Rheumatic Heart Disease: Causes, Symptoms, Treatment, and Prevention
Learn about rheumatic heart disease, its symptoms, causes, treatments, and preventive strategies for heart health.
Rheumatic Heart Disease: Understanding Causes, Risks, and Care
Rheumatic heart disease (RHD) is a serious condition resulting from damage to the heart valves, stemming from one or more episodes of acute rheumatic fever caused by an abnormal immune response to a Streptococcus pyogenes (group A streptococcus) infection. RHD remains a leading cause of acquired heart disease, particularly in children and young adults in developing countries. Its impact can be life-long, making awareness, early detection, and proper management crucial for individuals and healthcare providers alike.
What is Rheumatic Heart Disease?
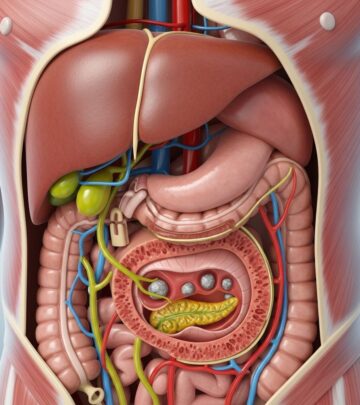
Rheumatic heart disease refers to permanent damage of the heart valves that follows repeated or severe attacks of acute rheumatic fever, itself a sequela of inadequately treated strep throat or scarlet fever. This condition can develop years after an initial infection and often involves the mitral or aortic valves, although any heart valve can be affected. The disease is characterized by progressive scarring and deformity of the valves that can eventually lead to heart failure and other complications.
How RHD Develops
- Initial infection: Usually starts with a strep throat caused by group A streptococcus.
- If left untreated, the body’s immune response can attack not just the bacteria but also tissues, notably the heart, joints, skin, and brain.
- Acute Rheumatic Fever: A systemic inflammatory condition developing about 2–3 weeks after the original infection.
- Over time and across repeated attacks, this can result in chronic and progressive valve damage.
Risk Factors and Causes
The main cause of rheumatic heart disease is an abnormal immune response to an infection with group A beta-hemolytic streptococcus (the most common agent in strep throat). Several risk factors increase a person’s susceptibility to RHD:
- Untreated or inadequately treated strep throat or scarlet fever infections
- Repeated infections: Multiple episodes increase risk of chronic heart valve injury
- Age: Most commonly affects children between 5 and 15 years old, but adults can be affected as well
- Socioeconomic factors: Overcrowded living conditions, poor access to medical care, and poverty
- Genetics and family history: Certain individuals may be more prone due to genetic predispositions
Symptoms of Rheumatic Heart Disease
Symptoms of RHD can vary widely depending on:
- The stage of the disease
- The heart valves affected
- The degree of valve damage
Common symptoms may include:
- Shortness of breath
- Chest pain
- Fatigue, especially with exertion
- Swelling in the abdomen, legs, ankles, or feet (edema)
- Heart palpitations or irregular heartbeats
- Heart murmur (detectable by a physician on examination)
- Fainting or dizziness (in severe cases)
Children may display additional symptoms during rheumatic fever:
- Fever
- Painful, swollen joints
- Rash with pink rings and a clear center (erythema marginatum)
- Jerky, involuntary body movements (Sydenham chorea)
- Small, painless nodules under the skin
Diagnosis: How is Rheumatic Heart Disease Identified?
Early, accurate diagnosis of RHD is critical to guide treatment and prevent further damage. Healthcare providers use a combination of clinical examination, laboratory tests, and imaging studies:
- History & Physical Exam: Listen for heart murmurs or rubs, check for joint swelling, skin rashes.
- Throat cultures/Blood tests: Identify streptococcal infection and markers of inflammation.
- Echocardiogram (ultrasound of the heart): Gold standard for diagnosing valve damage and assessing severity.
- Electrocardiogram (ECG/EKG): Analyzes heart rhythm and electrical activity for signs of strain or abnormal conduction.
- Chest X-ray: Evaluates heart enlargement and possible fluid in the lungs.
- Cardiac MRI (if required): Offers highly detailed visualization of heart structure.
Diagnosis is based on the modified Jones criteria for acute rheumatic fever, and observation of persistent or progressive heart valve damage is key for RHD diagnosis.
Complications of Rheumatic Heart Disease
RHD can cause significant, life-threatening complications if not managed promptly and effectively:
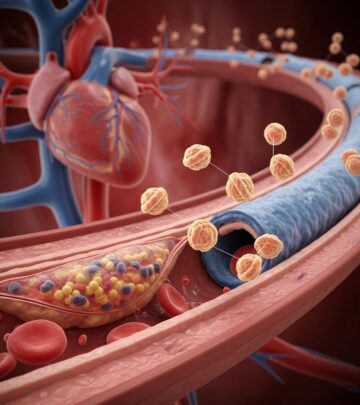
- Heart failure: Poor blood flow due to malfunctioning valves leads to fluid buildup and decreased oxygen delivery.
- Arrhythmias: Especially atrial fibrillation, increasing stroke risk.
- Infective endocarditis: Infected or damaged valves are more susceptible to serious bacterial infections.
- Stroke: Due to increased risk of blood clots caused by irregular heartbeats or pooling blood in an enlarged heart chamber.
- Pulmonary hypertension: High blood pressure in lung arteries resulting from poorly functioning left-sided heart valves.
Pathophysiology: Why Does RHD Happen?
The heart’s valves (usually mitral and aortic) are most frequently damaged through a type II hypersensitivity reaction:
- Immune system forms antibodies targeting strep bacteria, but these also mistakenly attack proteins in heart tissue due to molecular mimicry.
