supervised by a cardiac rehabilitation specialist, is encouraged for most people to improve stamina and overall health. Activities should be paced carefully to avoid overexertion and should always be approved by a healthcare professional.
What does sudden weight gain mean in right-sided heart failure?
Rapid weight gain (more than 2–3 pounds in 24 hours or 5 pounds in a week) may signal fluid retention and an impending “heart failure flare.” It is important to notify your healthcare team quickly so medication adjustments or medical evaluation can be undertaken.
Summary Table: Key Aspects of Right-Sided Heart Failure
| Aspect | Right-Sided Heart Failure | Left-Sided Heart Failure |
|---|---|---|
| Main Effect | Swelling of legs, ankles, abdomen (systemic congestion) | Lung congestion, shortness of breath (pulmonary congestion) |
| Primary Symptoms | Edema, weight gain, enlarged liver | Shortness of breath, cough, fatigue |
| Primary Causes | Left-sided heart failure, lung diseases, valve disease, pulmonary hypertension | Coronary artery disease, hypertension, valve disorders |
| Treatment Approach | Medications, lifestyle changes, device support/surgery if needed | Medications, lifestyle changes, device support/surgery if needed |
Additional Resources
- Consult your cardiologist or primary care provider regularly.
- Ask about cardiac rehabilitation programs in your area.
- Visit reputable resources, such as the American Heart Association, for ongoing updates and patient education materials.
References
- https://www.healthline.com/health/heart-failure/right-sided-heart-failure
- https://www.baptisthealth.com/care-services/conditions-treatments/rightsided-heart-failure
- https://www.ahajournals.org/doi/10.1161/cir.0000000000000560
- https://www.webmd.com/heart-disease/heart-failure/right-sided-heart-failure
- https://www.nhlbi.nih.gov/health/heart-failure/treatment
- https://www.mayoclinic.org/diseases-conditions/heart-failure/symptoms-causes/syc-20373142
- https://www.ncbi.nlm.nih.gov/books/NBK459381/
- https://my.clevelandclinic.org/health/diseases/17069-heart-failure-understanding-heart-failure
- https://medlineplus.gov/heartfailure.html
Read full bio of Sneha Tete












