Rheumatic Heart Disease: Causes, Symptoms, Treatment, and Prevention
Explore the origins, symptoms, complications, and modern management strategies for rheumatic heart disease.
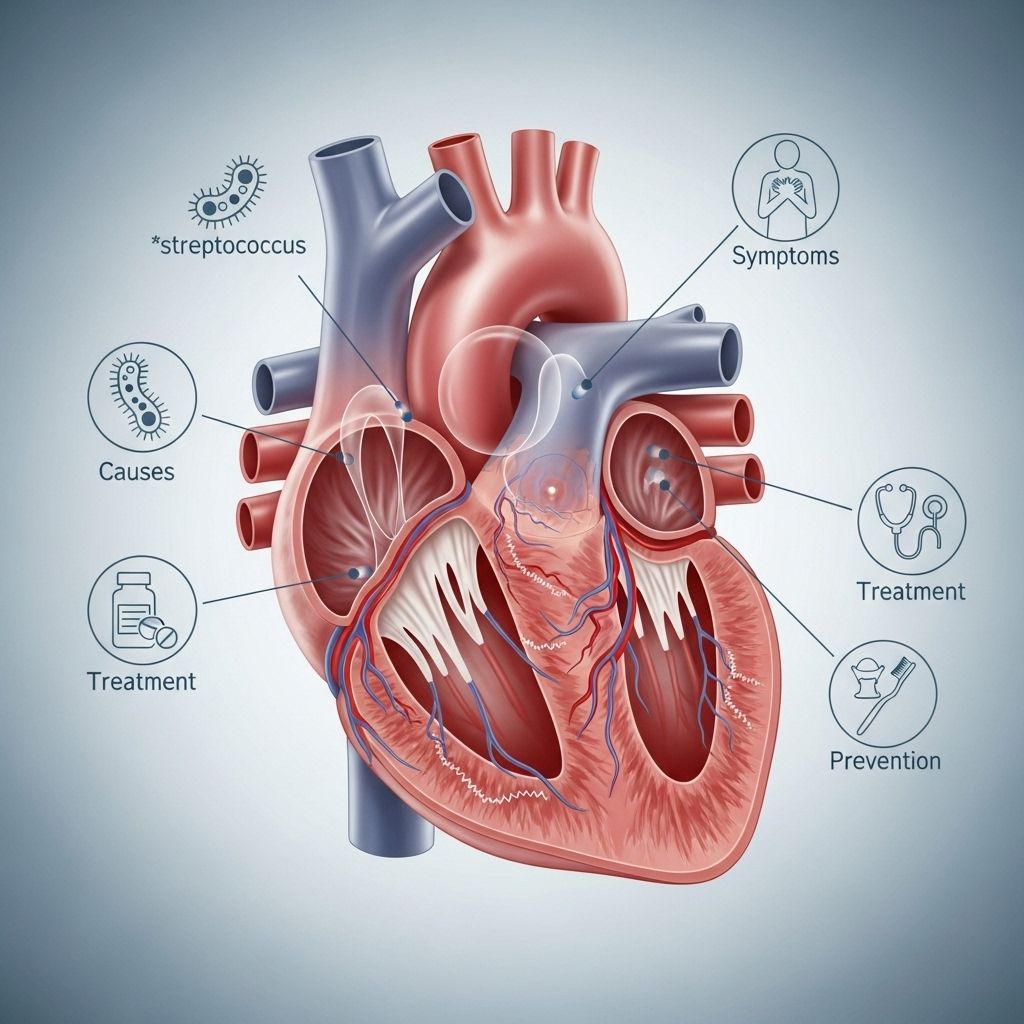
Rheumatic heart disease (RHD) is a chronic condition arising from permanent damage to the heart valves caused by one or more episodes of rheumatic fever, an inflammatory complication that follows an untreated or poorly managed group A streptococcal (GAS) throat infection. This article provides an in-depth exploration of RHD, covering its origins, symptoms, risk factors, prevention, diagnosis, treatment, possible complications, and long-term outlook.
What is Rheumatic Heart Disease?
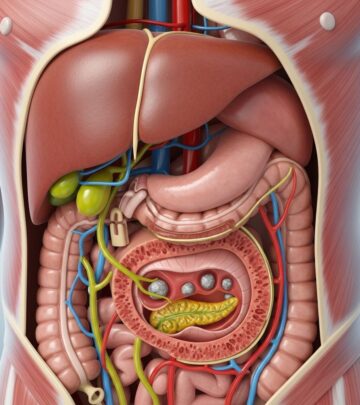
Rheumatic heart disease refers to the lasting injury to the heart’s valves following acute episodes of rheumatic fever. Rheumatic fever is itself a delayed autoimmune reaction that can occur following a sore throat or, less commonly, a scarlet fever infection caused by group A Streptococcus bacteria. The inflammation related to rheumatic fever most commonly injures the mitral valve, but may affect the aortic, tricuspid, or, rarely, pulmonary valves as well.