- This autoimmune process triggers inflammation and the formation of Aschoff nodules in the myocardium, eventually resulting in scarring, thickening, and fusion of the heart valve leaflets.
- With repeated or severe attacks, the valve damage becomes permanent, causing either valve narrowing (stenosis) or leaking (regurgitation or insufficiency).
These changes alter normal blood flow through the heart and may ultimately compromise cardiac efficiency and oxygen delivery throughout the body.
Treatment Options for Rheumatic Heart Disease
Management of RHD focuses on preventing further damage, controlling symptoms, and treating or preventing complications.
Prevention
Primary prevention: Early and aggressive treatment of strep throat infections is the first line of defense.
- Antibiotics: Most commonly, penicillin or amoxicillin. For allergy, alternatives like cephalexin (unless allergic) or macrolides may be used.
Secondary prevention: For those with a history of acute rheumatic fever or evidence of RHD, long-term antibiotic prophylaxis (usually benzathine penicillin G injections every 3-4 weeks) is recommended to prevent recurrence.
Medical Management
- Anti-inflammatory medications: Such as aspirin or corticosteroids to reduce acute inflammation during active rheumatic fever.
- Medications for heart failure: Beta-blockers, ACE inhibitors, diuretics, or digoxin to relieve symptoms and reduce strain on the heart.
- Anti-arrhythmics: For rhythm irregularities like atrial fibrillation.
- Anticoagulants: To lower stroke risk in patients with atrial fibrillation or severe valve disease.
Surgical and Interventional Options
- Valve repair: Surgical reshaping or reconstruction of damaged valves.
- Valve replacement: With artificial (mechanical or tissue) valves in severe cases.
Patients who undergo valve replacement may require lifelong anticoagulation or additional medications and long-term follow-up for optimal outcomes.
Prognosis and Long-term Outlook
The outlook for individuals with RHD depends on the severity and extent of heart valve damage, the speed and effectiveness of treatment, and access to ongoing care. Key factors influencing prognosis include:
- Early diagnosis and treatment: Timely management of strep throat and acute rheumatic fever dramatically lowers the chance of severe RHD.
- Access to healthcare: Socioeconomic status, community health infrastructure, and education about disease are closely linked to long-term outcomes.
- Adherence to secondary prophylaxis: Prevents recurrence and additional damage.
- Effective management of complications and lifestyle modifications can improve quality of life and reduce hospitalizations.
Prevention Strategies and Global Perspective
Global strategies reflect the need for both social and medical interventions:
- Primordial prevention: Reduce poverty, overcrowding, and poor living conditions that enhance the spread of group A streptococcus.
- Primary prevention: Increase awareness and provide prompt antibiotic treatment for sore throats, especially in children.
- Secondary prevention: Long-term antibiotics for those with prior acute rheumatic fever or RHD.
- Vaccination: Research is ongoing into vaccines for group A streptococcus, which may someday reduce the disease burden.
- Regular monitoring and education: Patients and communities should engage in regular health evaluations and learn about the importance of medication adherence and recognizing early symptoms.
Living with Rheumatic Heart Disease
- Ongoing medical and sometimes surgical care is necessary to manage symptoms and limit progression.
- Regular follow-ups with a cardiologist or heart team are essential.
- Living a heart-healthy lifestyle—avoiding tobacco, maintaining a balanced diet, exercising as tolerated, and taking prescribed medicines—help reduce risks.
- Women with RHD who plan pregnancy should seek counseling, as pregnancy may increase cardiac risks depending on disease severity.
Frequently Asked Questions (FAQs)
What is the main cause of rheumatic heart disease?
RHD is primarily caused by damage to the heart valves resulting from an abnormal immune response to a group A streptococcal infection, commonly strep throat.
Who is at greatest risk for developing RHD?
Children ages 5–15 in developing countries, people with limited access to healthcare, and those living in overcrowded or impoverished conditions are at the highest risk.
Is rheumatic heart disease contagious?
Rheumatic heart disease itself is not contagious, but group A strep infections are, so preventing transmission of strep is crucial for prevention.
How is RHD treated?
Treatment varies depending on disease severity, ranging from antibiotics and medications for heart symptoms to surgical valve repair or replacement in advanced cases. Lifelong preventive antibiotics may be needed to reduce recurrence risk.
Can RHD be prevented?
Yes. The most important preventive step is prompt, effective treatment of strep throat in children and adults to stop rheumatic fever and thus RHD from developing.
What are the complications of untreated RHD?
Untreated RHD can lead to chronic heart failure, stroke, atrial fibrillation, and increased risk of infective endocarditis and premature death.
What is the long-term outlook for people with RHD?
With early diagnosis, effective treatment, and appropriate long-term care, many people with RHD can live healthy lives. Severe or unrecognized cases may result in disability or shortened lifespan.
How can communities help reduce RHD?
Communities play a vital role through public health education, improving living conditions, ensuring access to healthcare, and supporting vaccination and early treatment programs for strep throat.
References
- https://www.youtube.com/watch?v=nvRIbmXMVKY
- https://www.hopkinsrheumatology.org/rdrcc/
- https://www.ncbi.nlm.nih.gov/books/NBK538286/
- https://www.hopkinsguides.com/hopkins/view/Johns_Hopkins_ABX_Guide/540006/all/Acute_Rheumatic_Fever
- https://www.heart.org/en/news/2024/08/23/how-the-war-against-rheumatic-heart-disease-was-and-wasnt-won
- https://pure.johnshopkins.edu/en/publications/generating-global-priority-for-addressing-rheumatic-heart-disease
- https://www.hopkinsarthritis.org/arthritis-info/rheumatoid-arthritis/
Read full bio of medha deb