- RHD typically develops gradually, typically many years after the initial infection, as a result of cumulative or repeated damage to the heart’s structures.
- Valve damage leads to impaired blood flow, resulting in symptoms such as fatigue, shortness of breath, or even heart failure.
- RHD remains a significant cause of cardiovascular morbidity and mortality in children and young adults, particularly in low- and middle-income countries.
How Does Rheumatic Heart Disease Develop?
Rheumatic heart disease is the end result of a sequence of events:
- Pharyngitis: A child or young person develops strep throat due to group A Streptococcus infection.
- Acute Rheumatic Fever (ARF): If the sore throat is not promptly or fully treated, the body’s immune response may trigger inflammation affecting the joints, skin, heart, and occasionally the brain.
- Heart Valve Damage: The inflammation from rheumatic fever can cause scarring and permanent distortion or fusion of the heart valves’ cusps and supporting structures. This may narrow (stenosis) or make the valves leaky (regurgitation).
- Progressive Valve Dysfunction: Over time, repeated episodes and ongoing inflammation can worsen the valve dysfunction, eventually leading to the signs and symptoms of RHD.
What Causes Rheumatic Heart Disease?
- Group A Streptococcal Infection: Initial and repeat infections with Streptococcus pyogenes are the root cause.
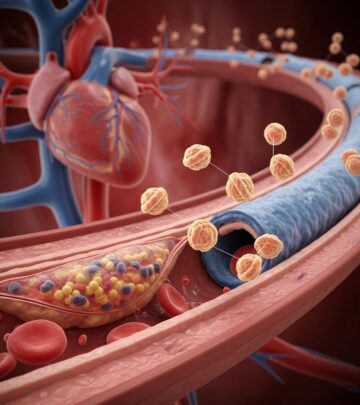
- Autoimmune Reaction: The body’s immune response to the bacteria mistakenly targets the body’s own tissues, particularly the heart valves.
- Repeated Acute Rheumatic Fever Episodes: Multiple flare-ups heighten the risk and extent of irreversible heart valve injury.
Who is at Risk?
Rheumatic heart disease can affect anyone, but certain factors increase vulnerability:
- Children aged 5–15 are most commonly affected, especially in areas with limited healthcare resources.
- People with a history of untreated, recurrent strep throat infections.
- Socioeconomic factors:
- Overcrowding and poor living conditions increase the spread of strep throat.
- Lack of access to healthcare and antibiotics means strep throat often goes untreated.
- Higher prevalence in certain regions: Asia, Sub-Saharan Africa, Pacific Islands, and Indigenous populations in Australia and New Zealand.
Symptoms of Rheumatic Heart Disease
The manifestations of rheumatic heart disease typically relate to the damaged heart valves and potential heart failure. Symptoms can develop shortly after active rheumatic fever or many years later, depending on the severity of valve damage.
- Shortness of breath, especially during physical activity or when lying down
- Fatigue and decreased ability to exercise
- Chest pain or discomfort
- Swelling of the ankles, feet, legs, abdomen, or neck veins
- Heart palpitations or an irregular heartbeat
- Occasionally, fainting, dizziness, or sudden weight gain due to fluid buildup
In some cases, especially early on, there may be no symptoms. This silent progression makes regular screening and follow-up important for at-risk individuals.
Symptoms of Acute Rheumatic Fever
- Painful or swollen joints (most common in knees, ankles, wrists, elbows)
- Fever
- Red, raised skin rash (erythema marginatum)
- Unusual, jerky movements (Sydenham’s chorea)
- Small, painless bumps under the skin (subcutaneous nodules)
- Heart inflammation (carditis), presenting with chest pain, shortness of breath, or even heart failure in severe cases
Complications of Rheumatic Heart Disease
Complications arise from ongoing damage to heart valves and the resulting cardiac dysfunction. These may include:
- Heart failure: Due to the heart’s inability to pump blood effectively, leading to fluid buildup and shortness of breath.
- Arrhythmias: Abnormal heart rhythms, such as atrial fibrillation, increasing stroke risk.
- Infective endocarditis: Infection of the damaged heart valves, a life-threatening complication.
- Stroke: Caused by blood clots forming in the heart and traveling to the brain, especially if atrial fibrillation is present.
- Pulmonary hypertension: High blood pressure in the lungs as a result of backward pressure from left heart valve disease.
How is Rheumatic Heart Disease Diagnosed?
Diagnosis is based on a combination of medical history, examination, and heart imaging tests to detect valve abnormalities and check for heart failure or arrhythmias.
| Diagnostic Method | Purpose |
|---|---|
| Echocardiogram (heart ultrasound) | Primary tool to visualize heart valve structure and function, measure severity of valve stenosis or regurgitation, and detect heart failure. |
| Electrocardiogram (ECG) | Records electrical activity for arrhythmias (irregular heartbeat). |
| Chest X-ray | Checks for heart enlargement or fluid in the lungs. |
| Blood tests | May show markers of inflammation or identify strep antibodies indicating prior infection. |
| Physical examination | May detect heart murmurs from valve damage and signs of heart failure. |
How is Rheumatic Heart Disease Treated?
While the valve damage in RHD is permanent, effective treatments can relieve symptoms, prevent further valve injury, and reduce complications:
1. Medications
- Antibiotics: Long-term (often monthly) penicillin injections prevent recurrent strep infections and further episodes of rheumatic fever.
- Medications for heart failure: Diuretics (to reduce fluid buildup), ACE inhibitors, beta-blockers, or other specialized heart medicines as needed.
- Anticoagulants (blood thinners): Used if atrial fibrillation occurs or after some valve surgeries to reduce risk of stroke.
2. Surgery or Interventional Procedures
- Valve repair or replacement: Surgical intervention may be required for severe valve stenosis or regurgitation that does not respond to medications.
- Percutaneous balloon valvuloplasty: A minimally invasive procedure used mainly for mitral stenosis.
3. Ongoing Care and Monitoring
- Regular follow-up with a cardiologist to monitor valve function and symptoms.
- Good dental hygiene to prevent heart valve infection (endocarditis).
- Vaccinations against influenza and pneumococcus to reduce infections that strain the heart.
- Antenatal care for women of childbearing age, as pregnancy can put extra stress on the heart.
Prevention: The Key Approach
Prevention remains the most effective measure against rheumatic heart disease.
Primary Prevention (Preventing Rheumatic Fever)
- Prompt antibiotic treatment of strep throat: Consult a healthcare provider if a child has sore throat with fever and treat confirmed strep infections with penicillin or other appropriate antibiotics.
- Public health measures in communities, such as improving housing, reducing overcrowding, and better access to healthcare, reduce the incidence of strep infections.
Secondary Prevention (Preventing Recurrence in Those with Previous Rheumatic Fever)
- Long-term antibiotic prophylaxis (regular intramuscular penicillin shots) to prevent repeat attacks of rheumatic fever and limit progressive valve damage.
- Regular check-ups and close monitoring.
Tertiary Prevention (Preventing Complications in RHD Patients)
- Early recognition and management of arrhythmias, heart failure, and other complications.
- Lifelong medical care and timely surgical intervention when needed.
Long-Term Outlook and Prognosis
The prognosis for RHD patients varies based on:
- Age at diagnosis
- Severity of heart valve involvement
- Access to regular medical care, antibiotics, and surgical services (if needed)
With appropriate and continuous care, many patients lead long, productive lives. However, in resource-poor settings, lack of early intervention and treatment often leads to serious disability or premature death from heart failure or stroke.
Frequently Asked Questions (FAQs) on Rheumatic Heart Disease
What is the difference between rheumatic fever and rheumatic heart disease?
Rheumatic fever is an inflammatory disease triggered by a group A streptococcal infection (like strep throat) and may affect joints, skin, brain, and heart. Rheumatic heart disease is the chronic, permanent valve damage that develops after rheumatic fever episodes.
Can adults get rheumatic heart disease?
Yes, though most cases start in childhood, adults can experience symptoms or complications of RHD later in life, especially if they had undiagnosed or untreated rheumatic fever in youth.
Is rheumatic heart disease preventable?
Most cases can be prevented by early recognition and antibiotic treatment of strep throat and by giving long-term antibiotics to those with a history of rheumatic fever.
Can rheumatic heart disease be cured?
There is no cure for existing valve damage, but symptoms can be managed and progression prevented with the right long-term medical care and strategies.
What are the lifelong needs for someone with rheumatic heart disease?
- Lifelong antibiotic prophylaxis in most patients to prevent further attacks.
- Regular heart assessments and medical follow-up.
- Good oral hygiene and infection prevention.
- Possible surgical interventions for severe valve disease.
Key Points to Remember
- Rheumatic heart disease is a serious, chronic complication of untreated or recurrent rheumatic fever.
- Heart valve damage is irreversible, but complications are preventable with early care.
- Prompt treatment of strep throat and long-acting antibiotics for those with prior rheumatic fever are crucial to reduce new cases of RHD.
- Global efforts continue to focus on improving standards of living, access to healthcare, and awareness in affected communities.
References
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/rheumatic-heart-disease
- https://www.who.int/news-room/fact-sheets/detail/rheumatic-heart-disease
- https://www.ncbi.nlm.nih.gov/books/NBK538286/
- https://www.medstarhealth.org/services/rheumatic-heart-disease
- https://stanfordhealthcare.org/medical-conditions/blood-heart-circulation/rheumatic-heart-disease/treatments.html
- https://world-heart-federation.org/what-we-do/rheumatic-heart-disease/
- https://my.clevelandclinic.org/health/diseases/21485-rheumatic-heart-disease
- https://www.mayoclinic.org/diseases-conditions/rheumatic-fever/symptoms-causes/syc-20354588
- https://www.ucsfbenioffchildrens.org/conditions/rheumatic-heart-disease
Read full bio of Sneha Tete